Optic Neuritis
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.

Overview
Optic neuritis (ON) is an inflammation of the optic nerve that abruptly disrupts the flow of visual information from the eye to the brain. Most attacks strike adults between 18 – 45 years and cause eye-pain that worsens with movement, followed by rapid loss of vision in one eye.1 Up to 70 % of first-time ON cases are linked to demyelinating diseases such as multiple sclerosis (MS), neuromyelitis optica spectrum disorder (NMOSD) or MOG-antibody–associated disease (MOGAD).2 Fortunately, vision recovers in 9 of 10 people—often within weeks—especially when high-dose intravenous steroids are started early. Ongoing research into immune-modifying biologics and neuro-protective therapies aims to preserve optic-nerve tissue and lower the risk of future attacks.
Symptoms
- Pain with eye movement—classically precedes vision loss by 1–3 days and resolves first.3
- Sub-acute monocular vision loss—blurry or dim vision that can progress to hand-motions only.
- Washed-out colors (dyschromatopsia)—reds look brown or gray.
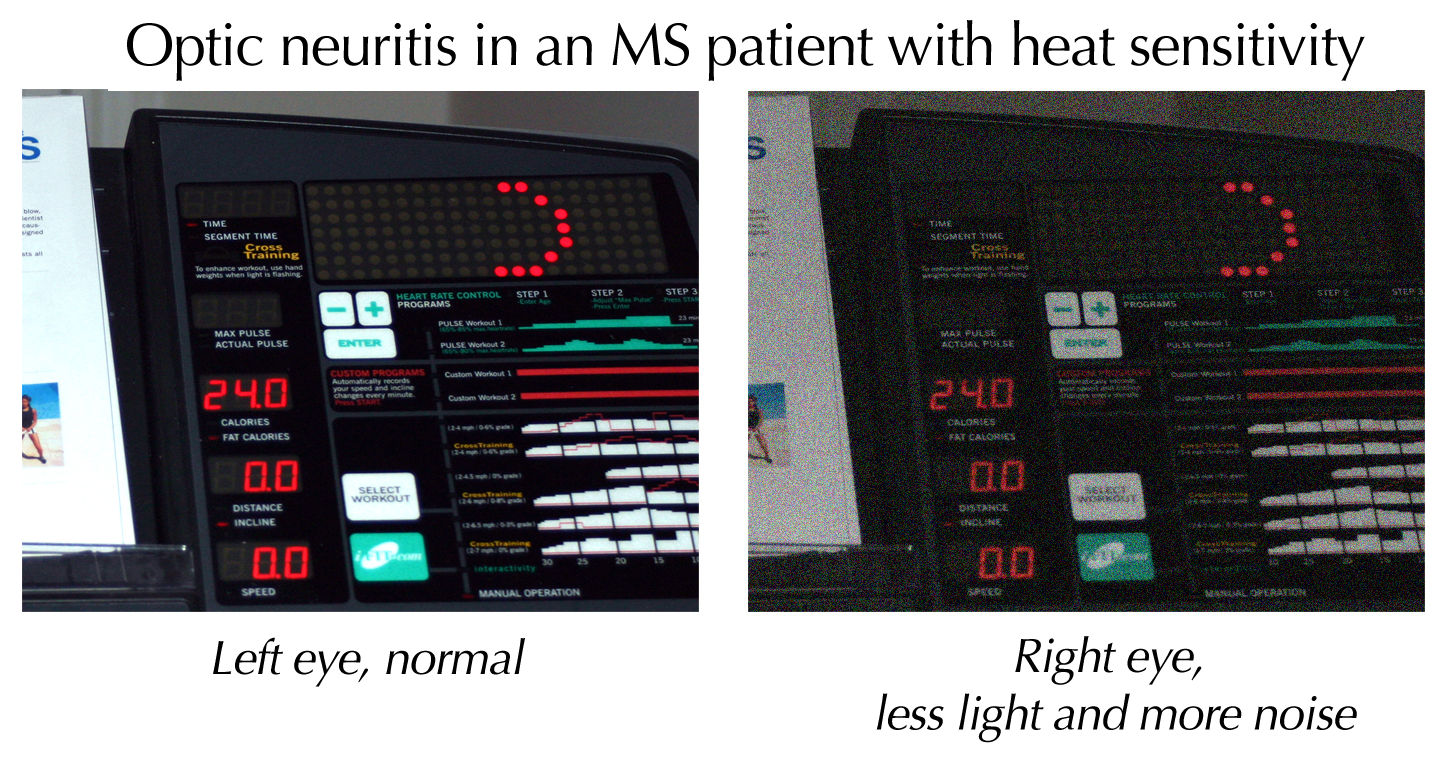
- Uhthoff phenomenon—vision worsens when body temperature rises (hot shower or exercise).
- Photopsias—brief flashes or flickers of light.
- A relative afferent pupillary defect (RAPD)—the pupil of the affected eye constricts poorly to light.
Children may present with bilateral disc swelling and fewer pain complaints, whereas adults more often have unilateral, retro-bulbar lesions that look “normal” on initial exam—hence the phrase “the patient sees nothing, and the doctor sees nothing.”4
Causes and Risk Factors
ON is usually immune-mediated but several contributors raise risk:
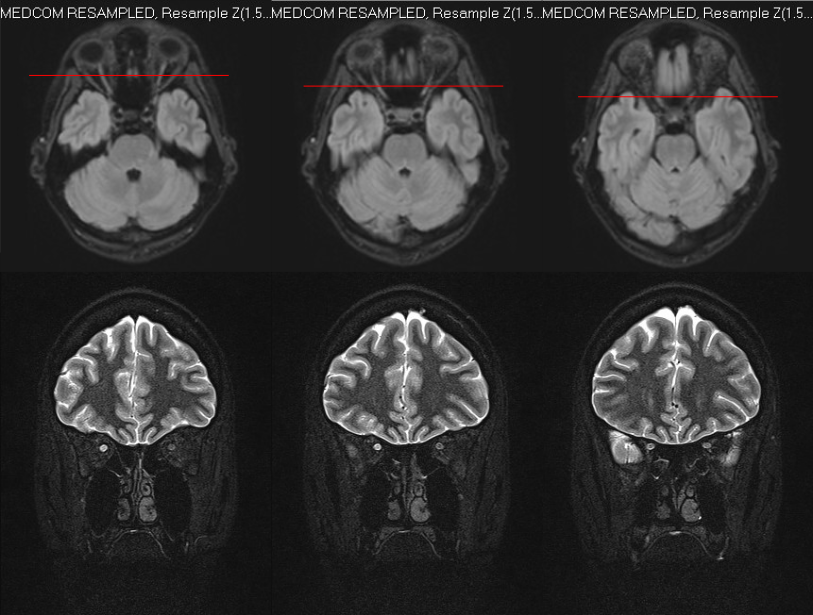
- Demyelinating disease—first manifestation of MS in ~20 % of patients; risk rises with ≥ 1 brain MRI lesion.5
- Serum antibodies—aquaporin-4 (AQP4) marks NMOSD; myelin-oligodendrocyte-glycoprotein (MOG) marks MOGAD.
- Female sex—auto-immune ON is twice as common in women.6
- Smoking—doubles the odds of MS conversion after an ON attack.
- Infections or vaccines—rare post-viral or post-immunization ON has been reported.
- Drugs/toxins—ethambutol, amiodarone, chloramphenicol and excess radiation can injure the optic nerve.
Risk of Developing MS Within 5 Years After First Optic Neuritis Attack
Select your details to estimate risk factors.
Diagnosis
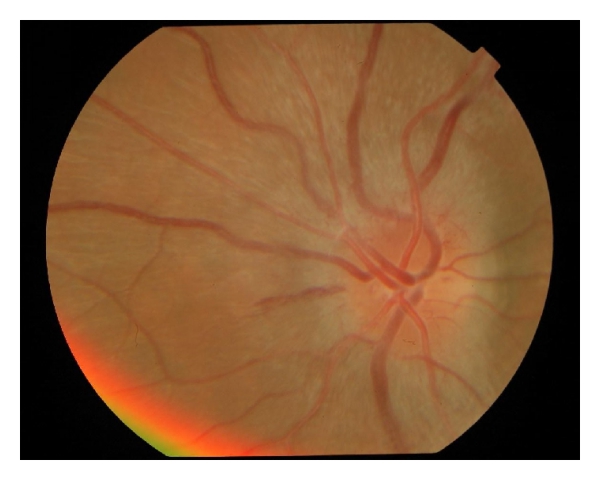
- Comprehensive eye exam—visual acuity, color plates, pupillary testing and dilated funduscopy to look for optic-disc swelling (papillitis).
- Orbital & brain MRI with contrast—T2/FLAIR hyper-intensity and gadolinium enhancement of the optic nerve confirm inflammation and screen for demyelinating lesions elsewhere.7
- Visual Evoked Potential (VEP)—checks conduction speed along the optic pathway; a delayed P100 latency supports demyelination.8
- Blood tests—AQP4-IgG, MOG-IgG, syphilis, Lyme and B12 levels as indicated.
- Lumbar puncture—oligoclonal bands bolster MS risk-assessment if MRI is equivocal.
Treatment and Management
Acute attack
- High-dose IV methylprednisolone (1 g/day × 3–5 days) speeds visual recovery and may delay MS onset.9
- Switch to a brief oral prednisone taper (e.g., 1 mg/kg for 11 days) to minimize rebound inflammation—a lesson learned from the Optic Neuritis Treatment Trial (ONTT).10
- Plasma exchange or IVIG for steroid-refractory NMOSD or MOGAD attacks.
Long-term disease modification
- MS-directed agents (interferon-β, dimethyl-fumarate, ocrelizumab) reduce future relapses.
- NMO spectrum disorder is managed with rituximab, eculizumab or satralizumab.
- MOGAD may respond to mycophenolate, azathioprine or monthly IVIG.
Living with Optic Neuritis and Prevention
Most people regain 20/40 or better vision, yet subtle deficits in contrast or color may persist. To protect your sight:
- Follow-up MRIs and neuro-ophthalmic exams every 6–12 months during the first two years.
- Vitamin D sufficiency, regular exercise and smoking cessation—all lower MS activity.11
- Protective eyewear for sports—vision is monocular while the affected eye heals.
- Heat management—cool showers or cooling vests can blunt Uhthoff symptoms.
- Medication safety—always tell providers you have demyelinating disease before starting TNF-α inhibitors, which may trigger relapses.12
Latest Research & Developments
- ONTT 30-year follow-up—baseline MRI lesions remain the strongest predictor of future MS, guiding surveillance intensity.13
- Lancet Neurology 2023 review—biologic therapies targeting complement (eculizumab) and interleukin-6 (satralizumab) cut NMOSD relapse rates by > 70 %.14
- Gene-editing & axon-regeneration studies—NEI-funded teams identified embryonic-like neurons that could one day repair optic-nerve damage.15
- Antibody-specific prognosis—MOG-IgG-positive ON has higher relapse risk but better visual recovery than AQP4-IgG ON; trials of inebilizumab are underway.
- Portable VEP devices being validated for at-home monitoring of optic-nerve function.16
Recent Peer-Reviewed Research
Bilateral optic neuritis in a patient with idiopathic intracranial hypertension: a case report.
Yao W, Xu Y, Gan CL, et al.
Factors Associated With Relapse in Patients With Neurosarcoidosis.
Nitsch L, Skowasch D, Courtin E, et al.
Clinical Features and Factors Associated With Outcome in Late Adult-Onset Myelin Oligodendrocyte Glycoprotein Antibody-Associated Disease.
Dinoto A, Cacciaguerra L, Vorasoot N, et al.
Next Steps
Who to see: If you notice sudden eye pain or decreased vision, arrange an urgent evaluation with a neuro-ophthalmologist—a physician trained in both neurology and ophthalmology.
How to schedule: Ask your primary-care doctor or emergency department to mark the referral as “acute optic neuritis.” Many tertiary centers keep same-day infusion slots for steroid initiation. Tele–triage nurses can advise whether you need immediate imaging before traveling.
After discharge, keep follow-ups, review MRI results, and discuss long-term disease-modifying therapy if lesions or antibodies are present. You can also connect directly with board-certified specialists on Kerbside for a medical-education consult (no patient-physician relationship will be established) to better understand your options and questions before your next in-person visit.17