Watery Eyes
also known as Epiphora, Tearing
Last updated August 19, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.

Overview
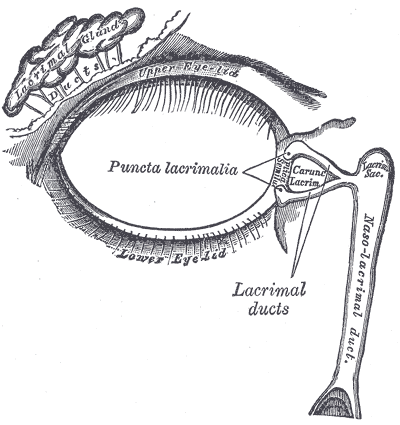
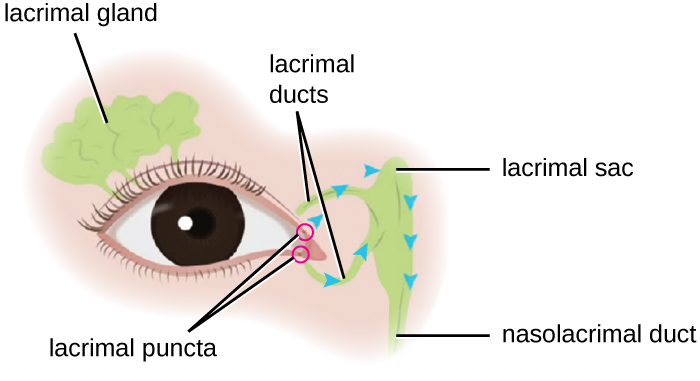
Watery eyes, also called epiphora, happen when your eyes make too many tears or when tears don’t drain away like they should. Tears normally keep the eye healthy and clear. They spread across the eye surface and then flow into tiny openings in the eyelids that drain into the nose. When this balance is off, tears may spill over your lids and run down your cheeks.
Epiphora is common and often temporary, but sometimes it signals a problem such as a blocked tear duct or an eyelid issue that needs treatment. 1 2
Symptoms
Symptoms can be mild or bothersome. You might notice:
- Eyes that look wet or “teary” most of the time.
- Tears running down your face.
- Blurry vision when tears pool on the eye.
- Burning, itching, or a gritty feeling (often from dry eye that triggers reflex tearing).
- Redness or mild discharge if there’s irritation or infection.
- In babies, tears that don’t seem to drain and crusting on the eyelashes.
Get help sooner if you have eye pain, swelling, fever, pus-like discharge, or changes in vision. 3 4
Causes and Risk Factors
Epiphora has two broad causes: too many tears (often from irritation) or poor drainage (a plumbing problem).
- Irritation/overproduction: allergies, dry eye, smoke, wind, bright light, a speck in the eye, eyelid inflammation, or infections like conjunctivitis.
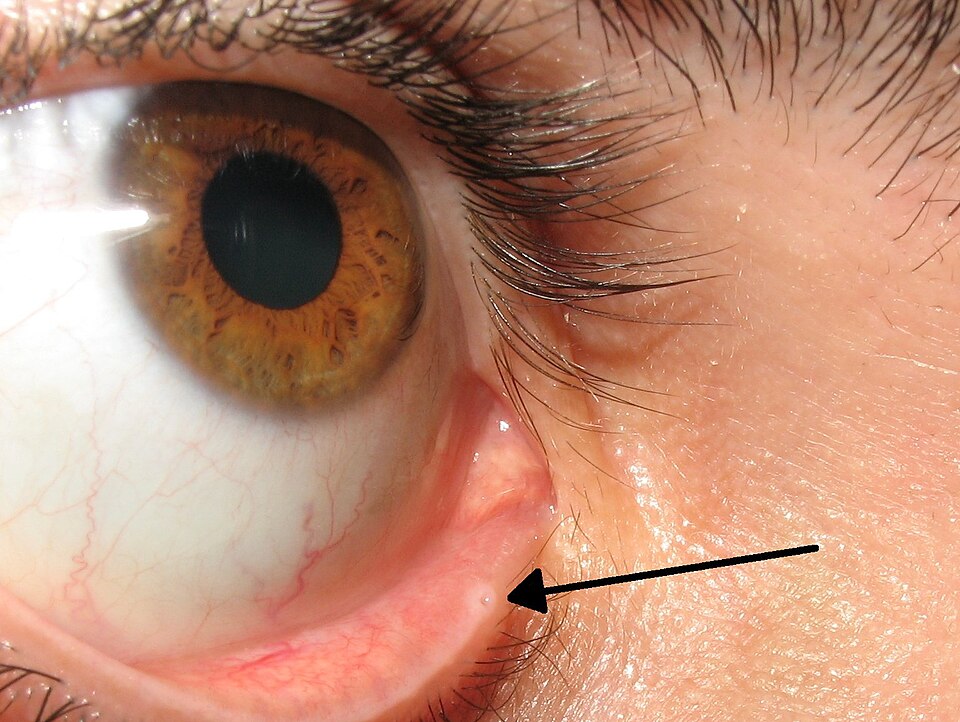
- Drainage problems: narrow or blocked tear ducts, eyelid turning out (ectropion) or in (entropion), or the tear drainage openings (puncta) not lining up with the eye. Babies often have not-yet-open tear ducts that usually clear on their own.
Risks rise with age (eyelid changes and narrowing of ducts), after nose/sinus problems or facial trauma, and with some medicines. In older adults, sagging eyelid skin can pull the lid away from the eye so tears can’t enter the ducts well. Adults can also develop blocked tear ducts from swelling, infection, or injury. 5 Understanding how the tear film and drainage system work also helps explain these causes. 2
Is Your Watery Eye Likely from a Drainage Problem?
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
Your eye doctor will ask about your symptoms and examine your eyes and eyelids. They may check how quickly a drop of harmless dye clears from your eye to see if tears are draining normally. If drainage is slow or blocked, imaging (like X-ray or CT) may be used in some cases.
Because dry eye can paradoxically cause watery eyes, part of the exam is looking for signs of dryness and eyelid disease. Most people don’t need complex testing to start treatment. 1 3
Treatment and Management
Treatment depends on the cause:
- Eye irritation or allergies: avoid smoke/wind when possible; use preservative-free artificial tears; consider allergy drops if recommended by your clinician.
- Dry eye: regular lubricating drops or gels; warm compresses and gentle lid hygiene; manage screen time and room humidity.
- Conjunctivitis or eyelid infection: medicines (like antibiotic drops) if your clinician confirms a bacterial cause.
- Blocked tear ducts: in babies, tear-duct massage and watchful waiting are often tried first. In older kids and adults, office procedures (probing/irrigation, balloon dilation or stents) or surgery may be needed. A common operation, dacryocystorhinostomy (DCR), creates a new pathway for tears to drain into the nose and can be done externally or through the nose (endoscopic). 6
Many cases are mild and improve with simple steps. Your clinician will tailor care to your situation. 4
Living with Watery Eyes and Prevention
A few habits can reduce symptoms:
- Wear wraparound sunglasses on windy or cold days.
- Use preservative-free artificial tears when your eyes feel dry or irritated.
- Avoid rubbing your eyes. Wash hands before touching your face.
- Keep lids clean; use warm compresses if they feel crusty or inflamed.
- Use a humidifier and take blinking breaks during screen time.
- Protect your eyes at work and play with safety glasses or goggles.
If allergies trigger tearing, try to limit exposure and follow your allergy plan. Babies with watery eyes usually improve over weeks to months; ask your pediatric clinician how to clean the lids and when to check back.
Learning how tears are made and drained can help you understand why these steps work. 2 4
Latest Research & Developments
Researchers continue to study the best ways to treat watery eyes.
- For dry-eye–related tearing, punctal plugs (tiny devices that block tear drainage to keep more moisture on the eye) can help some people, but evidence of benefit is mixed, and plugs may sometimes lead to watery eyes or infections; decisions are individualized. 7
- For blocked tear ducts, modern endoscopic DCR surgery avoids a skin incision and offers high success in properly selected patients; surgeons refine techniques and aftercare to improve comfort and outcomes. 6
Recently Published in Peer-Reviewed Journals
BMC ophthalmology
April 15, 2025
A case report of bacterial canaliculitis caused by Ottowia massiliensis Sp.nov.
Wu Y, Sun H, Kang M, et al.
BMC ophthalmology
April 7, 2025
Lacrimal drainage pathway disease-associated keratopathy effectively diagnosed with dacryoendoscopy: a report of two cases.
Inoue H, Toriyama K, Mitani A, et al.
BMC ophthalmology
January 20, 2025
Changes in tear cytokine and lactoferrin levels in postmenopausal women with primary acquired nasolacrimal duct obstruction complicated with obstructed meibomian gland dysfunction.
Jin H, Chen X, Ji F, et al.
Next Steps
If watery eyes are new, constant, or affecting vision, schedule an eye exam. The best specialist to see is a board-certified ophthalmologist (eye MD). If your lids or tear ducts may be the problem, ask for an oculoplastic (eyelid and tear-duct) specialist.
To book care, you can:
- Start with your primary care clinician or optometrist for an initial check. They can refer you to an ophthalmologist if needed.
- When calling an eye clinic, describe your symptoms and ask about waitlists and cancellation slots if the schedule is full.
- For urgent symptoms (eye pain, swelling, fever, sudden vision changes), seek same-day or emergency care.
You can also connect directly with the right specialist on Kerbside for a medical education consult about your condition and care options (this does not establish a patient–physician relationship). For general guidance on when to be seen and typical treatments, the NHS page on watering eyes is a helpful starting point. 4
