Glaucoma
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.

Overview
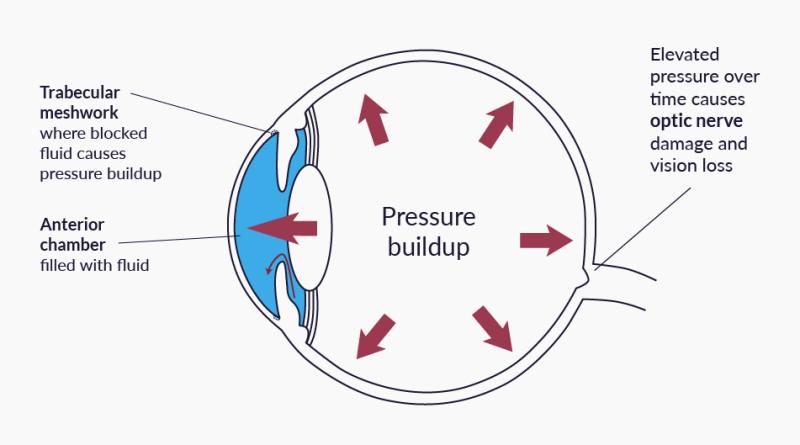
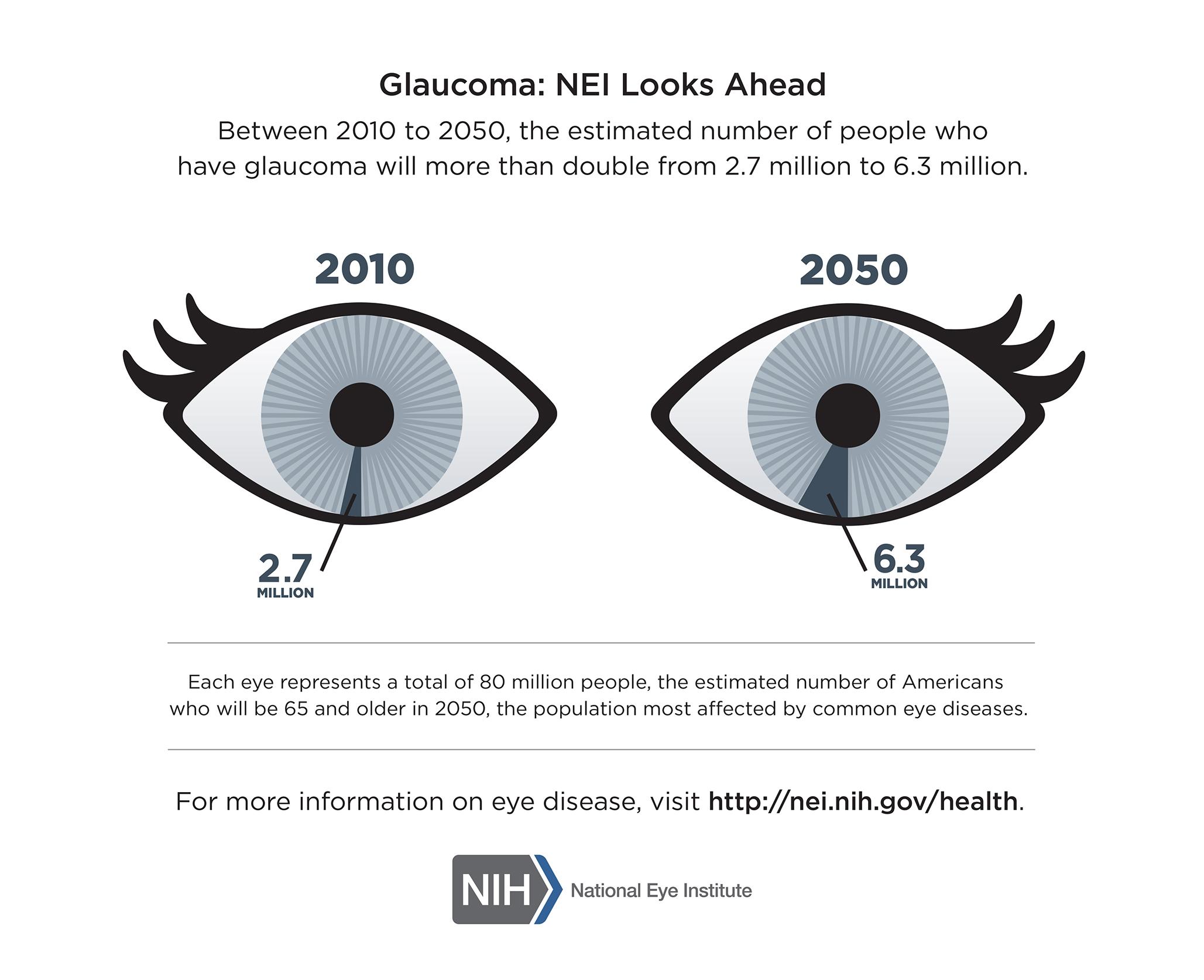
Glaucoma refers to a family of eye diseases that slowly damage the optic nerve, the “data cable” that connects each eye to the brain. Most—but not all—forms are linked to a build-up of aqueous fluid that raises intra-ocular pressure (IOP). Without treatment, the nerve fibers that carry visual information die off, leading to irreversible vision loss. Because early glaucoma is painless and your central vision stays clear, nearly half of people who have the disease do not realize it until permanent damage has occurred.1 Regular comprehensive eye exams are therefore essential; caught early, most people keep useful sight for life.2
Symptoms
Early-stage open-angle glaucoma is often called the “silent thief of sight” because it produces no noticeable symptoms at first. Side (peripheral) vision thins out slowly—too slowly for the brain to flag the change.3 As more nerve fibers are lost, untreated patients can develop tunnel vision and, eventually, total blindness.
By contrast, angle-closure glaucoma is an emergency. A sudden rise in eye pressure can trigger severe eye pain, headache, nausea, rainbow halos around lights and a visibly red eye.4 Anyone with these warning signs should seek urgent ophthalmic care.
- Normal-tension glaucoma damages the optic nerve despite average pressure—likely because of poor blood flow.
- Congenital and juvenile glaucomas appear in infants and children and need prompt surgical care.
Causes and Risk Factors
Glaucoma damage results when the optic nerve cannot tolerate the mechanical or vascular stress inside the eye. Researchers do not yet know why some nerves are more vulnerable, but the following factors raise risk:56
- Age > 40 (steep rise after 60)
- Family history of glaucoma, especially in first-degree relatives
- African, Hispanic/Latino or Asian ancestry
- Elevated IOP or thin central corneas (< 525 µm)
- Chronic steroid use, past eye injury or surgery
- Medical conditions such as diabetes, high blood pressure or migraine
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
The only reliable way to detect glaucoma early is a comprehensive dilated eye exam. Key tests include:78
- Tonometry – measures eye pressure.
- Ophthalmoscopy & OCT imaging – assess the health and thickness of the optic-nerve rim.
- Perimetry (visual-field test) – maps any blind-spot patterns.
- Pachymetry – checks corneal thickness, an important risk modifier.
- Gonioscopy – shows whether the drainage angle is open or blocked.
Adults at average risk should be screened every 1–2 years; those at high risk may need annual or more frequent exams.
Treatment and Management
Glaucoma damage can’t be reversed, but lowering IOP slows or halts further loss. Your ophthalmologist will tailor a plan that may combine the following:910
- Prescription eye drops – first-line therapy. Several drug classes (prostaglandin analogs, beta-blockers, Rho-kinase inhibitors and others) either improve out-flow or cut fluid production.11
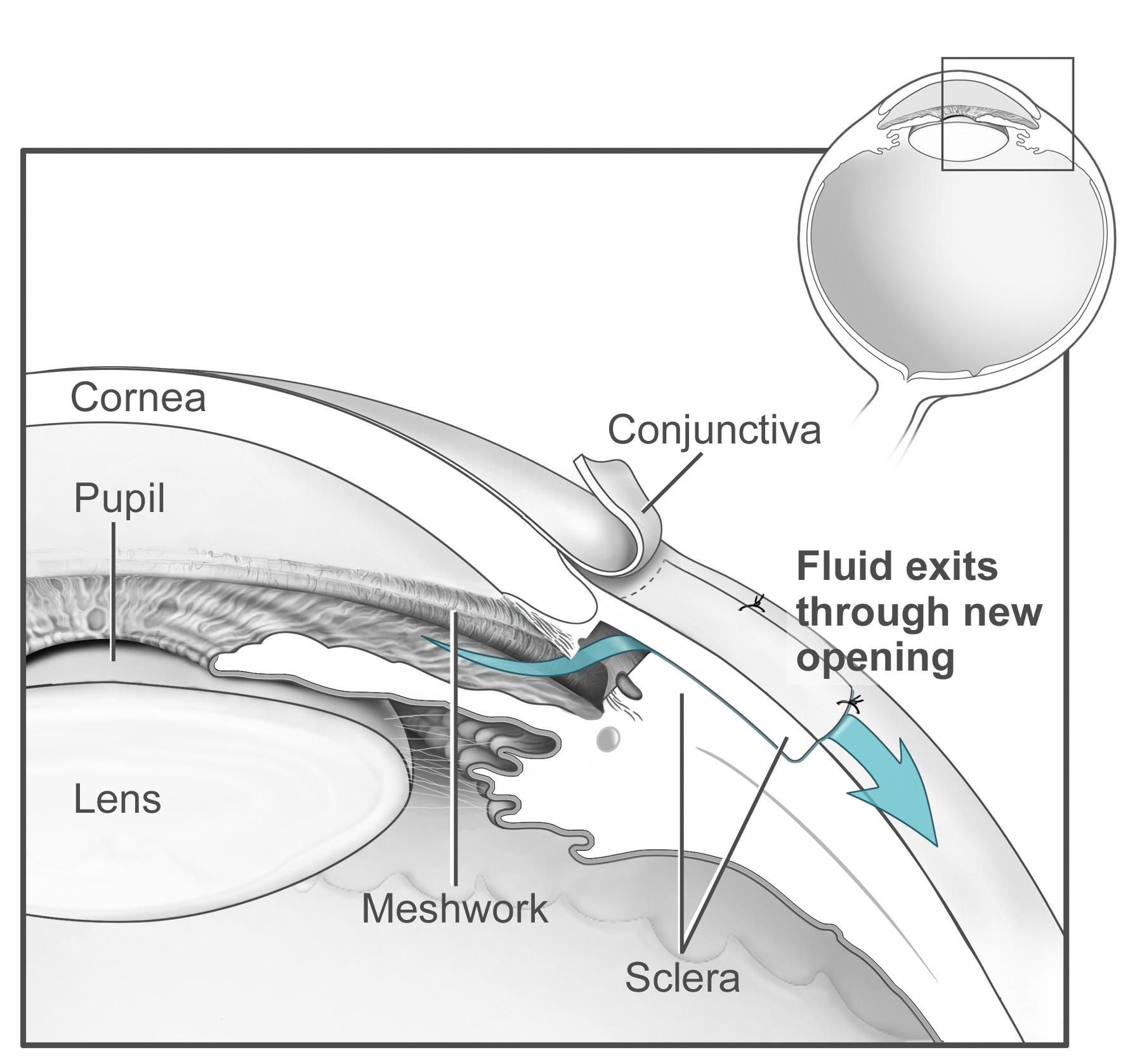
- Laser procedures – selective laser trabeculoplasty (SLT) for open-angle glaucoma, or peripheral iridotomy for angle-closure, can delay or replace drops.
- Minimally Invasive Glaucoma Surgery (MIGS) and classic filtering surgeries (trabeculectomy, tube shunts) when pressure targets are not met.
Follow-up every 3-6 months lets your doctor confirm that pressure goals remain on target and adjust therapy promptly.
Living with Glaucoma and Prevention
While glaucoma itself can’t yet be prevented, sight loss can be minimized with an active partnership in care:
- Stick with your regimen: use drops exactly as prescribed, set alarms and keep a spare bottle to avoid missed doses.12
- Protect your eyes: wear sports goggles and safety glasses during high-risk activities.
- Exercise safely: moderate aerobic exercise can lower IOP, but avoid inverted yoga poses that raise it—ask your doctor for guidance.
- Manage systemic health: control blood pressure, cholesterol and blood sugar.
- Family matters: encourage first-degree relatives to schedule baseline dilated exams, as early detection is key.
Latest Research & Developments
Innovation is rapidly reshaping glaucoma care:
- Sustained-release implants: The FDA approved iDose TR in 2024, a tiny anchor-like device that delivers travoprost inside the eye for up to 3 years, reducing or eliminating daily drops.13
- Durysta® bimatoprost implant—the first biodegradable intracameral implant—continues to show pressure-lowering benefits beyond 24 months in real-world studies.14
- Neuro-protective strategies: Early-phase trials of gene therapy and nicotinamide supplementation aim to shield retinal ganglion cells from death.15
- First-line laser therapy: Recent multi-center data suggest SLT may control pressure better than drops alone over five years, with fewer side-effects.16
Recently Published in Peer-Reviewed Journals
Ophthalmology. Glaucoma
July 26, 2025
Selective Laser Trabeculoplasty and the Evolving Glaucoma Paradigm.
Realini T, Gazzard G
American journal of ophthalmology
July 24, 2025
Safety and Efficacy of Omidenepag Isopropyl for Elevated Intraocular Pressure: A Systematic Review and Meta-Analysis.
Sharma S, Singh R, Balas M, et al.
Ophthalmology. Glaucoma
July 24, 2025
Intraocular Pressure Fluctuations Recorded by a Telemetric Sensor After Nonpenetrating Glaucoma Surgery in Primary Open-Angle Glaucoma.
Englisch CN, Trouvain A, Wakili P, et al.
Next Steps
If you have risk factors—or were just diagnosed—the smartest move is to book a full evaluation with a glaucoma specialist (an ophthalmologist who completed fellowship training in glaucoma).
How to get there:
- Ask your primary-care doctor or optometrist for a referral, or self-refer to a specialty clinic (permitted in many regions).
- Verify that the doctor is an ophthalmologist (MD/DO) rather than an optometrist; only ophthalmologists perform laser or surgical treatments.17
- Check availability: high-demand practices may book out weeks, so call early and mention any rapid vision loss or pain.
- Gather your records: prior eye-pressure readings, medication lists, and visual-field printouts speed the visit.
Ready to act? You can connect directly with our network of fellowship-trained glaucoma specialists below for second opinions, personalized treatment planning or ongoing management.18


