Dry Eye Syndrome
also known as Dry Eye Disease, Keratoconjunctivitis Sicca
Last updated July 26, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.
Overview
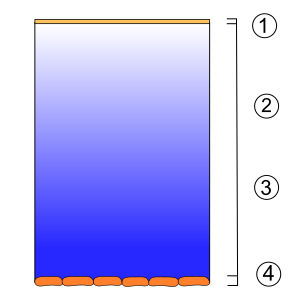
Dry Eye Syndrome (also called dry eye disease or keratoconjunctivitis sicca) happens when your eyes either don’t make enough tears or produce poor-quality tears. A healthy tear film has three layers—lipid, aqueous and mucin—that work together to keep the eye’s surface smooth, clear and protected. When any layer is out of balance, the ocular surface becomes inflamed and the eyes feel irritated or gritty.1 The condition is remarkably common: about 16 million U.S. adults report symptoms, and prevalence climbs with age and screen use.2 Although rarely sight-threatening, untreated dry eye can cause blurred vision, recurrent infections and damage to the cornea. Early recognition and tailored treatment keep most people comfortable and seeing clearly.3
Symptoms
- Stinging, burning or scratchy sensation
- Feeling of sand or grit in the eye
- Intermittent blurred or fluctuating vision
- Stringy mucus or contact lenses that pop out
- Excessive reflex tearing that runs down the cheek
- Light sensitivity or eye fatigue after reading or screen time
These symptoms often worsen in air-conditioned spaces, windy environments or during prolonged digital work.4 Many patients notice temporary relief when they blink or close their eyes, because blinking helps spread tears evenly across the surface.5
Causes and Risk Factors
Dry eye has multiple overlapping causes:
- Age > 40 yrs and female sex—post-menopausal hormonal changes reduce tear quantity and quality.2
- Meibomian gland dysfunction (MGD)—clogged oil glands cause tears to evaporate faster.5
- Auto-immune disorders such as Sjögren syndrome, rheumatoid arthritis and lupus impair tear glands.6
- Environmental/behavioral—extended screen use, contact-lens wear, low-humidity climates, smoke or air pollution.
- Medications—antihistamines, antidepressants, acne drugs, hormone therapy and some glaucoma drops.
An eye-care specialist will tease out which factors are driving your symptoms so treatment can be targeted.
Dry Eye Risk Score
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
Your provider starts with a symptom survey and a slit-lamp exam. Common office tests include:
- Schirmer test – a paper strip measures tear production in five minutes.4
- Tear-film breakup time (TBUT) – fluorescein dye reveals how quickly tears evaporate.
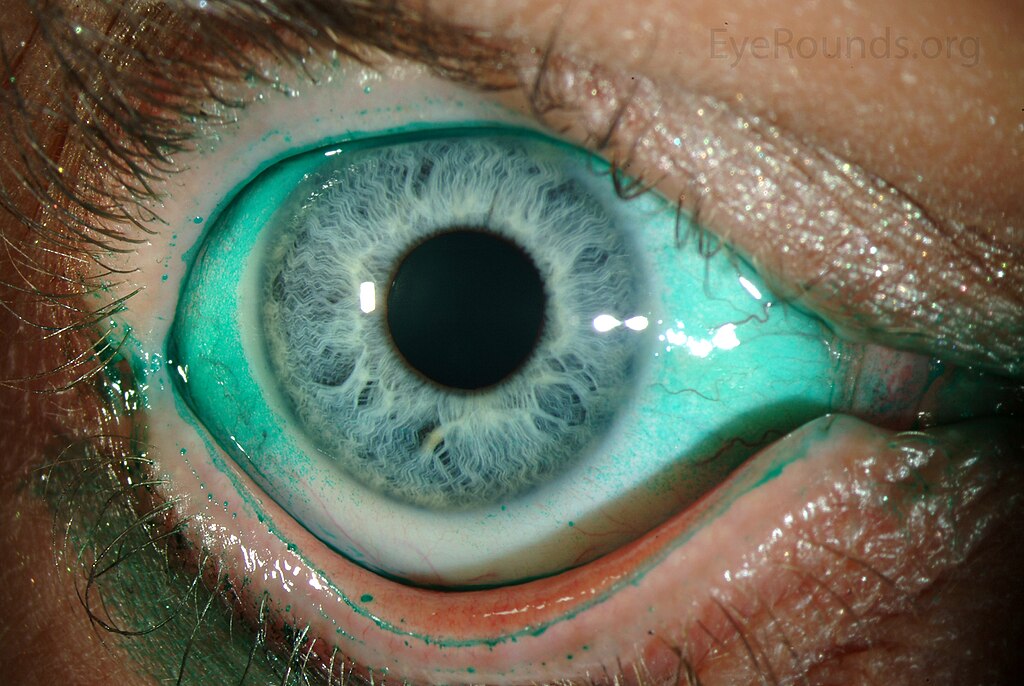
- Lissamine green staining – highlights damaged conjunctival cells (see Image 2).
- Point-of-care osmolarity or MMP-9 testing – detects inflammatory markers.
Advanced clinics may offer infrared meibography or ocular surface interferometry to visualize oil glands and lipid layer thickness.5
Treatment and Management
Most patients improve with a step-wise approach:
- Artificial tears (preservative-free if used >4×/day) and lubricating ointment at night.
- Warm compresses + lid massage to melt clogged oils.
- Omega-3 fatty-acid supplements and good hydration.
- Prescription therapies—cyclosporine 0.05 % (Restasis), lifitegrast 5 % (Xiidra) or varenicline nasal spray (Tyrvaya). Tyrvaya stimulates the trigeminal parasympathetic pathway to boost natural tear flow and was FDA-approved in 2021.8
- Punctal plugs or cautery to reduce tear drainage.
- Light-based therapies (IPL, radiofrequency) for stubborn meibomian blockage.
Your eye doctor will tailor the plan and review medications that might be worsening dryness.3
Living with Dry Eye Syndrome and Prevention
You can take charge daily:
- Follow the 20-20-20 rule: every 20 minutes, look 20 feet away for 20 seconds.
- Position screens slightly below eye level so the lids cover more surface.
- Add a humidifier, avoid fans blowing directly on the face and wear wrap-around glasses outdoors.
- Blink consciously, especially while scrolling.
- Stay hydrated and eat fatty-fish or flaxseed rich in omega-3s.
These simple habits, plus regular check-ins, reduce flare-ups and protect vision.81
Latest Research & Developments
Research is moving beyond simple lubrication. Highlights include:
- Neuro-stimulation therapies like Tyrvaya nasal spray, which use nicotinic-cholinergic pathways to trigger endogenous tearing.8
- Sustained-release cyclosporine inserts that sit in the canaliculus and free patients from daily drops.
- Autologous platelet-rich plasma and regenerating agent (RGTA) eye drops aimed at corneal healing.
- NIH-funded teams are studying gene-edited goblet-cell replacements and topical biologics that block inflammatory cascades.10
- Public-health data link rising screen time to earlier-onset dry eye, fueling ergonomic campaigns.8
Recently Published in Peer-Reviewed Journals
American journal of ophthalmology
July 9, 2025
Advancing Myopia Management: The Therapeutic Potential of Microbiota-Targeted Interventions.
Zhao L, Xie Y, Chen W, et al.
Investigative ophthalmology & visual science
July 1, 2025
Association of Human Leukocyte Antigen Polymorphisms With Moderate-to-Severe Dry Eye With and Without Sjögren's Syndrome.
Chen Z, Jiang D, Zheng Q, et al.
American journal of ophthalmology
June 27, 2025
A novel comparative study of inflammatory cytokines through non-invasive tear analysis in children with myopia versus emmetropia.
Nishanth S, Bauer NJ, Shetty R, et al.
Next Steps
Best specialist to see: Cornea & External Disease ophthalmologist
These eye-care subspecialists focus on the ocular surface and tear film. Ask your optometrist or primary-care doctor for a referral, or use our online scheduler to book directly. Bring a list of symptoms, current drops and medications to your first visit so we can personalize your care plan. If appointments are limited in your area, request a tele-triage to start treatment sooner—then follow up in person for detailed testing.
Ready for relief? Connect with our board-certified cornea specialists below and take the first step toward comfortable, clear vision.
