Corneal Abrasion
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.


Overview
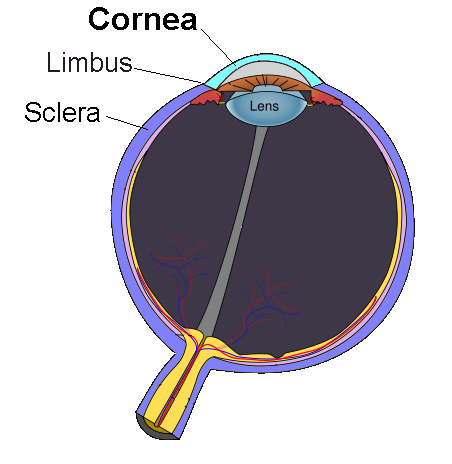
A corneal abrasion is a scratch or scrape on the cornea — the clear, dome-shaped “windshield” that focuses light into your eye. Because the cornea contains more sensory nerve endings than almost any other tissue in the body, even a hairline defect can feel dramatic. Most superficial scratches heal in one to three days, but deeper injuries can scar, trigger infection, or permanently blur vision if treatment is delayed.1 Globally, corneal trauma is among the top causes of preventable monocular blindness, underscoring the importance of prompt evaluation.2
The cornea also acts as a barrier against dirt, germs, and chemicals. A breach offers microbes a doorway to the delicate inner eye, so clinicians focus on both closing the scratch and preventing microbial keratitis—an aggressive infection that can develop within 24 hours. Standard care combines preservative-free lubrication to speed epithelial migration, a topical antibiotic to curb infection risk, and pain control so patients avoid rubbing the eye.3
Symptoms
Symptoms often appear within minutes and can be severe even for tiny abrasions:
- Sudden sharp pain that worsens with blinking
- Foreign-body sensation (the feeling something is in the eye)
- Redness and excessive tearing
- Blurred or hazy vision
- Light sensitivity (photophobia)
- Headache or eyelid twitching
Pain that intensifies over 12 hours, thick discharge, or a sudden drop in vision can signal infection or a deeper wound and requires same-day ophthalmic care.45
Causes and Risk Factors
Almost anything that touches the ocular surface can cause an abrasion, but common culprits include:
- Traumatic objects — fingernails, make-up brushes, paper edges, pet claws, plant branches.
- Foreign bodies — wind-blown sand, metal filings, sawdust.
- Contact-lens misuse — sleeping in lenses or poor hygiene.6
- High-velocity particles from grinding, mowing, or welding without ANSI-approved eyewear.
- Dry-eye disease or incomplete eyelid closure (lagophthalmos).
Sports such as basketball, racquetball, and hockey also rank high for ocular injuries; properly fitted polycarbonate sports goggles dramatically cut risk.7 A 2024 review found that eye protection prevented up to 90 % of game-related corneal abrasions.8
Personal Corneal Abrasion Risk Score
Select your details to estimate risk factors.
Diagnosis
An eye-care professional will:
- Take a focused history (mechanism, timing, contact-lens use).
- Instill anesthetic drops to allow gentle eyelid opening.
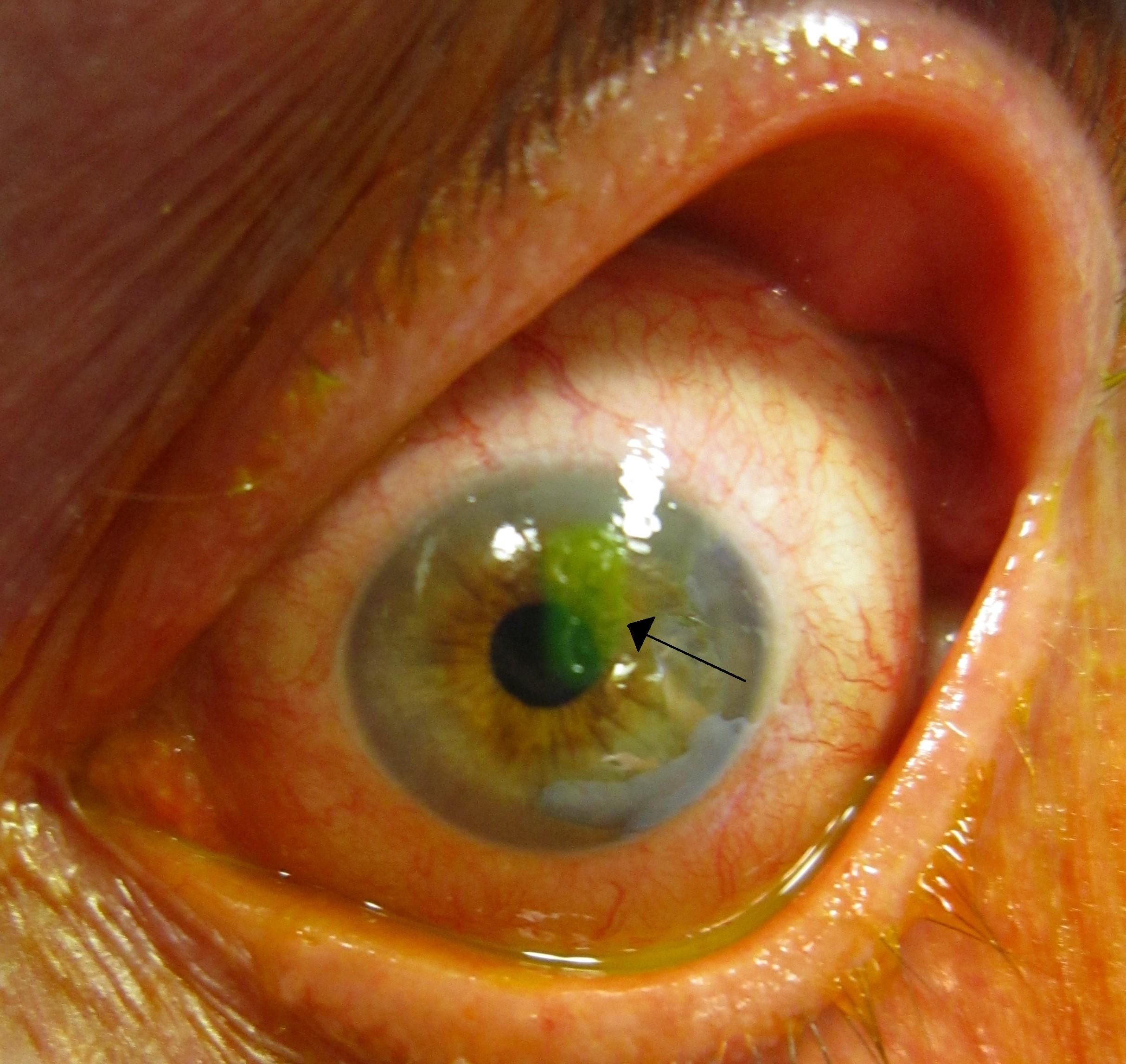
- Apply fluorescein dye; under blue light, the scratch glows bright green.
- Invert the upper lid to rule out a trapped foreign body.
- Use slit-lamp biomicroscopy to gauge size, depth, and location.
Defects limited to the epithelium and <6 mm usually heal rapidly; deeper or central lesions, organic-matter injuries, or those in contact-lens wearers warrant daily follow-up and sometimes cultures.39
Treatment and Management
Goals: speed re-epithelialization, prevent infection, relieve pain.
1. Lubrication
Preservative-free artificial tears every 1–2 hours reduce lid–wound friction and facilitate healing.
2. Antibiotic prophylaxis
Broad-spectrum topical antibiotics (e.g., erythromycin ointment or moxifloxacin drops) 4–6× daily until the defect closes.10
3. Pain control
Oral NSAIDs, short-course topical NSAIDs, or cycloplegic drops reduce ciliary spasm. A bandage contact lens can halve pain but necessitates close monitoring.
4. Tetanus update
Give if wound caused by soil-contaminated object and vaccination is outdated.
5. Follow-up
Re-examine within 24 hours; 90 % of simple abrasions close by then. Non-healing defects may indicate retained foreign body, irregular edges, or early infection requiring fortified antibiotics or amniotic-membrane therapy.11
Living with Corneal Abrasion and Prevention
During healing, avoid eye rubbing, contact lenses, and eye make-up. Wear sunglasses if light hurts. To prevent future abrasions:
- Protective eyewear: ANSI Z87.1 safety glasses prevent up to 90 % of occupational eye injuries.
- Contact-lens hygiene: Replace cases every three months, rub-and-rinse lenses, never swim or shower in lenses.
- Treat dry eye: Warm compresses, omega-3 supplements, and prescription anti-inflammatories reduce friction-related micro-abrasions.
Latest Research & Developments
Innovations aim to accelerate healing and minimize complications:
- Recombinant lubricin drops cut epithelial-closure time by ~30 % in a 2023 randomized trial.14
- Smart bandage lenses embedded with antibiotic-growth-factor micro-reservoirs received $6.7 million in new NEI funding to enter phase II trials.15
- Limbal stem-cell patches are being tested for recurrent erosion, with early reports of reduced episodes and better vision.
- Handheld anterior-segment OCT now allows bedside measurement of defect depth within microns, guiding more tailored therapy.
Recent Peer-Reviewed Research
Global Burden of Eye Injuries in Children and Adolescents, 1990 to 2021: A Systematic Analysis From the Global Burden of Disease Study.
Sun G, Luo H, Ran Q, et al.
Inhibitor of DNA-Binding 3 Is a Novel Regulator of Limbal Epithelial Cell Migration Via the EphA2/Akt Signaling Pathway.
Clutter ED, Yang W, Han J, et al.
Deep Corneal Nerve Plexus Selective Damage in Persistent Neurotrophic Corneal Epithelial Defects Detected by In Vivo Multiphoton Confocal Microscopy.
Komai S, Quiroga-Garza ME, Ruiz-Lozano RE, et al.
Next Steps – Finding the Right Care
Best specialist: a cornea and external-disease ophthalmologist. They have high-magnification microscopes, debridement tools, and access to advanced biologic therapies.
Scheduling tips: Start with urgent care or an optometrist for initial evaluation; ask for an expedited cornea referral if pain worsens after 24 hours, vision declines, or the injury involves contact-lens wear. Many hospital-based eye institutes reserve same-day “cornea walk-in” slots for acute injuries.12