Sudden Vision Loss
Last updated August 20, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.


Overview
Sudden vision loss means your sight drops quickly—over seconds, minutes, or a few days. It can affect one eye or both. This is an emergency. Getting help right away can protect your sight and, in some cases, your overall health.
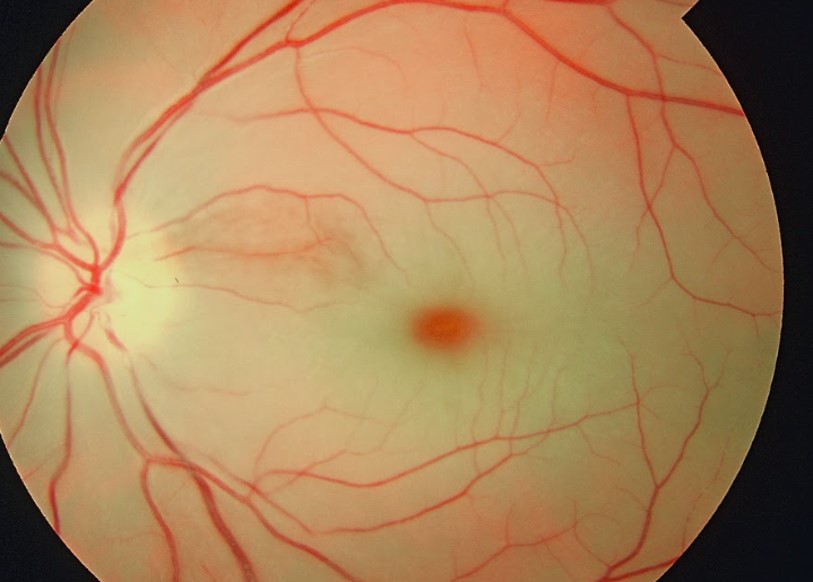
Common causes include problems with the retina (the light-sensing layer in the back of the eye), the optic nerve, or high pressure in the eye. Examples include eye stroke (central retinal artery occlusion), retinal detachment, optic neuritis, and acute angle-closure glaucoma.
If your vision suddenly changes, seek urgent care now. Sudden vision loss can be painless or painful—either way, do not wait to see if it gets better on its own. Call your eye doctor, go to urgent care or an emergency department, or dial emergency services if you also have weakness, trouble speaking, or a severe headache.
Why speed matters: early treatment for some causes—like retinal detachment surgery or fast stroke evaluation for an eye artery blockage—can save vision.
Learn more: Cleveland Clinic explains that sudden vision loss is a medical emergency 1, and the National Eye Institute notes that retinal detachment requires immediate care to prevent permanent vision loss 2.
Symptoms
Symptoms can help point to the cause. Tell your clinician exactly what you notice and when it started.
- “Curtain” or shadow coming over part of your vision with new flashes or many floaters — may suggest a retinal tear or detachment (usually painless, urgent). 3
- Severe eye pain, redness, halos around lights, headache, nausea — can signal acute angle-closure glaucoma and needs immediate treatment. 4
- Sudden, profound, painless loss of vision in one eye — could be an ocular stroke (central retinal artery occlusion); use a stroke pathway urgently.
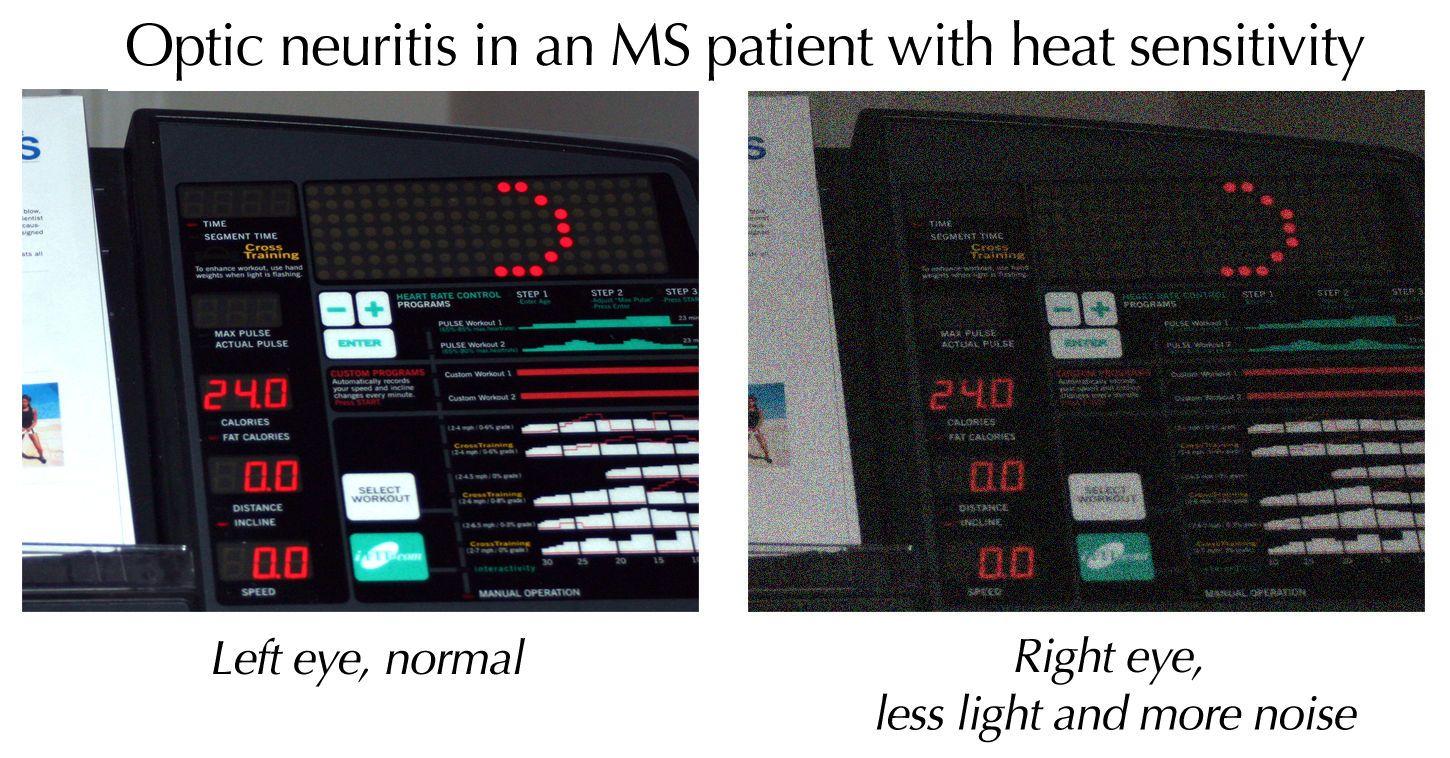
- Eye-movement pain with vision dimming or color washout — may point to optic neuritis (inflammation of the optic nerve).
Other clues include double vision, new blind spots, or flashes of light. Note if symptoms are constant or come and go, and if they affect one or both eyes.
Causes and Risk Factors
Sudden vision loss can come from different parts of the visual system.
- Retina problems: Retinal detachment (the retina peels away), retinal tears, or bleeding into the eye (vitreous hemorrhage). Risk rises with aging, severe nearsightedness, eye trauma, or prior eye surgery.
- Ocular stroke (CRAO): Blocks blood flow to the retina and causes painless, sudden vision loss; treated like an ischemic stroke and needs rapid triage. 5
- Optic nerve issues: Optic neuritis (often painful eye movements and color vision changes) and ischemic optic neuropathy (can be linked to giant cell arteritis in adults over 50).
- High eye pressure: Acute angle-closure glaucoma causes rapid pressure spikes and vision loss with pain, halos, and nausea; certain eye shapes, age, and some medicines can increase risk.
Systemic risks like high blood pressure, diabetes, atrial fibrillation, and carotid artery disease raise the chances of ocular stroke or other serious eye events. Guidelines emphasize quick recognition and referral because delays can lead to permanent vision loss. 6
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
Your evaluation starts with a focused history (exact timing, pain, trauma, other symptoms) and an eye exam. Typical steps may include:
- Vision and pupil checks, visual fields, and pressure measurement.
- Dilated eye exam to look for retinal tears, detachment, bleeding, or artery/vein blockages. 2
- Imaging such as optical coherence tomography (OCT) or ocular ultrasound when the view is cloudy, to identify detachment or hemorrhage.
- Stroke pathway for suspected CRAO: urgent emergency department evaluation with brain/vascular imaging and cardiac studies.
- Targeted labs (e.g., ESR/CRP) and sometimes temporal artery biopsy if giant cell arteritis is suspected in adults over 50 with new headache, jaw pain, scalp tenderness, or tender temples. 8
Tell your clinician about medicines (including decongestants or anticholinergics), prior eye surgery, recent trauma, or systemic symptoms (weakness, trouble speaking, chest pain).
Treatment and Management
Treatment depends on the cause and often must start quickly:
- Retinal detachment/tear: Laser, freezing (cryopexy), or surgery to seal tears and reattach the retina—best done urgently to preserve sight.
- Ocular stroke (CRAO): Immediate emergency department care through a stroke protocol; rapid triage and medical management aim to save vision and prevent future strokes.
- Optic neuritis: Often treated with high-dose steroids to speed recovery when vision is significantly affected or features are atypical; many people recover much of their vision, though color/contrast changes can persist. 7
- Acute angle-closure glaucoma: Emergency pressure-lowering eye drops and medications, followed by a laser procedure (iridotomy) to create a new fluid pathway and prevent future attacks. 4
Your care team may include an ophthalmologist (sometimes a retina or glaucoma specialist), emergency clinicians, neurologists (for suspected stroke), and your primary care clinician to manage risk factors.
Living with Sudden Vision Loss and Prevention
After the emergency is addressed, focus on protecting remaining vision and preventing another event.
- Control vascular risks: Manage blood pressure, diabetes, cholesterol, and heart rhythm (such as atrial fibrillation) with your primary care team to reduce the chance of ocular and brain strokes. 6
- Know GCA warning signs (age ≥50): New severe headache, jaw pain with chewing, scalp tenderness, or tender temples with vision change—seek urgent care; quick steroid treatment can prevent blindness. 8
- Eye protection: Wear safety glasses during sports or yard/house work to reduce trauma-related tears or detachments.
- Follow-up: Keep appointments after surgery or treatment to monitor healing and prevent complications; ask which symptoms should trigger same-day care.
- Daily tips: Increase lighting, use high-contrast materials, and consider low-vision tools if residual vision is limited.
Latest Research & Developments
A scientific statement from the American Heart Association recognizes central retinal artery occlusion as an acute ischemic stroke of the eye and calls for rapid stroke-style pathways for triage and treatment. 5
Retinal detachment techniques (e.g., small-gauge vitrectomy, improved tamponade choices) and imaging (OCT, widefield imaging) help diagnose and fix problems earlier. 2
Ongoing trials are studying ways to restore blood flow in ocular stroke and to tailor steroid or immune therapies for optic neuritis.
Recently Published in Peer-Reviewed Journals
BMC ophthalmology
July 21, 2025
Orbital apex syndrome and ophthalmic artery occlusion caused by acute sinusitis.
Liao D, Yang X, Li R
BMC ophthalmology
July 7, 2025
Idiopathic retinal vasculitis, aneurysms, and neuroretinitis (IRVAN) syndrome: a comprehensive literature review of a rare retinal vasculopathy.
Asaad H, Hasan R
BMC ophthalmology
March 14, 2025
Optic neuritis, as unusual manifestations of hypoparathyroidism: a rare case report.
Mirmazloomi Y, Ebrahimtabar F, Mozhdehipanah H
Next Steps
If your vision just changed suddenly, treat this as an emergency. If possible, do not drive yourself. Go to the nearest emergency department or call your eye doctor’s urgent line.
Best specialist to see: a board-certified ophthalmologist (and, depending on the cause, a retina or glaucoma specialist, or a neuro-ophthalmologist). In many areas you may need a referral from urgent care, your primary clinician, or the ER. If wait times are long, ask to be placed on a cancellation list and check nearby centers. For eye strokes (CRAO) or new neurologic symptoms, ask for the hospital’s stroke team.
- Bring a list of your medicines (including decongestants or motion sickness pills).
- Note exactly when symptoms started and any headache, jaw pain, weakness, or speech trouble.
- Those details help target urgent testing and treatment. 1
You can also connect with the right specialist on Kerbside for a focused medical education consult about your condition and next steps. This educational service does not create a patient–physician relationship.
Trusted Providers for Sudden Vision Loss

Dr. Emily Eton
Specialty
Retina/Vitreous
Education
Harvard Medical School

Dr. Grayson Armstrong
Specialty
Retina/Vitreous
Education
Ophthalmology

Dr. Jose Davila
Specialty
Retina/Vitreous
Education
Retina/Vitreous Surgery

Dr. Nicholas Carducci
Specialty
Retina/Vitreous
Education
University of Pennsylvania Perelman School of Medicine