Blepharitis
also known as Eyelid Inflammation
Last updated July 28, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.



Overview
Blepharitis is a common, chronic inflammation of the eyelid margins. It often flares in cycles, leaving lids red, itchy, and coated with oily scales that cling to the eyelashes. Although uncomfortable, the condition rarely threatens vision. Blepharitis can be broadly classified as anterior (affecting the lash line) or posterior (linked to meibomian‑gland dysfunction). Regular lid hygiene is the mainstay of control—much like brushing your teeth to prevent gingivitis. Because the disease is multifactorial, management usually combines self‑care with medications when needed. Blepharitis is not contagious, but it can persist for life without consistent treatment 1 2
Symptoms
- Burning, gritty, or stinging eyes—often worse on waking
- Itchy or swollen eyelids with greasy flakes at the lash base
- Crusting that can glue the lids together overnight
- Watery or red eyes; intermittent blurred vision that clears with blinking
- Light sensitivity and a sensation of “something in the eye”
Symptoms tend to wax and wane. People with rosacea, dandruff, or dry eye often notice more frequent flare‑ups 2 3
Causes and Risk Factors
Blepharitis results from a mix of factors:
- Bacterial biofilm—especially Staphylococcus species that thrive at the lash roots and trigger inflammation.
- Meibomian‑gland dysfunction (MGD)—thickened oils block gland outlets, destabilizing the tear film.
- Skin conditions such as seborrheic dermatitis and rosacea.
- Demodex mites that live in lash follicles and feed on oils.
- Environmental factors: contact‑lens wear, heavy makeup use, and low‑humidity workspaces.
Age > 50 years, oily complexions, and a family history of rosacea also raise risk 1 4
Blepharitis Flare‑Risk Estimator
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
Your eye‑care provider will:
- Review symptoms and health history (e.g., rosacea, dandruff, allergies).
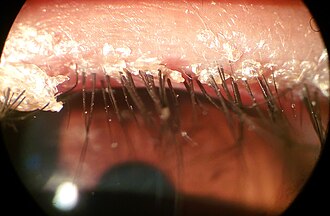
- Examine lids and lashes under magnification, looking for collarettes (cylindrical dandruff), capped glands, or mites.
- Gently press the meibomian glands to assess oil quality.
- Check tear‑film stability and ocular‑surface staining.
In stubborn or atypical cases, cultures, lash‑scrapings, or biopsy help rule out infection, cancer, or autoimmune disease 3 4
Treatment and Management
Daily lid hygiene is the cornerstone:
- Apply a warm compress for 5‑10 minutes.
- Massage lids to express oils.
- Clean lash margins with diluted baby shampoo or commercially prepared lid wipes.
Other options include:
- Topical antibiotics (e.g., azithromycin, bacitracin) for bacterial overgrowth.
- Short courses of steroid drops/ointments for acute inflammation.
- Oral tetracyclines to reduce meibomian inflammation in rosacea.
- In‑office thermal pulsation or intense‑pulsed‑light therapies for MGD.
- Lotilaner 0.25 % eye drops (Xdemvy)—FDA‑approved in 2023 as the first Rx targeting Demodex mites.
Consistent routines usually control symptoms; stopping care can trigger relapse 2 5 6
Living with Blepharitis and Prevention
Because blepharitis tends to recur, think of eyelid care as part of your daily routine:
- Commit to twice‑daily warm compresses and lid scrubs—even when eyes feel normal.
- Replace eye makeup every 3‑4 months and skip mascara during flare‑ups.
- Use preservative‑free lubricating drops to ease dryness.
- Blink often when using screens, and keep humidity ≥ 40 % indoors.
- Manage underlying skin conditions with your dermatologist.
Good hygiene dramatically cuts flare frequency and keeps vision comfortable 1 3
Latest Research & Developments
Recent studies explore novel therapies that go beyond hygiene:
- Lotilaner ophthalmic solution 0.25 % showed significant mite eradication and symptom relief in the SATURN‑1 and SATURN‑2 Phase 3 trials, supporting FDA approval in 2023 6.
- Thermal pulsation systems continue to evolve, delivering controlled heat and pressure to improve meibomian‑gland flow, with long‑term studies demonstrating sustained tear‑film benefits 5.
Ongoing research is investigating probiotics, omega‑3 supplements, and low‑dose intense‑pulsed‑light to modulate ocular‑surface inflammation.
Recently Published in Peer-Reviewed Journals
American journal of ophthalmology
May 30, 2025
TFOS DEWS III Diagnostic Methodology.
Wolffsohn JS, Benítez-Del-Castillo J, Loya-Garcia D, et al.
American journal of ophthalmology
December 1, 2024
Ophthalmic Immune-Related Adverse Events and Association with Survival: Results From a Real-World Database.
Quiruz L, Yavari N, Kikani B, et al.
BMC ophthalmology
November 18, 2024
BlephEx-treatment for blepharitis: a prospective randomized placebo-controlled trial.
Siegel H, Merz A, Gross N, et al.
Next Steps
If home care is not enough, schedule an appointment with an ophthalmologist—preferably a cornea and external‑disease specialist. They can:
- Confirm the diagnosis and rule out mimicking conditions.
- Tailor a medication plan (antibiotics, anti‑inflammatories, or mite‑directed therapy).
- Recommend in‑office procedures for stubborn meibomian‑gland blockages.
You can locate the right specialist through your primary‑care provider or by using professional directories. Kerbside can also help connect you directly with a qualified eye‑care professional in your area and streamline scheduling.
Bring a list of symptoms, prior treatments, and current medications to maximize the visit 2 3
