Exposure Keratopathy
Last updated September 6, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.



Overview
Exposure keratopathy (also called exposure keratitis) occurs when the cornea dries out because the eyelids do not close fully or often enough. With the surface uncovered, the tear film evaporates and the cornea can develop dry spots, scratches, or ulcers, leading to pain, light sensitivity, infection, scarring, and—if untreated—vision loss. 1
Exposure may happen during sleep, with facial nerve problems, after eyelid surgery, with thyroid eye disease, or in very ill patients who cannot blink well. The condition is treatable: most people improve with lubrication, protective measures (e.g., eyelid taping or moisture chambers), and procedures to help the lids close when needed. 3
Symptoms
Symptoms can be mild at first and may fluctuate. Common signs include:
- Dryness, burning, or a gritty feeling
- Redness and tearing
- Light sensitivity and blurry vision (often worse late day or on waking)
- Pain or foreign-body sensation
Some people have nocturnal lagophthalmos (sleeping with eyes partly open) and wake with irritation or blur that improves after blinking; others notice trouble closing an eye after Bell’s palsy or other facial nerve issues. 2
Causes and Risk Factors
Anything that limits normal eyelid closure and blinking can cause exposure keratopathy.
Common causes:
- Lagophthalmos from facial nerve palsy (e.g., Bell’s palsy), eyelid scarring, or post–eyelid surgery
- Nocturnal lagophthalmos—eyes partially open during sleep
- Proptosis from thyroid eye disease, preventing full coverage of the cornea 7
- ICU/anesthesia: poor blink and dry air in sedated or ventilated patients
Risk clues include reduced blink rate, poor Bell’s reflex, contact lens overwear on an exposed surface, and dry eye disease. Without care, exposure can lead to erosions, infections, scarring, and vision loss. 1
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
Diagnosis is based on history and a careful eye exam by an optometrist or ophthalmologist.
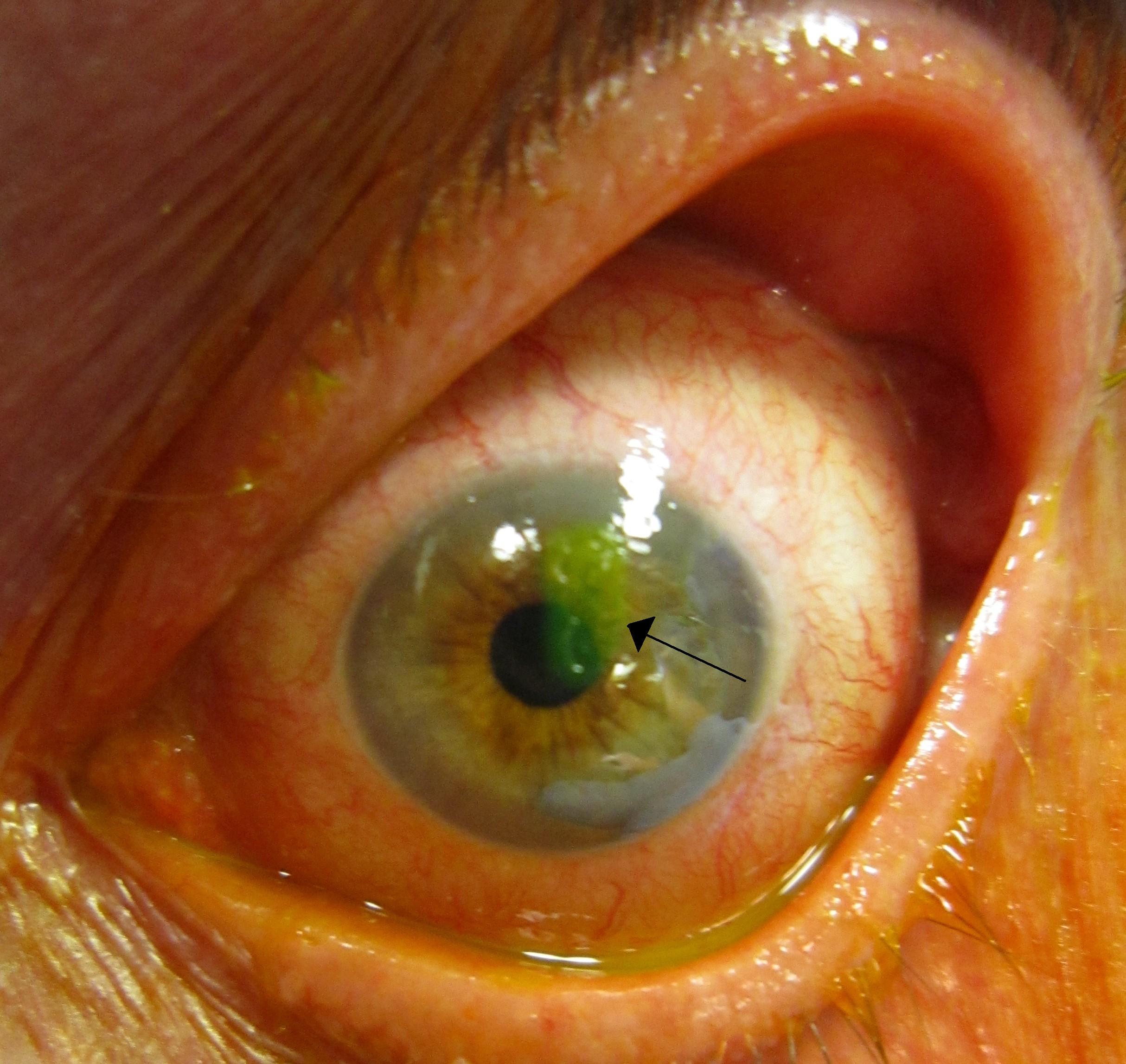
- Slit-lamp exam: dry spots, punctate epithelial erosions, filaments, or ulcers—often inferior (most exposed)
- Fluorescein stain with blue light to highlight scratches/dry areas
- Eyelid exam: lid position (retraction, ectropion), closure strength, blink rate
- Tear film tests: break-up time and staining patterns
Clinicians also seek the cause (e.g., facial nerve palsy, thyroid eye disease, lid scarring) and measure how much the eye remains open on gentle lid closure. 4
Treatment and Management
Goals: keep the cornea moist, protected, and address the underlying cause. Care typically progresses from simple to advanced as needed.
First-line care:
- Preservative-free artificial tears by day and a thick ointment at bedtime
- Eyelid taping or a moisture chamber (goggles/clear shields) during sleep
- Frequent full blinking and screen breaks
- Short antibiotic course if there is an open epithelial defect
Office/advanced options (if exposure persists):
- Bandage soft contact lens or scleral lens for protection
- Punctal plugs to retain tears
- Tarsorrhaphy (temporary partial lid closure) for short-term protection in severe cases 6
- Eyelid weight implant (gold/platinum) or lid repair for chronic facial nerve problems
These approaches are well established; clinicians select the least invasive option that keeps the cornea safe. 4
Living with Exposure Keratopathy and Prevention
Daily steps can protect your eyes and prevent flares:
- Night routine: use ointment before bed; if lids don’t close completely, gently tape them or wear a moisture chamber
- Day routine: preservative-free tears as advised; blink fully/often, especially with screens; wear wraparound glasses outdoors
- Protect in hospital: in ICU or after anesthesia, ask staff about taping or moisture chambers—evidence supports moisture chambers for preventing exposure damage in critically ill patients 5
- Avoid rubbing; follow instructions closely if using a bandage lens
With steady care and follow-up, most people maintain comfort and good vision. 2
Latest Research & Developments
ICU prevention: Reviews/trials suggest moisture chambers (clear goggles or film covers) often outperform ointments alone in preventing exposure keratopathy in sedated/ventilated patients—informing hospital protocols. 8
Eyelid weights for nerve palsy: In chronic facial nerve weakness, upper-lid gold/platinum weights can improve blink and reduce corneal damage; reports show improved surface health post-implantation. 9 Ongoing work explores scleral lenses, biologic tear substitutes (e.g., autologous serum), and refined lid-position/blink surgeries.
Recently Published in Peer-Reviewed Journals
Investigative ophthalmology & visual science
June 2, 2025
Human Platelet Lysate Treatment for Exposure Keratopathy: An In Vivo Confocal Microscopy and Anterior Segment OCT Study.
Tsai CY, Huang WL, Yang SC, et al.
American journal of ophthalmology
May 1, 2022
Tape Splint Tarsorrhaphy for Persistent Corneal Epithelial Defects.
Mimouni M, Liu ES, Din N, et al.
BMC ophthalmology
December 28, 2021
Congenital orbital teratoma: a case report with preservation of the globe and 18 years of follow-up.
Tsoutsanis PA, Charonis GC
Next Steps
If you have exposure symptoms—or were told your eyes don’t close fully—see a cornea or oculoplastic ophthalmologist.
- How to schedule: request an appointment for “exposure keratopathy or lagophthalmos”; bring glasses/contacts info, medication list, and prior eye records
- What to expect: slit-lamp exam, surface staining, tear tests, and eyelid function assessment; plans start with lubrication/protection and may include procedures if needed
- Timing tips: ask for the cancellation list; mention morning blur or pain to convey urgency
For an overview of corneal problems and treatments, see NEI’s corneal conditions page. 3
