Eye Allergies
also known as Allergic Conjunctivitis
Last updated August 4, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.
Overview
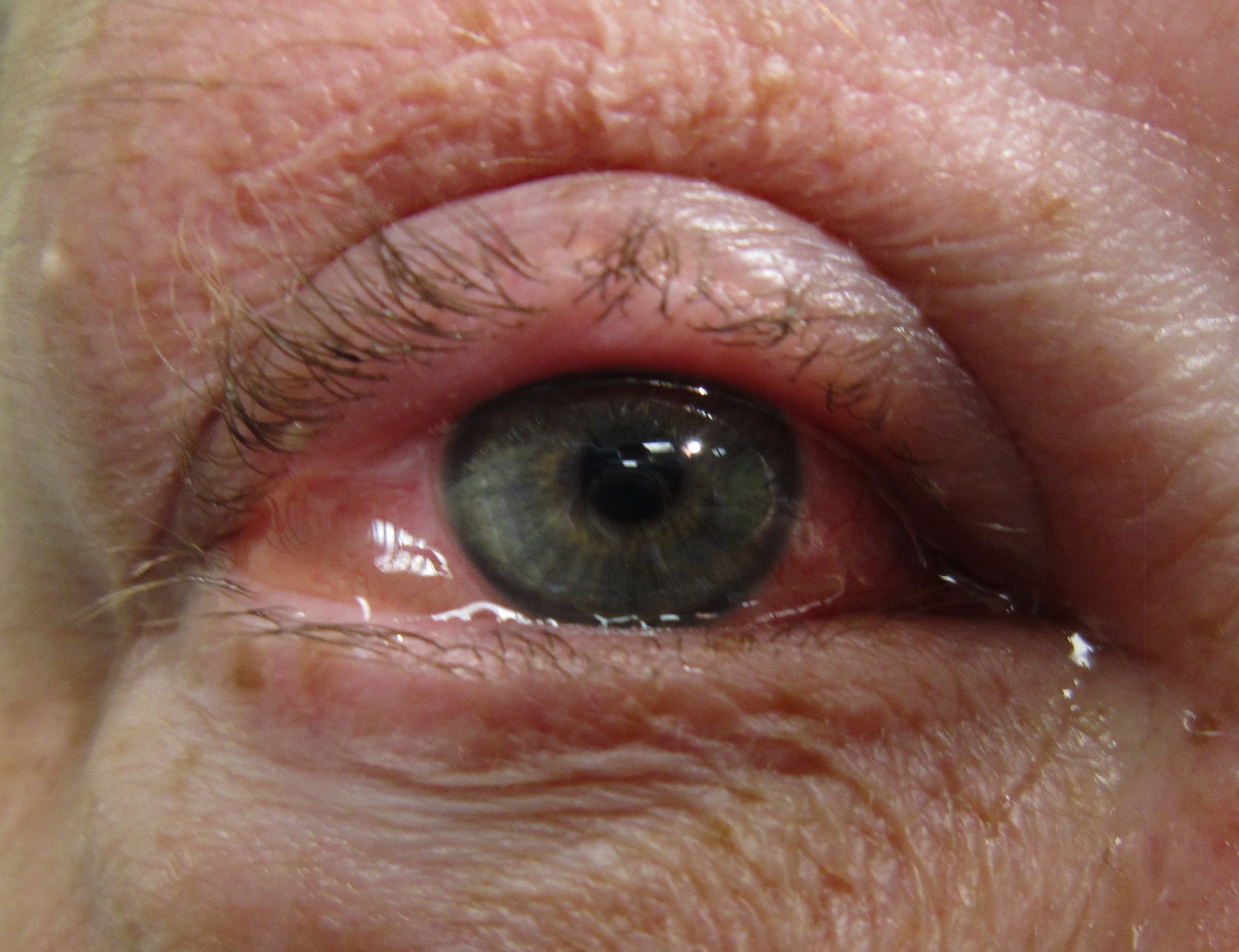
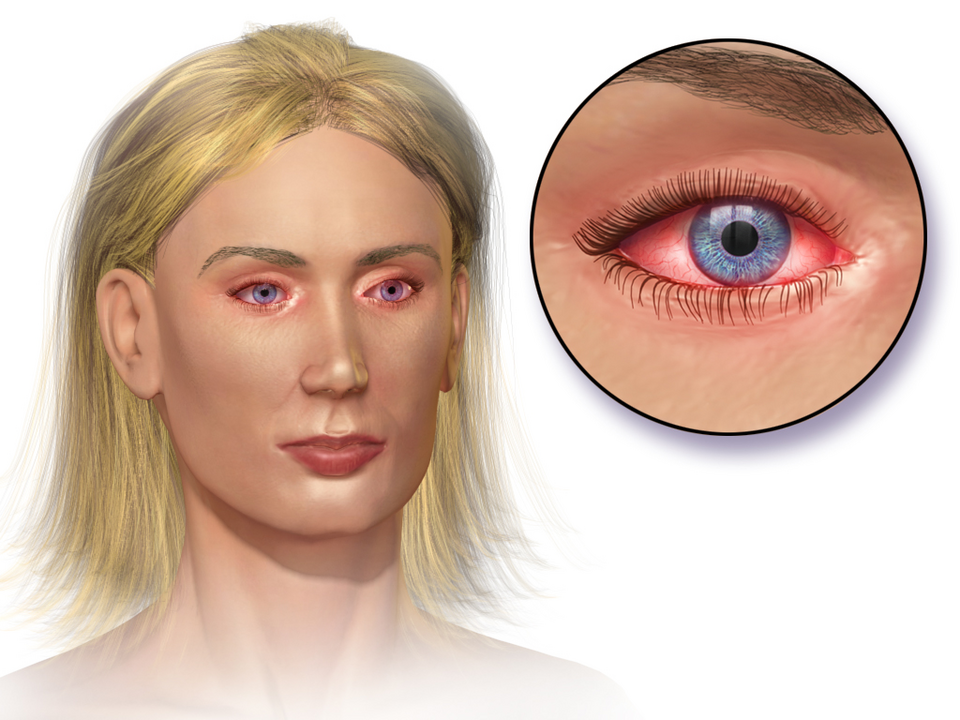
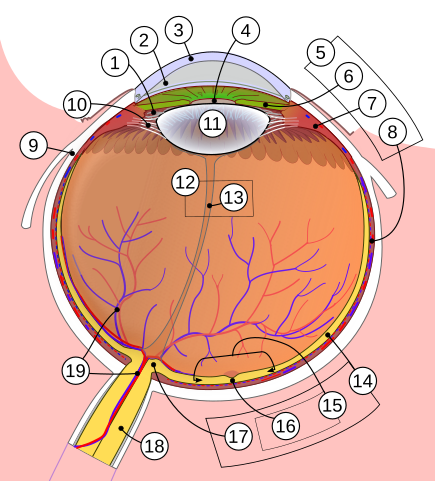
Eye allergies—medically called allergic conjunctivitis—happen when your immune system over-reacts to harmless triggers such as pollen, pet dander or dust. Histamine and other inflammatory chemicals flood the thin membrane that lines the eyelids and covers the whites of your eyes (conjunctiva), leaving them red, itchy and watery. Up to 40 % of people experience ocular allergy symptoms at some point, and many also have nasal allergies or asthma.1 Unlike viral or bacterial “pink eye,” eye allergies are not contagious but they can still blur vision, disrupt sleep and impair performance at school or work if left untreated.2
Symptoms
- Intense itching or burning that makes you want to rub your eyes.
- Redness and swelling of the conjunctiva and lids.
- Watery or “stringy” mucus discharge that may cloud vision.
- Tearing and light sensitivity, especially on windy days.
- Nasal symptoms—sneezing, congestion, an itchy throat—often accompany the eye complaints.
Both eyes are usually affected and symptoms may last for weeks during pollen season or all year round if indoor allergens are to blame.13
Causes and Risk Factors
Any airborne particle that provokes an IgE-mediated immune response can spark eye allergies. Common culprits include:
- Seasonal pollens from trees (spring), grasses (summer) and weeds (fall).
- Indoor allergens such as dust-mite debris, pet dander and mold spores.
- Contact allergens—cosmetics, contact-lens solutions or workplace chemicals.
Personal or family history of hay fever, eczema or asthma raises risk. Living in high-pollen regions or spending long hours outdoors without eye protection adds to the burden.24
Eye Allergy Risk Estimator
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
Your eye-care professional will review your history, examine the surface of each eye with a slit-lamp microscope and look for tell-tale bumps (papillae) on the inner lids. The presence of itching plus watery discharge strongly suggests an allergic cause. If the picture is unclear—or if symptoms are severe or year-round—you may be referred for skin-prick or blood-IgE tests to pinpoint offending allergens.6 In rare cases, doctors gently scrape the conjunctiva to count eosinophils, a type of allergy cell.3
Treatment and Management
Step-wise care usually provides quick relief:
- Cold compresses and preservative-free artificial tears flush allergens and soothe burning.
- Over-the-counter antihistamine / mast-cell-stabilizer drops (e.g., ketotifen) ease itching within minutes and protect for 8–12 hours.
- Prescription dual-action drops (olopatadine, alcaftadine) or topical antihistamines such as azelastine are next-line options.1
- Short courses of mild steroid droplets may be added for severe swelling, but require monitoring for side-effects.
- For stubborn, multi-season disease, allergy immunotherapy (shots or under-the-tongue tablets) retrains the immune system over time.7
Living with Eye Allergies and Prevention
You can’t change pollen counts, but you can limit exposure and calm inflammation:
- Wear wrap-around sunglasses when outdoors; shower and change clothes after yardwork.
- Keep windows closed on high-pollen days; use high-efficiency (HEPA) filters indoors.
- Wash pets weekly and run a dehumidifier to discourage dust-mites and mold.
- Avoid rubbing—friction worsens swelling and can scratch the cornea.
Daily lubricating drops, cool compresses and disciplined allergy-pill use help many people breeze through peak seasons.25
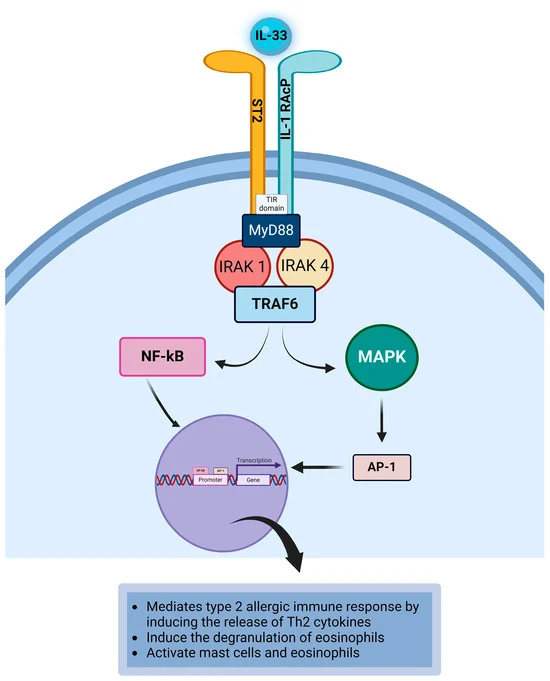
Latest Research & Developments
Scientists are testing biologic agents that block interleukin-4 and interleukin-13—the same pathway targeted in asthma and eczema—to see if they can quiet severe, steroid-dependent ocular allergy. The National Eye Institute (NEI) lists several active clinical trials exploring new topical nanocarrier antihistamines and gene-edited mast-cell inhibitors.9 Early data suggest these therapies may reduce itching scores by 50 % or more while lowering steroid use.8
Recently Published in Peer-Reviewed Journals
BMC ophthalmology
April 17, 2025
The therapeutic effect of IPL on children with refractory seasonal allergic conjunctivitis.
Jiang J, Yang X, Du F, et al.
BMC ophthalmology
February 4, 2025
Keratoconus with two consecutive re-emergences: a case report.
Zhang P, Wu Y, Ma L, et al.
BMC ophthalmology
December 19, 2024
High body mass index with the risk of allergic conjunctivitis in children: a case-control study in Southwest China.
Tang XJ, He JT, Liu Q, et al.
Next Steps
If OTC drops no longer control redness or your vision blurs, book an appointment with a cornea or ocular surface disease specialist. They can perform in-office testing, tailor prescription therapy and coordinate with an allergist for immunotherapy when appropriate. Referrals often come from primary eye-care providers, but you can also self-refer or use Kerbside to connect directly with nearby experts. Bring a list of medications, known allergies and any previous skin-test results to streamline care.12
