Eye Pain
also known as Ocular Pain
Last updated August 19, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.
Overview
Eye pain is discomfort in or around one or both eyes. It can feel scratchy, burning, aching, sharp, or throbbing. Some causes are minor and improve with simple care (like dry eye or eyestrain), while others are emergencies that can threaten vision if not treated quickly (such as a chemical splash, a deep corneal infection, or a sudden pressure spike inside the eye). Knowing the warning signs helps you decide how fast to seek help. 1
Common causes include dry eye, conjunctivitis ("pink eye"), a scratched cornea, uveitis (inflammation inside the eye), and infection or inflammation from contact lens wear. 2
Symptoms
Eye pain can appear in different ways. You may notice:
- Surface irritation: burning, scratchy, sandy feeling, or stinging.
- Deep eye ache: pain that seems inside the eye, sometimes worse with eye movement or in bright light.
- Other clues: redness, tearing, light sensitivity, blurred vision, headache, halos around lights, or nausea.
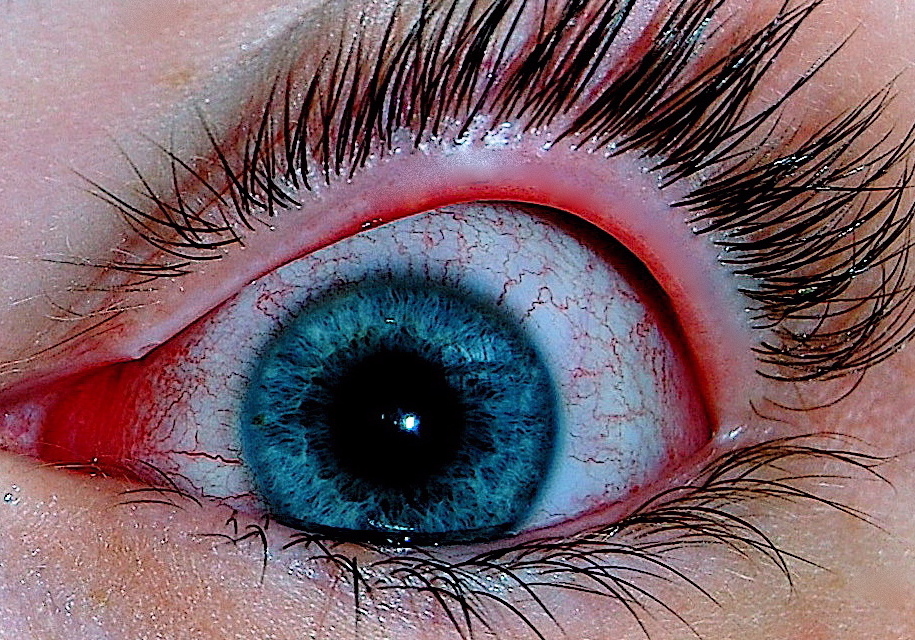
Red flags that need urgent care include severe pain with sudden blurry vision, rainbow halos, headache and nausea, or a very red eye that won’t improve—these can signal acute angle-closure glaucoma, an emergency. 3 Pain plus light sensitivity and reduced vision can suggest uveitis and also needs prompt evaluation. 4
Causes and Risk Factors
Many conditions can cause eye pain. Common examples include:
- Dry eye: not enough healthy tears or fast evaporation causes burning or stinging and blurred vision that improves after blinking. 5
- Conjunctivitis (pink eye): inflammation from viruses, bacteria, or allergies.
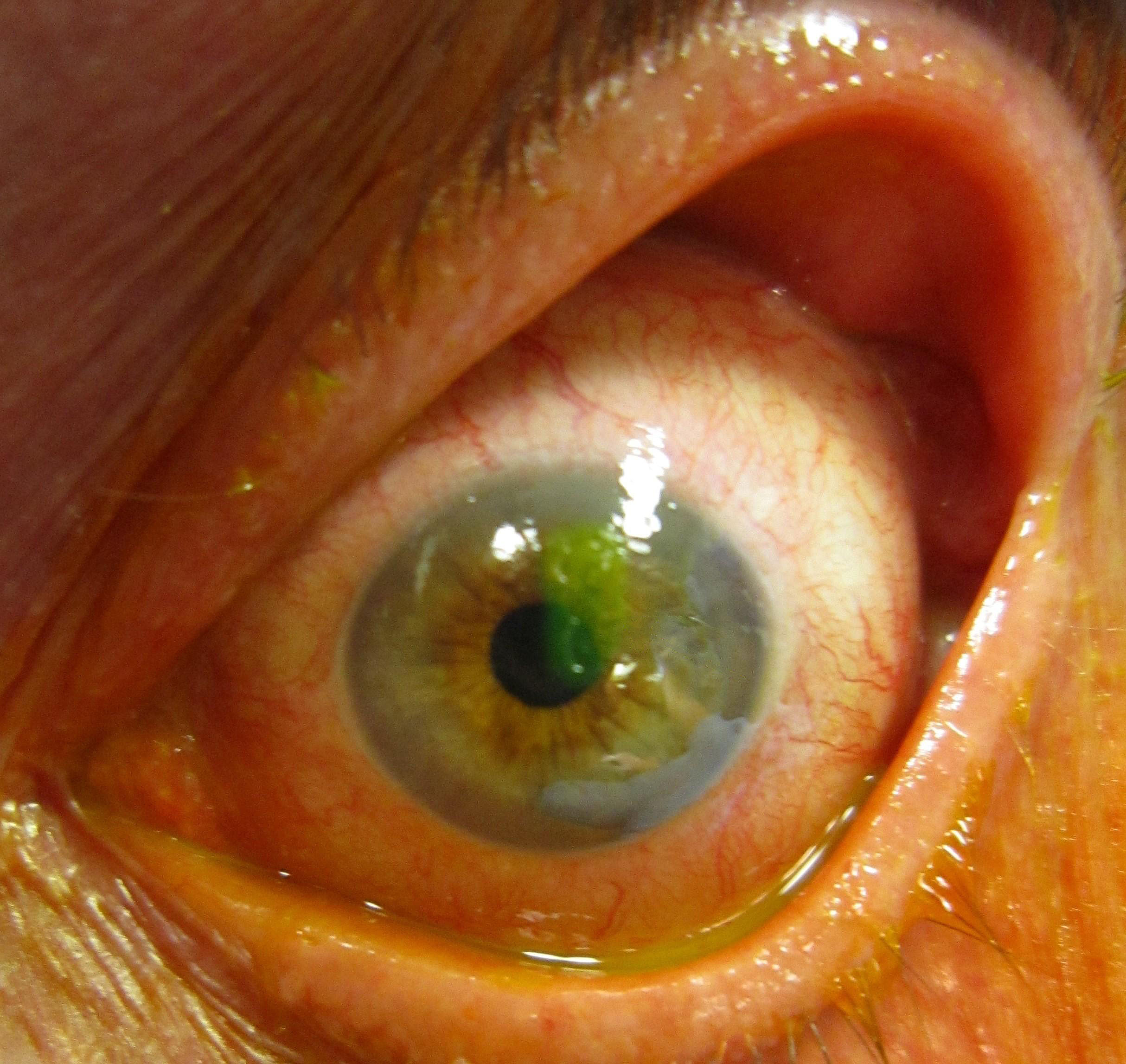
- Corneal problems: abrasion (scratch), foreign body, or infection (keratitis) causing sharp pain, tearing, and light sensitivity. Contact lens wear and poor lens hygiene raise keratitis risk. 6
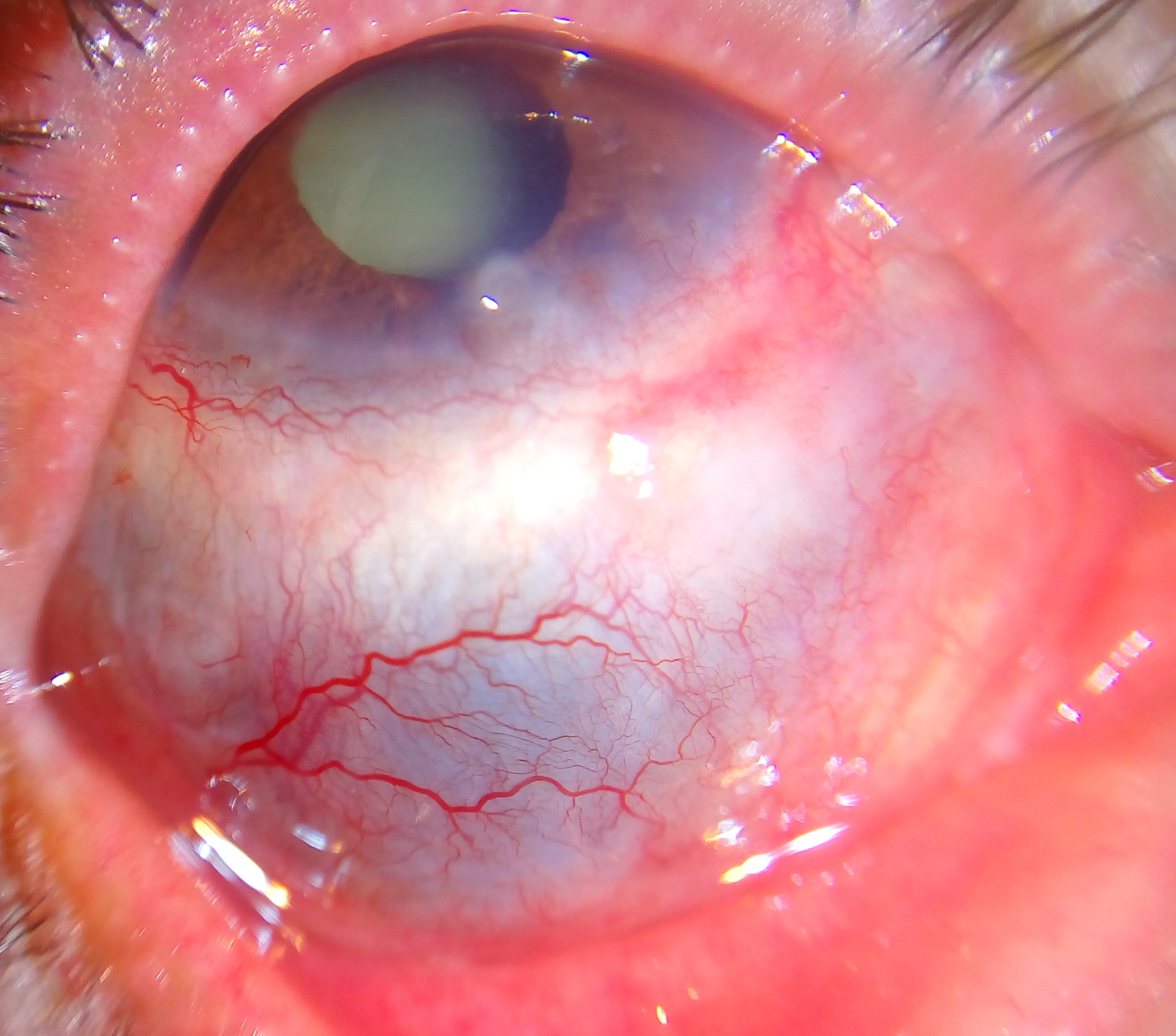
- Uveitis: inflammation inside the eye, often with light sensitivity and decreased vision.
- Scleritis: severe, boring eye pain from inflammation of the white coat of the eye, sometimes tied to autoimmune disease.
- Glaucoma (acute angle closure): sudden high eye pressure causing intense pain, halos, and nausea.
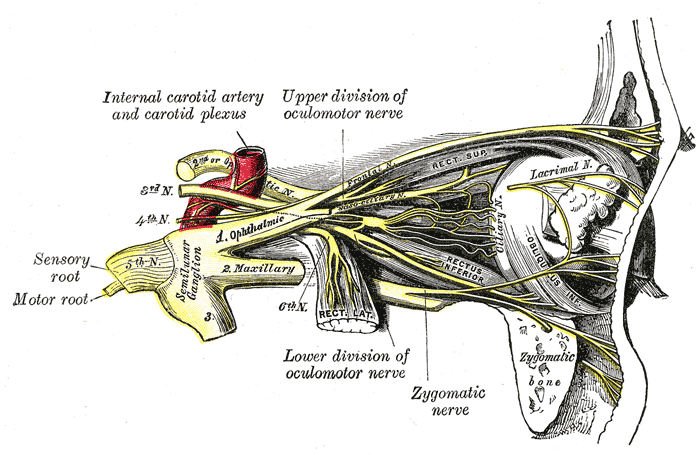
- Optic neuritis and headaches: pain with eye movement (optic neuritis); migraine or cluster headaches can cause pain around or behind the eye.
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
An eye care professional will ask about symptoms and examine your eyes. Depending on the situation, tests may include:
- Vision and pupil checks to see clarity and pupil reactions.
- Slit-lamp exam to look closely at the cornea and surface; fluorescein dye may show a scratch or ulcer. 8
- Eye pressure (tonometry) to screen for glaucoma.
- Eyelid flip and foreign body check if something may be stuck under the lid.
- Dilated exam to examine the retina and optic nerve.
For chemical exposures or serious injuries, immediate irrigation and urgent referral are essential. 7
Treatment and Management
Treatment depends on the cause. General guidance:
- Dry eye or eyestrain: preservative-free lubricating drops, regular screen breaks, adjust lighting/screen height; consider a humidifier.
- Conjunctivitis: viral cases often improve on their own; cool compresses and artificial tears can soothe. Bacterial cases may need antibiotic drops. Avoid contacts until cleared.
- Contact lens wearers: with pain, redness, or blur, remove lenses and call your eye professional. Good lens hygiene helps prevent infections like keratitis. 9
- Corneal abrasion or foreign body: do not rub the eye. Providers may remove the foreign body and protect the eye. 10
- Chemical splash: rinse with clean water or saline for at least 15 minutes and seek emergency care.
- Acute angle-closure glaucoma: this is an emergency; go to the ER or on-call ophthalmologist without delay.
Living with Eye Pain and Prevention
You can lower your chances of eye pain and protect your sight by:
- Resting your eyes: follow the 20–20–20 rule for screens. 11
- Using protective eyewear for sports, yardwork, and DIY projects.
- Practicing contact lens hygiene: never sleep, swim, or shower in lenses; clean and store as directed; replace cases regularly. 12
- Managing allergies if eyes are itchy or watery—ask about safe eye treatments.
- Scheduling regular eye exams, especially if you wear contacts or have diabetes, autoimmune disease, or glaucoma risk.
Most eye pain improves with the right diagnosis and care. Seek help if symptoms are severe, new, or not getting better.
Latest Research & Developments
Scientists are learning more about how the eye senses pain and why some people develop long-lasting or \"neuropathic\" ocular pain even after the surface looks normal. The U.S. National Eye Institute has funded projects to map corneal nerves and better understand ocular pain pathways—work that may lead to new treatments for dry eye, migraine-related light sensitivity, and other painful eye conditions. 13 For dry eye and meibomian gland disease (MGD), studies are evaluating intense pulsed light (IPL) therapies; evidence is still evolving and not all trials are low risk of bias. 14
Recently Published in Peer-Reviewed Journals
BMC ophthalmology
July 28, 2025
Endophthalmitis following inadvertent intravitreal injection of botulinum toxin: a case report and literature review.
Aljohani SM, Alharbi AS, Alhayaza RM
BMC ophthalmology
July 10, 2025
Intraocular lens subluxation obstructing a glaucoma tube shunt after a Valsalva maneuver: a case report.
Ha A, Nam KT, Kim S, et al.
BMC ophthalmology
July 1, 2025
A rare case of membrane pupillary-block glaucoma in a phakic eye with uveitis.
Iwahashi C, Fukuda M, Makita S, et al.
Next Steps
Who to see: For new or ongoing eye pain, the best first stop is a board-certified ophthalmologist (medical eye doctor). If symptoms are severe—such as sudden vision loss, halos with headache and nausea, a very red eye, or a chemical splash—seek emergency care right away. 15
How to schedule: Explain your symptoms clearly when you call. Ask for a same-day or next-day urgent slot if you have vision changes, light sensitivity, or contact lens–related pain. If clinics are booked, join a waitlist and ask about cancellation openings. For injuries, follow first-aid steps and proceed to urgent or emergency care as advised. 16
On Kerbside: You can connect with the right specialist on Kerbside for a medical education consult. We can help you understand your diagnosis, tests, and treatment options. This service supports your care but does not create a patient–physician relationship.
