Thermal Pulsation for Meibomian Gland Dysfunction (MGD)
Also known as Thermal Pulsation
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms for details.

Overview
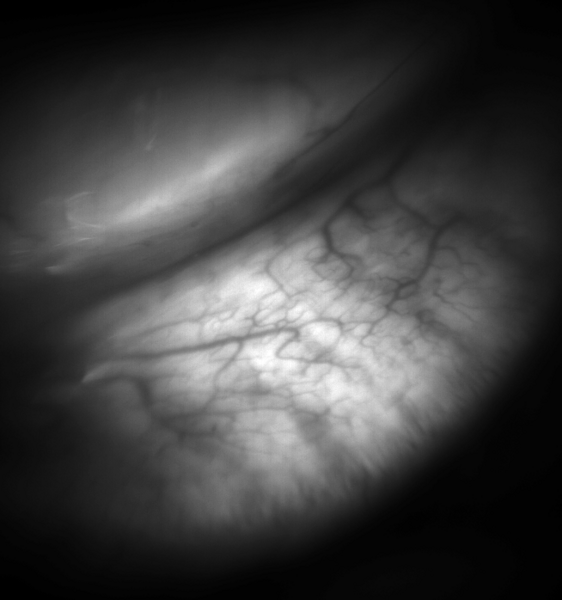
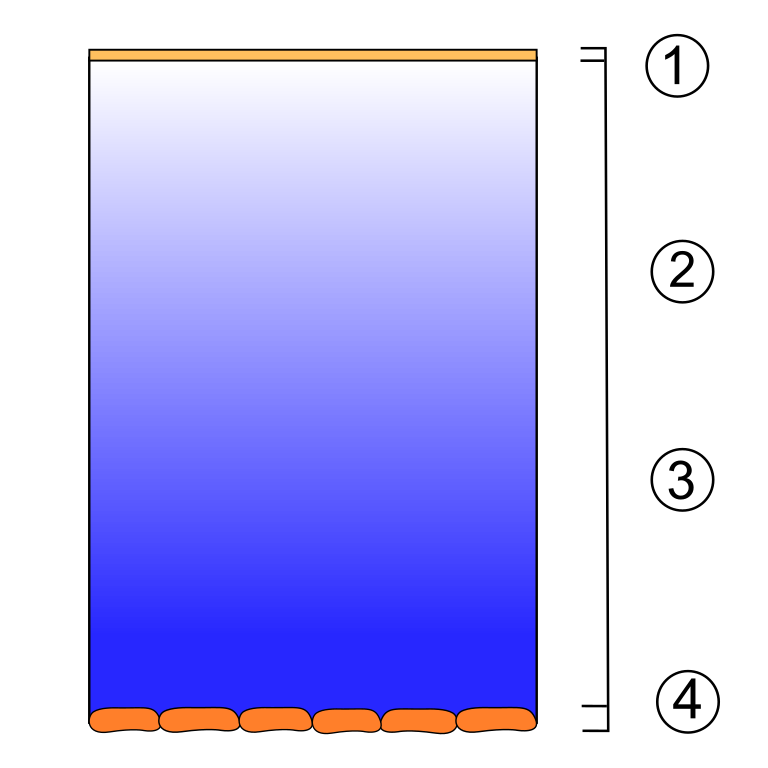
Thermal pulsation is an in-office treatment that gently warms and massages the eyelids to melt and clear clogged meibomian glands. These glands make the oil layer of your tears. When oil is thick or blocked, tears evaporate too fast and eyes can feel dry, gritty, or blurry—especially during reading or screen time. 1
A 2023 technology assessment in Ophthalmology reviewed many studies and found that thermal pulsation can improve signs and symptoms of meibomian gland dysfunction (MGD)–related dry eye in selected adults. 2
Think of thermal pulsation as a targeted, medical-grade version of warm compresses plus lid massage. The device applies controlled heat to the inner or outer eyelids and gentle pressure to express thickened oils, helping glands flow again so the tear film is more stable and comfortable.
How the Procedure Works & Options
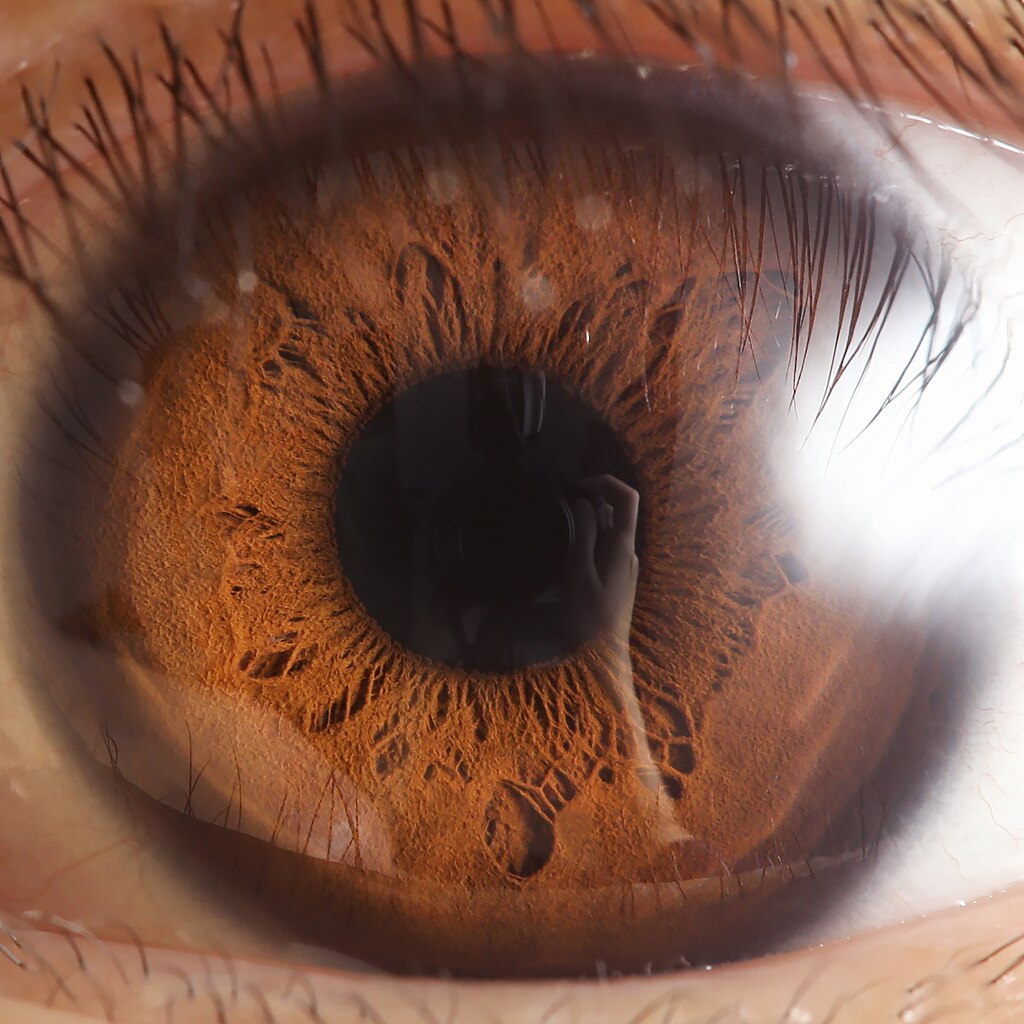
What happens during a session: After reviewing your eye and skin history, your clinician places protective shields and positions the applicator. The system warms the eyelids to a precise temperature and applies timed pulses of pressure. This melts and expresses blocked oil right where the problem starts—the meibomian glands along the lid margin. The treatment does not shine light into the eye or change the shape of the eye. The FDA classifies eyelid thermal pulsation as a prescription medical device that applies localized heat and pressure therapy to adult eyelids for MGD. 3 Most patients also continue simple home care—warm compresses, lid cleansing, and artificial tears—as part of a stepwise plan.
Options and add-ons: Several FDA-cleared systems deliver heat and pressure in different ways. Your eye doctor chooses settings based on your lids, skin type, and exam. Some clinics combine the device treatment with manual gland expression at the same visit; others pair thermal pulsation with anti-inflammatory drops or in-office eyelid cleaning if buildup is present. The goal is the same: freer-flowing oil, steadier tears, and more comfortable eyes. 4
Who Is a Candidate?
Often a good fit: Adults with evaporative dry eye from MGD who still have burning, stinging, fluctuating vision, or eyelid redness despite regular home care (warm compresses, lid hygiene, preservative-free tears). Your doctor will confirm MGD at the slit lamp and may test the tear film and gland function before recommending a procedure. 4 Independent evidence reviews also describe benefits after a short series of treatments in selected adults.
Who may need a different plan or adjusted settings: People with active eye infections, recent eyelid surgery, open skin lesions in the treatment area, or certain photosensitive skin conditions may need to wait or use alternative care first. Your clinician will also consider pregnancy, medicines, and skin tone when choosing device settings or deciding if the treatment is right for you. 5
Is Thermal Pulsation a Good Fit for Me?
Select your details to estimate suitability.
Cost and Price
How clinics package it: Thermal pulsation is commonly offered as a single in-office treatment per eye, often with a follow-up visit to check results. Some people choose a maintenance session months later if symptoms return. Evidence summaries describe short treatment courses (e.g., a single ~12-minute session in some trials) with benefits on tear stability and gland output. Ask your clinic whether manual expression is included and how follow-ups are billed. 5
Paying for care: Coverage varies by plan and region. Many insurers consider thermal pulsation a procedure for dry eye due to MGD and may require documentation of medical necessity and prior conservative care. Because dry eye also drives indirect costs (missed work, repeated purchases of drops/compresses), some families view an effective procedure as part of the overall cost picture.
Smart budgeting checklist to request from your clinic:
- Itemized estimate: evaluation, the procedure per eye, whether gland expression is included, and follow-up visits.
- Maintenance policy: typical timing and price if symptoms return later.
- Insurance help: what documentation your plan needs; whether HSA/FSA funds can be used.
- At-home supplies: budget for preservative-free tears, lid cleansers, and warm compress masks to support results.
Bring a short symptom diary (good and bad days, screen time, environment). It helps you and your clinician decide if and when a maintenance session will add value. 6
Benefits and Limitations
Benefits seen in studies:
- Improved meibomian gland output and increased tear breakup time.
- Reduced dryness symptoms compared with no treatment or standard warm compresses in selected adults.
- Randomized/controlled studies over the last decade support improvements after a short session, with some durability over months. 8
Limits to understand: Results vary. Thermal pulsation is not a cure; glands can clog again over time, and many people benefit from ongoing home care or later maintenance. Temporary side effects may include mild redness, lid tenderness, or light sensitivity on the treatment day. Serious complications appear uncommon when devices are used properly, but your clinician will review risks and aftercare based on your lids and skin. 7
Recovery and Long-Term Care
Right after treatment: Most people return to normal activities the same day. Your team will share simple aftercare—keep the skin clean, avoid heavy sun and harsh products for a short period, and call if you notice unusual pain, discharge, or sudden vision change. Ongoing symptoms usually fade over days as oils flow better and the tear film stabilizes. 1
Habits that help results last:
- Warm compresses and gentle lid hygiene to keep oils moving.
- Preservative-free tears as needed; blink breaks during screen time; consider a humidifier at home or work.
- Sunglasses outdoors for wind/sun protection; manage allergy or rosacea triggers if they worsen your lids.
- Bring all eye drops and products to follow-ups so your clinician can simplify your plan and avoid duplicates.
Your doctor will set a follow-up schedule and, if needed, suggest when a maintenance session might make sense for your symptom pattern. 4
Latest Research & Innovations
What recent evidence says: Over the last 10–15 years, research has expanded understanding of how thermal pulsation helps MGD. A 2024 systematic review in Contact Lens and Anterior Eye notes that comparative-effectiveness evidence is still developing and calls for more high-quality trials and standardized protocols—useful context when setting expectations. 11
A 2024 narrative review summarizes real-world outcomes, durability, and safety across many studies, supporting use in selected adults and guiding discussions on maintenance. 8
Professional guidance places thermal pulsation within a broader, stepwise dry eye plan that also treats eyelid inflammation and tear evaporation.
Recent Peer-Reviewed Research
Interventions for Dry Eye: An Overview of Systematic Reviews.
McCann P, Kruoch Z, Lopez S, et al.
Thermal Pulsation in the Management of Meibomian Gland Dysfunction and Dry Eye: A Report by the American Academy of Ophthalmology.
Tao JP, Shen JF, Aakalu VK, et al.
Effects of Vectored Thermal Pulsation on Objective Tear Film Measures.
Fallah S, Loer CJ
Next Steps
If your eyes feel dry or sandy, or your vision fluctuates with screens, start with a full eye exam. Ask whether MGD is part of your dry eye and whether thermal pulsation could help alongside daily lid care. Testing may include tear breakup time, gland evaluation, and surface staining to track progress. 10 Bring a short symptom diary and list of current drops to your visit so your plan fits your schedule, budget, and goals. 4
Who to see: a Cornea/External Disease ophthalmologist or an optometrist experienced in ocular surface disease. Together, you’ll decide on the right mix of home care, in-office therapy, and follow-up to keep your eyes comfortable day to day.