Photophobia
also known as Light Sensitivity
Last updated August 5, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.
Overview
Photophobia literally means “fear of light,” but in medicine it describes any uncomfortable or painful sensitivity to light. The symptom can range from mild squinting on a sunny day to severe eye or head pain triggered by a smartphone screen. Photophobia is not a disease by itself—it’s a signal that something else (often in the eyes, brain, or both) needs attention. An estimated 10–30 % of routine eye-clinic visits mention light sensitivity, and prevalence rises sharply in people with migraine, traumatic brain injury (TBI), inflammatory eye disease, or albinism.1 Although most cases resolve when the underlying cause is treated, persistent or worsening photophobia should always prompt a professional evaluation to rule out infections, neurologic emergencies, or vision-threatening eye disorders.2
Symptoms
People experience photophobia in many ways. Common descriptions include:
- Sharp, stabbing, or burning eye pain when exposed to sunlight or fluorescent lamps;
- Immediate headaches or worsening migraine when looking at screens or car headlights;
- Excessive tearing, blinking, or a need to close one or both eyes;
- Feeling physically ill—nausea, dizziness, or the urge to vomit—in bright environments.
Symptoms may come on suddenly (for example, with meningitis or corneal abrasion) or build gradually, as in chronic dry eye and computer-vision syndrome.3 Because photophobia often co-exists with blurred vision, eye redness, or neurological signs, noting every associated symptom helps clinicians pinpoint the underlying condition.4
Causes and Risk Factors
Light sensitivity can originate from ocular, neurologic, systemic, or environmental factors. Key categories include:
- Ocular surface disorders – corneal abrasion, keratitis, conjunctivitis, and severe dry eye disrupt the cornea’s smooth surface.5
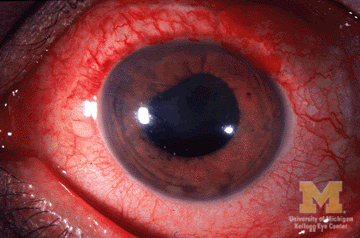
- Intra-ocular inflammation – iritis/uveitis, acute angle-closure glaucoma, or post-surgical inflammation.
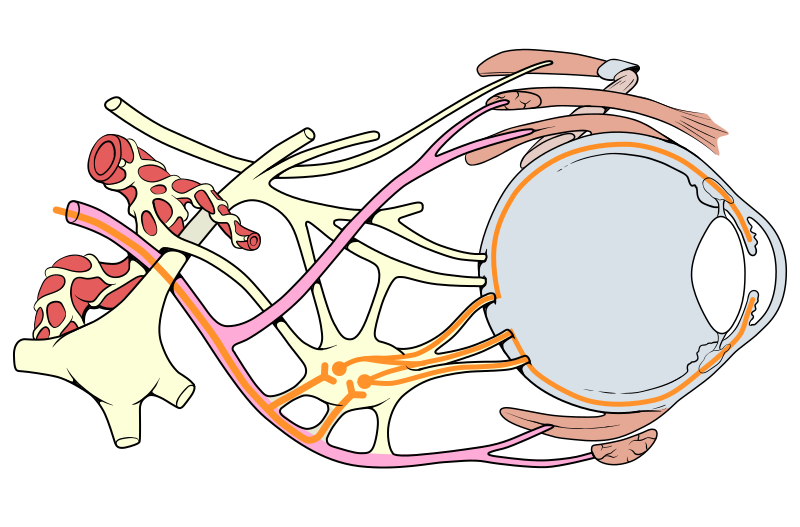
- Neurologic conditions – migraine, meningitis, subarachnoid hemorrhage, TBI, and trigeminal nerve disorders.6
- Systemic & genetic factors – albinism, aniridia, retinal dystrophies, thyroid eye disease.
- Medications & chemicals – mydriatic eye drops, anticholinergics, retinoids, some antibiotics.
- Environmental/behavioral – prolonged screen time, inadequate ambient lighting, high-contrast workstations.
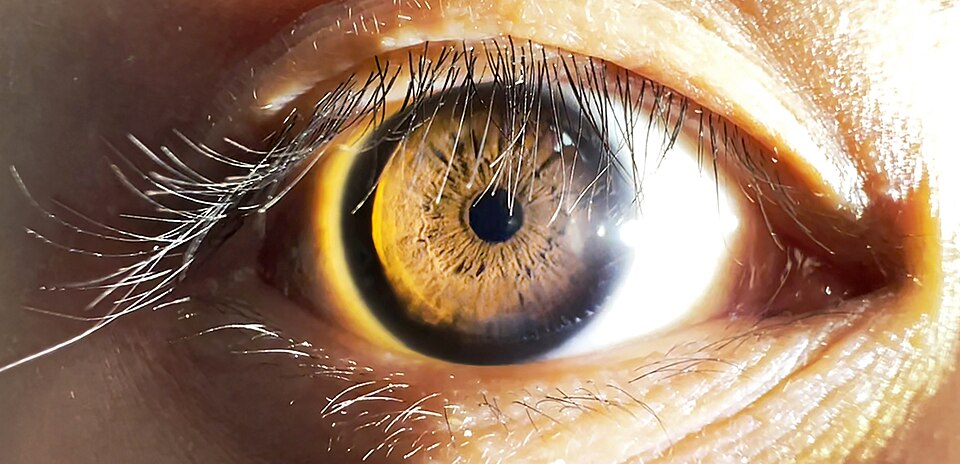
Having pale irides (light-colored eyes) slightly increases baseline sensitivity because they allow more stray light into the eye.
Photophobia Risk Estimator
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
A clinician will begin with a targeted history (onset, duration, triggers, systemic symptoms) followed by a comprehensive eye exam with slit-lamp biomicroscopy, corneal staining, intra-ocular pressure, and dilated funduscopy. If ocular findings are minimal but symptoms are severe, neurologic work-up—including cranial nerve testing, visual-field assessment, and possibly neuro-imaging—may be required.7 Lab tests or lumbar puncture are added when infection or autoimmune inflammation is suspected.8 Prompt diagnosis is critical because a corneal ulcer or meningitis can escalate within hours.
Treatment and Management
Management focuses on treating the root cause and reducing light exposure while healing occurs. Typical measures include:
- Lubricating or medicated eye drops for dry eye, allergy, or mild keratitis;
- Topical steroids or cycloplegics for uveitis;
- Antibiotics/antivirals for infectious causes;
- Triptans or CGRP inhibitors for migraine-associated photophobia;
- Protective eyewear: wrap-around sunglasses, amber lenses for screen use, or specialty tints such as FL-41 rose filters, which clinical studies show can reduce light-evoked discomfort and migraine frequency.10
Patients should avoid driving or operating machinery if sudden light exposure provokes pain or visual blackout.9
Living with Photophobia and Prevention
Daily habits help keep symptoms at bay:
- Choose matte screens and lower screen brightness; employ blue-light–filter software;
- Use brimmed hats and UV-blocking sunglasses outdoors;
- Set up work areas with indirect, warm-tone LED lighting;
- Stay hydrated and follow the 20-20-20 rule (every 20 minutes, look 20 feet away for 20 seconds) to curb digital eyestrain.11
Regular eye exams catch early corneal or retinal problems, and vaccine-preventable infections (e.g., meningococcal meningitis) should be up to date to lower sudden-onset photophobia risk.12
Latest Research & Developments
Research is clarifying the neural circuitry connecting the retina, trigeminal pathways, and thalamus—explaining why both eye and brain disorders can trigger photophobia. Functional MRI studies show that FL-41 rose-tinted lenses dampen activity in pain-processing cortical areas, reducing light-evoked unpleasantness by up to 30 %.13 A 2024 prospective case series confirmed symptom relief in chronic ocular-pain patients wearing FL-41 indoors for eight weeks.14 Parallel work on green-light–filtering “Avulux” lenses and pupillary-modulating neuro-stimulation devices is under way, holding promise for non-pharmacologic control of disabling light sensitivity.
Recently Published in Peer-Reviewed Journals
Cephalalgia : an international journal of headache
August 1, 2025
The psychometric properties of an e-headache diary in migraine.
van Veelen N, Pelzer N, van der Arend BWH, et al.
BMC ophthalmology
July 28, 2025
Endophthalmitis following inadvertent intravitreal injection of botulinum toxin: a case report and literature review.
Aljohani SM, Alharbi AS, Alhayaza RM
Cephalalgia : an international journal of headache
July 1, 2025
Characteristics of visual snow syndrome in Japan and its association with migraine.
Suzuki Y, Kiyosawa M
Next Steps
If bright light hurts or you routinely avoid well-lit settings, schedule a comprehensive exam with a neuro-ophthalmologist (or an ophthalmologist comfortable co-managing neurological eye disorders). They can coordinate imaging and collaborate with neurologists when needed. Ask your primary-care doctor for a referral, or use professional society directories; alternatively, you can connect directly with the right specialist through Kerbside to streamline the process.
Bring a log of triggers, current medications, and photos of your work environment to the visit. Early evaluation improves outcomes, especially when infections, glaucoma, or inflammatory eye disease are the culprits.1516