Open-Angle Glaucoma
also known as Primary Open-Angle Glaucoma, POAG
Last updated July 26, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.


Overview
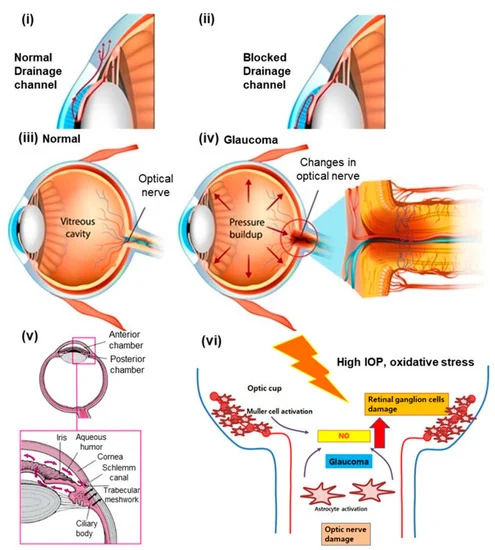
Primary open-angle glaucoma (POAG) is the most common form of glaucoma worldwide. It occurs when the eye’s drainage angle remains physically open, yet microscopic changes inside the trabecular meshwork slow aqueous outflow, leading to chronically elevated intraocular pressure (IOP) and progressive, irreversible optic-nerve damage.1 Globally, POAG affects an estimated 64 million adults, a number projected to exceed 111 million by 2040.2 Because vision loss creeps in painlessly and peripherally, POAG is often dubbed the “silent thief of sight.” Early detection through regular dilated eye examinations is crucial to preserving vision.
Symptoms
Most people with open-angle glaucoma experience no noticeable symptoms until significant peripheral vision has been lost.3 As the disease advances, patients may bump into objects off to the side, miss letters when reading, or struggle with low-contrast tasks such as night driving.4 Because central vision remains intact until late stages, many individuals are unaware of any problem. Once optic-nerve fibers are lost, the resulting visual-field defects are permanent; POAG-related blindness is preventable only through timely diagnosis and treatment.
Causes and Risk Factors
- Elevated IOP (>21 mmHg): the single most modifiable risk factor.
- Age > 60 years (or >40 years for individuals of African ancestry).5
- Family history: first-degree relatives confer a 4- to 9-fold risk.6
- Thin central corneal thickness (≤ 510 µm).
- Race/ethnicity: African, Afro-Caribbean and Hispanic individuals develop POAG earlier and more severely.
- Systemic conditions: diabetes, hypertension, obstructive sleep apnea, and long-term corticosteroid use increase risk.
POAG is multifactorial. Researchers believe oxidative stress, genetic variants (e.g., MYOC, OPTN) and vascular dysregulation all contribute to trabecular meshwork failure and optic-nerve susceptibility.
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
Diagnosis combines structural and functional testing:
- Tonometry: Goldmann applanation remains the gold standard for IOP measurement.
- Gonioscopy: confirms an open anterior chamber angle.7
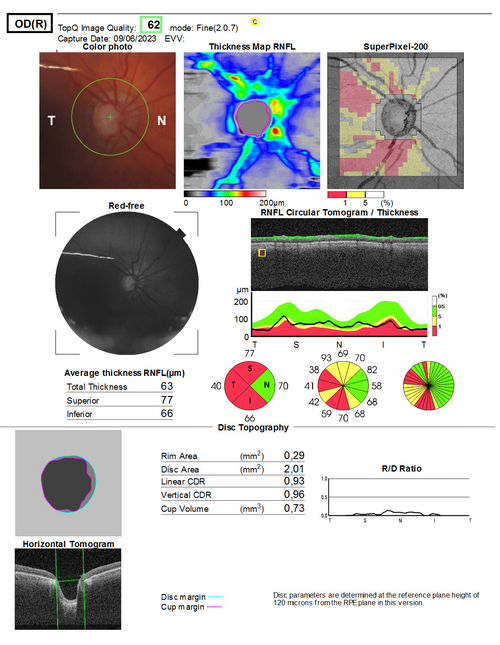
- Optic-nerve evaluation: slit-lamp biomicroscopy and optical coherence tomography (OCT) reveal neuro-retinal-rim thinning, cup-to-disc enlargement, and retinal-nerve-fiber-layer loss.
- Standard automated perimetry (SAP): detects characteristic arcuate visual-field defects.
- Pachymetry: measures corneal thickness, an essential element of modern POAG risk calculators.
Because POAG is often asymptomatic, the American Academy of Ophthalmology recommends comprehensive eye exams every 1–2 years after age 40 and annually after 65.8
Treatment and Management
The goal of therapy is to lower IOP to a level that halts optic-nerve damage. Typical steps include:
- Topical medications: prostaglandin analogs, beta-blockers, carbonic-anhydrase inhibitors, alpha-agonists, and ROCK inhibitors.9
- Laser trabeculoplasty (SLT): first-line or adjunctive therapy that improves aqueous outflow with minimal downtime; the LiGHT trial showed SLT can safely replace drops for many newly diagnosed patients.10
- Minimally invasive glaucoma surgery (MIGS): goniotomy, trabecular bypass stents, and canaloplasty lower IOP with faster recovery than traditional trabeculectomy.
- Trabeculectomy or tube-shunt surgery: reserved for advanced or refractory cases.
Target IOP is individualized, typically 20–40 % below baseline, and revisited at each follow-up visit.
Living with Open Angle Glaucoma and Prevention
Although POAG cannot be prevented, its impact can be minimized:
- Adhere to prescribed drops and appointment schedules.
- Learn correct instillation techniques (see image below) and use reminders or smartphone apps to improve compliance.11
- Maintain overall cardiovascular health (blood pressure, blood sugar) and avoid smoking.
- Use protective eyewear during sports to prevent secondary ocular injuries.
Low-vision services, adaptive lighting, high-contrast reading materials, and orientation-and-mobility training help patients with advanced field loss stay independent.12
Latest Research & Developments
Recent advances include:
- Early intervention: The LiGHT trial demonstrated that SLT as a first-line treatment offers IOP control comparable to drops while reducing medication burden and costs.13
- AI-assisted diagnostics: Deep-learning algorithms analyze OCT and fundus images to detect glaucoma with >90 % accuracy, potentially facilitating mass screening.14
- Neuroprotection: Laboratory studies on nicotinamide riboside, brimonidine and gene-editing approaches aim to preserve retinal ganglion cells beyond pressure reduction.
- Drug delivery: Sustained-release bimatoprost implants and refillable port-delivery systems are in late-phase clinical trials.
Recently Published in Peer-Reviewed Journals
BMC ophthalmology
July 23, 2025
Analysis of surgical outcomes and risk factors after gonioscopy-assisted transluminal trabeculotomy.
Gunay M, Turk A, Kurutas OK, et al.
Ophthalmology. Glaucoma
July 21, 2025
Outcomes in Primary Congenital Glaucoma, 2011-2023: L V Prasad Eye Institute, Hyderabad.
Mandal AK, Gothwal VK, Ali MH
Investigative ophthalmology & visual science
July 1, 2025
Glaucoma in Older Asians Aged 60 to 100 Years: Prevalence, Factors, Trends, and Projections (2024-2040).
Gupta P, Thakur S, Wong CMJ, et al.
Next Steps
Best specialist to see: a board-certified glaucoma specialist (fellowship-trained ophthalmologist) has the expertise and technology to tailor therapy and monitor progression.
How to schedule:
- Ask your primary eye-care provider or optometrist for a referral, especially if you have risk factors or suspicious findings.
- Verify that the specialist participates in your insurance plan and brings experience with advanced diagnostics (OCT, visual-field analyzers) and both laser and surgical options.
- If wait-times are long, request to be placed on a cancellation list and schedule virtual follow-ups when appropriate.
You can also directly book an appointment with our glaucoma team below; most patients are seen within two weeks. Early evaluation and individualized care dramatically reduce the risk of vision loss.1516


