Selective Laser Trabeculoplasty
also known as SLT
Last updated August 1, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.

Overview
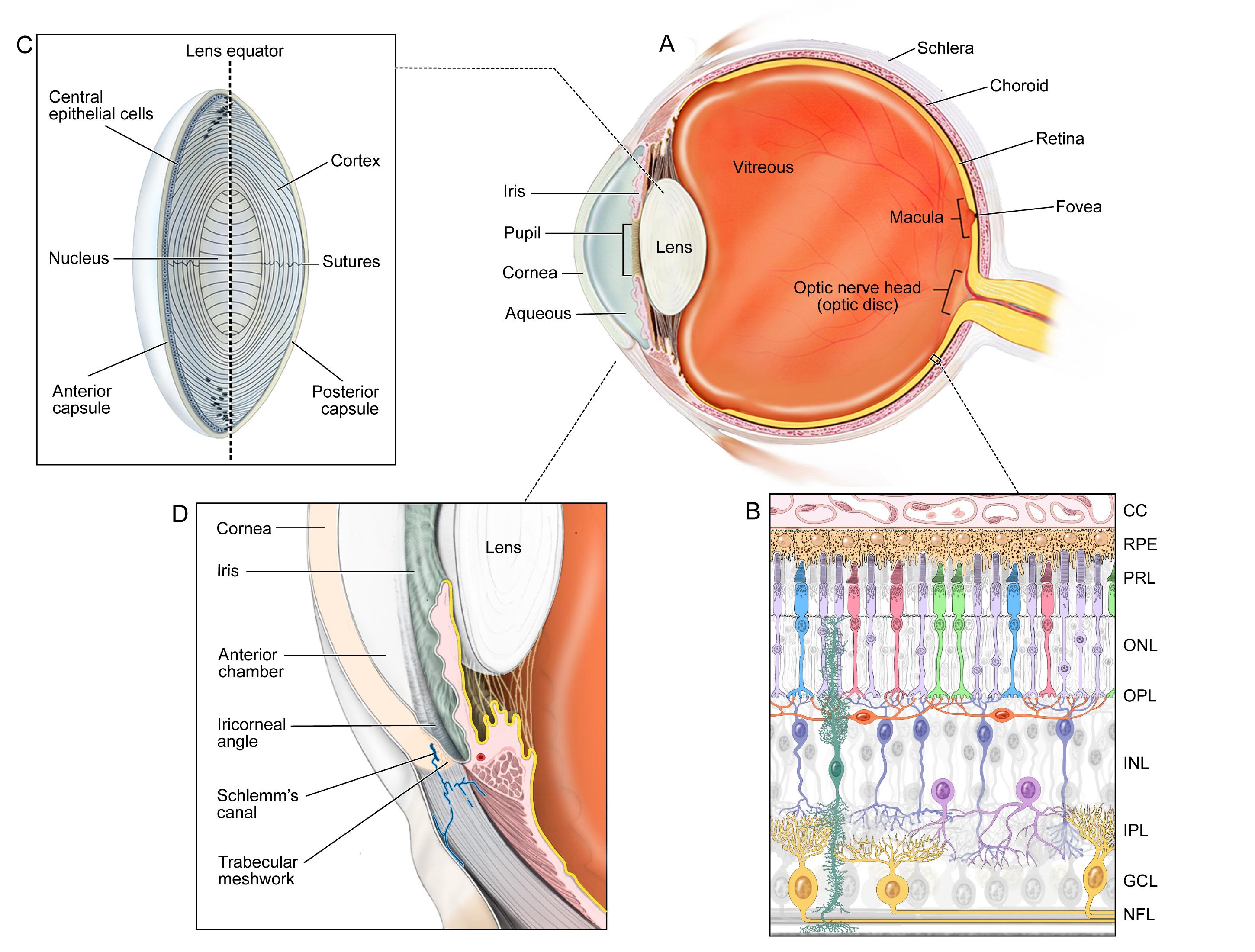
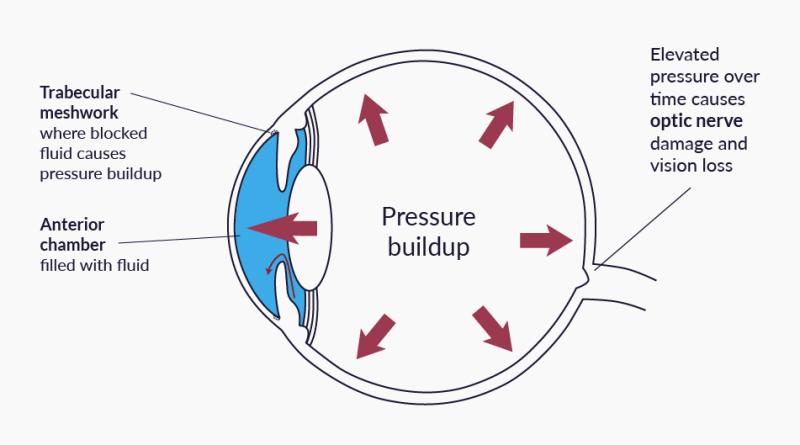
Selective Laser Trabeculoplasty (SLT) is an in‑office laser procedure that lowers the pressure inside the eye by helping fluid drain through the trabecular meshwork. It is most often used to treat open‑angle glaucoma and ocular hypertension. Unlike earlier argon‑laser techniques, SLT targets only pigmented cells, producing little thermal damage and making the procedure repeatable if pressure rises again. Many experts now consider SLT an excellent first‑line alternative to daily eye‑drop therapy because it is quick, painless, and has a long track‑record of safety.
About eight in ten people experience a 20–30 % fall in eye pressure after one treatment, and the effect typically lasts several years before gradually wearing off.12
How the Procedure Works & Options
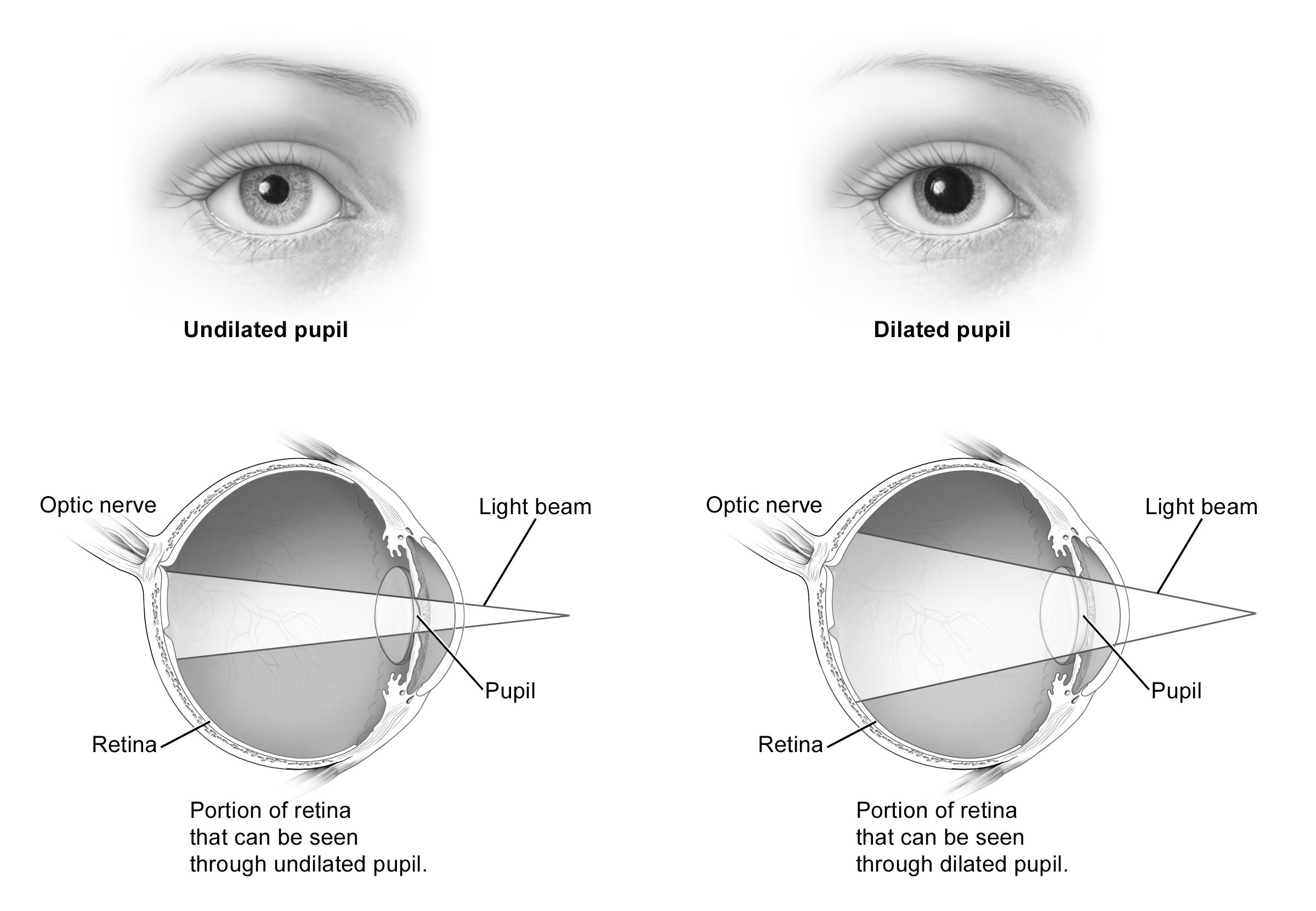
SLT uses short pulses of low‑energy, green Nd:YAG laser light delivered through a special contact lens at the slit‑lamp microscope. The laser selectively treats melanin‑rich cells lining the trabecular meshwork over 180°–360° of the angle. This triggers a gentle biological response that clears microscopic debris and remodels tissue, improving aqueous outflow and thereby lowering intra‑ocular pressure (IOP). The treatment itself takes about five to ten minutes, requires only topical anesthesia, and patients go home the same day.
Variations include 360° SLT (full angle), 180° SLT (half angle), and re‑SLT for pressure rebound. Some centers also offer Micropulse LT, an even lower‑energy protocol, though long‑term data are more limited.34
Who Is a Candidate?
Ideal candidates are adults with primary open‑angle glaucoma or ocular hypertension whose angles are visible on gonioscopy. SLT is especially attractive for people who:
- Struggle to remember, tolerate, or afford daily eye drops
- Need further IOP reduction despite maximum medical therapy
- Have pigment in the trabecular meshwork (lighter eyes may respond, but success is higher in moderately pigmented angles)
It is not recommended for eyes with active inflammation, neovascular or angle‑closure glaucoma without prior peripheral iridotomy, or significantly scarred angles. Trials dating back to the landmark NEI‑sponsored Glaucoma Laser Trial and follow‑up studies confirm that early laser therapy is as safe and effective as initial medication in many patients.56
SLT Suitability Score
Enter your details below to check your suitability for this treatment
Suitability Level
Recommendation
Benefits and Limitations
Benefits
• Lowers IOP by 20–30 % in most eyes and may delay or eliminate the need for drops.
• Quick, painless, and done in clinic without systemic anesthesia.
• Tissue‑sparing—so it can be repeated if pressure creeps back up.
Limitations
• Effect is not permanent; about half of patients need retreatment within 3–5 years.
• Works less predictably in heavily scarred or lightly pigmented angles.
• A small percentage (<5 %) experience a short‑term IOP spike, so a pressure check is done 1–2 hours post‑op.
The multicenter LiGHT randomized trial showed that first‑line SLT achieved similar vision‑related quality‑of‑life scores to medication while being more cost‑effective and reducing the need for surgery over three years.78
Risks and Side Effects
SLT has a very favorable safety profile. The most common side effects are mild eye irritation, transient light sensitivity, and temporary redness lasting 24–48 hours. A short course of anti‑inflammatory drops is usually prescribed.
Serious complications are rare but can include a post‑laser pressure spike, peripheral anterior synechiae, or, very rarely, persistent inflammation. Risk is slightly higher in eyes with markedly elevated baseline IOP or narrow angles. Long‑term damage to the trabecular meshwork is minimal compared with older argon laser trabeculoplasty, supporting retreatability.910
Recovery and Long‑Term Care
Most people resume normal activities the next day. Your doctor will:
- Check IOP 1–2 hours after treatment and again in 4–6 weeks.
- Continue or adjust any glaucoma drops while the laser effect develops.
- Schedule routine follow‑ups every 3–6 months to monitor pressure and optic‑nerve health.
If IOP rises again after several years, SLT can be safely repeated or combined with medicines, minimally invasive glaucoma surgery (MIGS), or conventional filtering surgery as needed.1112
Latest Research & Innovations
Research continues on ways to enhance laser efficacy and convenience. Newer energy‑modulation strategies such as micropulse LT aim to further reduce inflammation. Direct Selective Laser Trabeculoplasty (DSLT) uses an automated, non‑contact delivery system to treat through the limbus in seconds and is undergoing multicenter trials.
Investigators are also refining predictive models—higher baseline IOP and greater angle pigmentation correlate with a better pressure drop—and exploring biomarkers that might forecast long‑term success.1314
Recently Published in Peer-Reviewed Journals
Ophthalmology. Glaucoma
July 26, 2025
Selective Laser Trabeculoplasty and the Evolving Glaucoma Paradigm.
Realini T, Gazzard G
Ophthalmology
May 9, 2025
Randomized Noninferiority Trial of Direct Selective Laser Trabeculoplasty in Open-Angle Glaucoma and Ocular Hypertension: GLAUrious Study.
Gazzard G, Congdon N, Azuara-Blanco A, et al.
JAMA ophthalmology
April 1, 2025
Selective Laser Trabeculoplasty After Medical Treatment for Glaucoma or Ocular Hypertension.
Konstantakopoulou E, Gazzard G, Garway-Heath D, et al.
Next Steps – See a Glaucoma Specialist
If you have been told you have elevated eye pressure or glaucoma, scheduling an appointment with a glaucoma specialist is the next best step. They can determine whether SLT is right for you, explain alternatives, and design a follow‑up plan tailored to your lifestyle. You can connect with the right clinician through Kerbside and take the first step toward protecting your sight for the long term.
Bringing your medication list and recent eye‑pressure readings will help your specialist craft the safest, most effective care plan.1516


