Meibomian Gland Dysfunction
Also known as MGD
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.

Overview
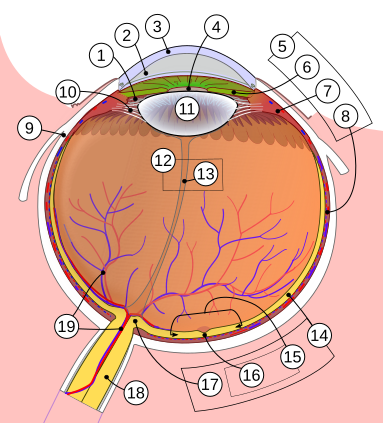
Meibomian gland dysfunction (MGD) is the leading cause of evaporative dry eye. Tiny oil-secreting glands in your upper and lower lids thicken or clog, so the lipid layer that normally prevents tears from drying out becomes patchy. As a result, the ocular surface dehydrates, triggering burning, fluctuating vision and irritation.1 Population studies suggest that up to two-thirds of people with dry eye have signs of MGD, yet it often goes undiagnosed for years.2
Symptoms
- Scratchy, sandy or burning sensation that worsens in air-conditioned or windy environments.
- Intermittent blurry vision that clears after a blink.
- Watery eyes (reflex tearing) as the surface tries to compensate for lipid loss.
- Red, swollen lid margins with crusting or frothy tear film.
- Styes (hordeola) or chalazia that recur in the same spot.
Symptoms usually affect both eyes and may wax and wane throughout the day.34
Causes and Risk Factors
MGD develops when meibum becomes thicker than normal or when the gland openings scar over. Major risk factors include:
- Aging and hormonal shifts—glands atrophy after age 50, especially in women.
- Rosacea and seborrheic dermatitis that inflame lid margins.
- Long-term contact lens wear and heavy digital-screen use that suppress blinking.
- Low omega-3 intake, high cholesterol or certain acne medicines (e.g., isotretinoin).
- Environmental stressors—low humidity, smoke and air pollution.
A large review found that people over 50 are nearly four times more likely to have MGD than those under 30.56
MGD Risk Score Estimator
Select your details to estimate risk factors.
Diagnosis
Your eye-care professional will:
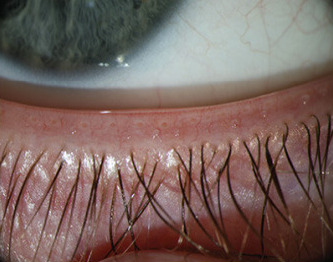
- Examine lids with a slit-lamp microscope to look for capped or missing orifices, telangiectasia and toothpaste-like meibum.
- Apply gentle pressure to the glands (meibomian expression) to grade secretion quality.
- Measure tear break-up time (TBUT); <10 seconds suggests evaporative dry eye.
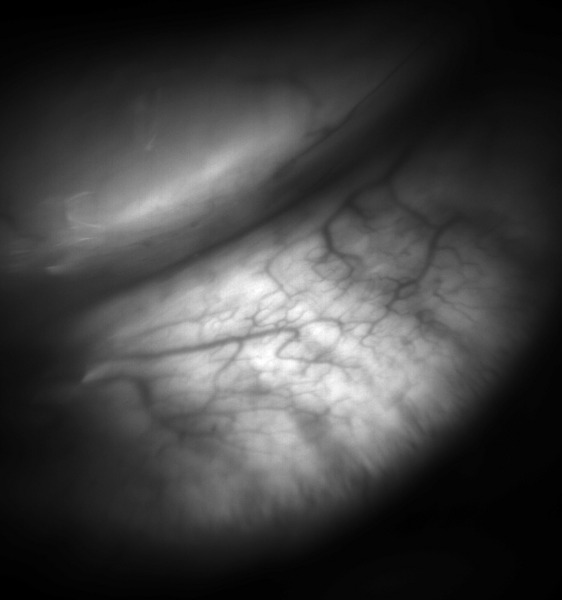
- Use non-contact infrared meibography to image gland dropout or distortion.
These tests help separate MGD from aqueous-deficient dry eye and allergic conjunctivitis.78
Treatment and Management
Therapy targets both obstruction and inflammation:
- Daily warm compresses + lid massage to liquefy and express stagnant oil.
- Eyelid hygiene (dilute baby shampoo, hypochlorous acid, or commercial foam cleansers) removes biofilm and Demodex.
- Topical anti-inflammatories (low-dose steroids, cyclosporine, lifitegrast) calm the ocular surface.
- Oral tetracyclines (doxycycline or minocycline) reduce gland inflammation and thin meibum.
- In-office thermal pulsation or intense pulsed light (IPL) delivers heat and mechanical pressure to unblock glands with results lasting 6–12 months.
Clinical studies show thermal pulsation can improve symptoms and gland scores for the majority of patients who fail conventional care.910
Living with Meibomian Gland Dysfunction and Prevention
Consistent self-care keeps glands flowing:
- Blink fully every 20 minutes while reading or using screens; follow the 20-20-20 rule.
- Add 1–2 g of omega-3 fatty acids (fish-oil or flaxseed) daily to improve meibum quality.
- Use a room humidifier and limit direct fan or heater airflow to your face.
- Replace old eye makeup every 3 months; avoid tight eyeliner that blocks gland openings.
- Schedule yearly eye exams—even when symptoms seem under control.
Following these steps, many patients report a 50 % reduction in flare-ups within three months.1112
Latest Research & Developments
Researchers are exploring stem-cell-based therapies to regenerate atrophied glands and restore healthy lipid output. A 2025 National Eye Institute–funded mouse study pinpointed Hedgehog signaling as a key driver of meibomian stem-cell renewal, opening the door to drug targets that could reverse age-related gland loss.13 Multiple phase-2 trials listed on the NEI clinical-trials database are also testing novel topical perfluorohexyloctane and protease inhibitors designed to stabilize the tear film without preservatives.14
Recent Peer-Reviewed Research
Factors Associated With Perfluorohexyloctane Treatment Response in Dry Eye Disease Associated With Meibomian Gland Dysfunction.
Gu H, Li Z, Zhu L
Comparative Analysis of Age-Associated Changes in Meibum Composition, Distribution, and Function in Mice With Altered Hyaluronan Expression.
Verma S, Montoya PAG, Sun M, et al.
Calcium-Dependent Regulation of Desmosomal Proteins in Human Meibomian Gland Epithelial Cells.
Garreis F, Adelung S, Schicht M, et al.
Next Steps
If your eyes remain gritty or vision blurs despite warm compresses and over-the-counter drops, ask for a referral to a dry-eye or ocular surface specialist. These clinicians can perform meibography, tailor prescription regimens, and discuss thermal pulsation or IPL. You can self-refer, request a referral from your optometrist, or connect directly with vetted specialists on Kerbside—whatever is most convenient. Bring a list of current medications, supplements and previous treatments so the visit is efficient.1516
Trusted Specialists
Board-certified providers specializing in Meibomian Gland Dysfunction.
