Thyroid Eye Disease
also known as Graves’ Orbitopathy
Last updated August 5, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.


Overview
Thyroid eye disease (TED) is an autoimmune inflammatory disorder in which antibodies that normally target the thyroid also stimulate fibroblasts in the orbit. The resulting cascade—cytokine release, glycosaminoglycan deposition and edema—causes the extra-ocular muscles and orbital fat to enlarge, pushing the eyes forward (proptosis) and affecting vision.1 TED affects about 25–50 % of people with Graves’ hyperthyroidism but can also appear in euthyroid or hypothyroid states.2 The disease has two phases: an active (inflammatory) phase that typically lasts 6–24 months, and a chronic (fibrotic) phase in which changes stabilize but may leave lasting dysfunction and disfigurement.
Symptoms
TED symptoms depend on which orbital tissues are inflamed and how far the disease has progressed, but common complaints include:
- Bulging eyes (proptosis) or a constant “staring” appearance.3
- Eyelid retraction or lag with increased scleral show.
- Dryness, redness, burning and tearing from exposure keratopathy.4
- Double vision (diplopia) due to restrictive strabismus when swollen muscles cannot move freely.
- Eye pain or pressure, especially when looking up or sideways.
- Blurry vision or color-desaturation in severe cases, signalling compressive optic neuropathy.
Symptoms often fluctuate with fatigue, smoking and thyroid-hormone swings, so keeping a symptom diary helps clinicians gauge activity.
Causes and Risk Factors
TED results from loss of immune tolerance to the thyroid-stimulating hormone receptor (TSHR) and the insulin-like growth-factor-1 receptor (IGF-1R) on orbital fibroblasts. Well-known risk factors include:
- Autoimmune thyroid disease: Graves’ hyperthyroidism is present in ≈ 90 % of TED cases.5
- Cigarette smoking, which increases both incidence and severity up to eight-fold.4
- Female sex (5 : 1 versus men) but more severe disease in men.
- Radioiodine ablation without prophylactic steroids.
- Poorly controlled thyroid hormone levels, high TSHR-antibody titers and stressful life events.
- Genetic polymorphisms in HLA-DR and CTLA-4 loci and family history of autoimmune disease.
TED Progression Risk Score
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
Diagnosis combines clinical signs with targeted testing:
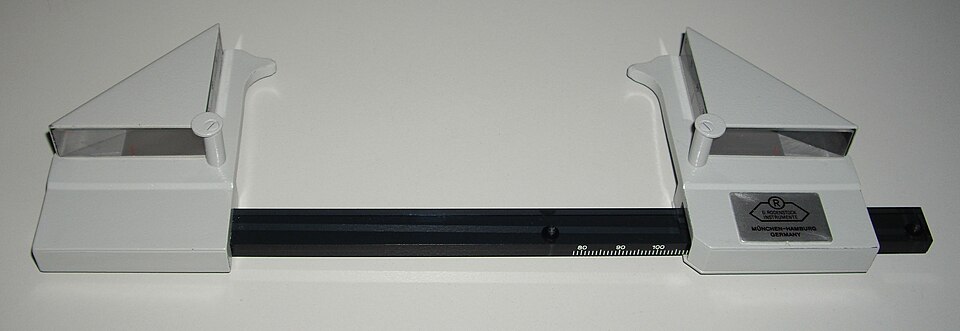
- Comprehensive eye exam measuring proptosis (Hertel exophthalmometry), lid position and ocular motility.6
- Thyroid function tests (TSH, free T4, TSHR antibodies) and systemic assessment.
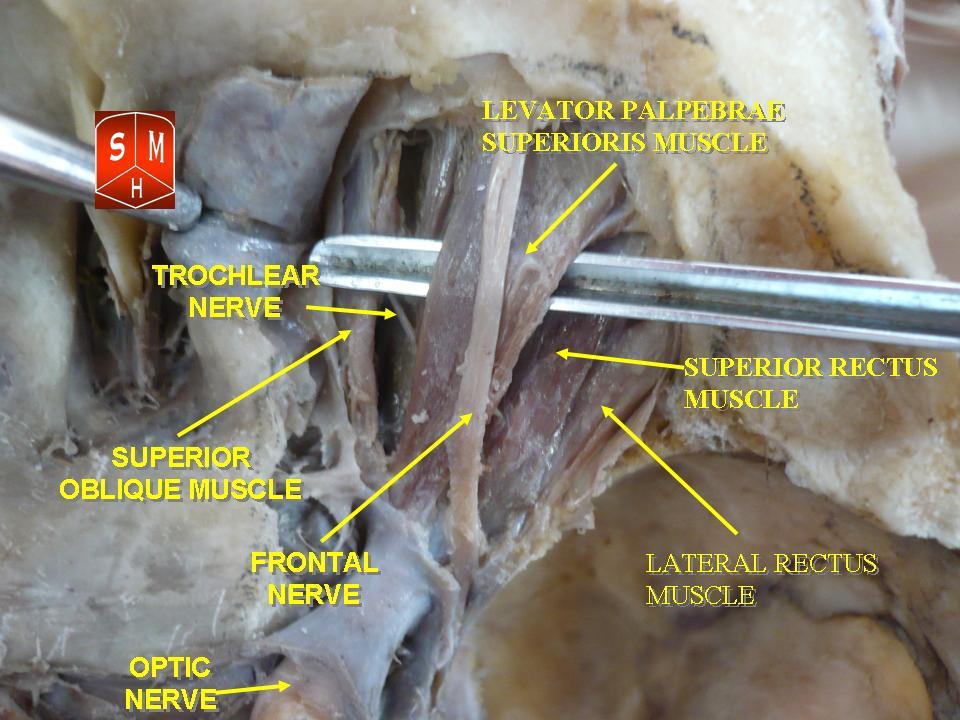
- Orbital CT or MRI shows symmetrical enlargement of extra-ocular muscle bellies with tendon sparing—the classic “Coca-Cola bottle” sign.7
- Clinical Activity Score (CAS) or EUGOGO scale rates disease activity to guide treatment.8
Urgent neuro-ophthalmology referral is required if color vision fades, visual fields constrict or CAS ≥ 4 persists despite medical therapy.
Treatment and Management
Therapy is tailored to activity (inflammatory vs. fibrotic) and severity (mild, moderate, sight-threatening):
- Optimize thyroid control (antithyroid drugs, surgery or radioactive iodine with steroid cover).1
- Smoking cessation—the single most effective modifiable step.4
- Lubricants, sunglasses and prism glasses for mild, inactive disease.
- Immunomodulation for active, moderate-to-severe TED: high-dose IV methylprednisolone; orbital radiotherapy; or biologics such as teprotumumab (IGF-1R inhibitor) and tocilizumab (IL-6 blocker).5
- Sight-threatening optic neuropathy requires urgent IV steroids or surgical orbital decompression.
- Rehabilitative surgery (bone decompression, strabismus correction, eyelid repair) is typically staged after 6–12 months of inactivity.
A multidisciplinary team—endocrinology, oculoplastics, strabismus, radiology and psychology—optimizes outcomes.
Living with Thyroid Eye Disease and Prevention
TED can be emotionally and functionally challenging, but proactive self-care lessens its impact:
- Quit smoking; even reducing cigarette count lowers reactivation risk.5
- Maintain stable thyroid levels—check TSH every 4–6 weeks during adjustment, then every 3–6 months.
- Use preservative-free artificial tears and nightly lubricating ointment to protect the cornea.
- Sleep with head elevated to reduce morning eyelid puffiness.
- Wear wrap-around glasses outdoors to shield from wind and UV.
- Report red-flag symptoms—sudden double vision, color-washout, eye pain or rapid vision loss—immediately.
Joining TED support groups and counseling services can also ease anxiety and body-image concerns.
Latest Research & Developments
TED management is advancing rapidly:
- Teprotumumab, the first FDA-approved targeted therapy, demonstrated an average 3 mm reduction in proptosis and improved diplopia in phase-3 trials.8
- Phase-2 trials of rituximab, low-dose mycophenolate and methotrexate are exploring steroid-sparing regimens.
- High-resolution orbital OCT angiography and AI algorithms are being developed to quantify disease activity objectively and guide treatment timing.7
- 3-D printed, patient-specific orbital implants show promise for safer decompression in the chronic phase.
- International registries are collecting real-world data on long-term safety of biologics and the impact of early intervention on quality-of-life scores.
Recently Published in Peer-Reviewed Journals
Investigative ophthalmology & visual science
July 1, 2025
The miR-320a/PRDX3 Axis Alleviates the Oxidative Stress and Fibrotic Alterations in Fibroblasts in Thyroid Eye Disease.
Liu S, Yi J, Lu S, et al.
Investigative ophthalmology & visual science
June 2, 2025
Three-Dimensional Culture of Orbital Fibroblasts From Thyroid Eye Disease Induce In Vivo-Like Tissue Remodeling and Fibrosis.
Bao X, Xu Z, Wang X, et al.
Ophthalmology
May 19, 2025
Long-term Cardiovascular, Renal, and Safety Outcomes of Teprotumumab versus Systemic Glucocorticoids in Thyroid Eye Disease: A Target Trial Emulation.
Lo JE, Freitag SK, Liu CY, et al.
Next Steps
If you develop persistent eye bulging, double vision, or your vision dims, schedule promptly with an oculoplastic or orbit specialist. These surgeons partner with endocrinologists to manage both the thyroid and the orbit.2 Severe or sight-threatening cases may need referral to tertiary centers that offer biologic infusions, intensity-modulated radiotherapy and endoscopic decompression.
How to schedule: Your endocrinologist or general ophthalmologist can refer you, but many subspecialty clinics accept self-referrals. Tele-ophthalmology platforms like Kerbside can review imaging, confirm disease activity and coordinate timely in-person treatment plans.
