Direct Selective Laser Trabeculoplasty
also known as Direct SLT, DSLT
Last updated August 6, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.

Overview
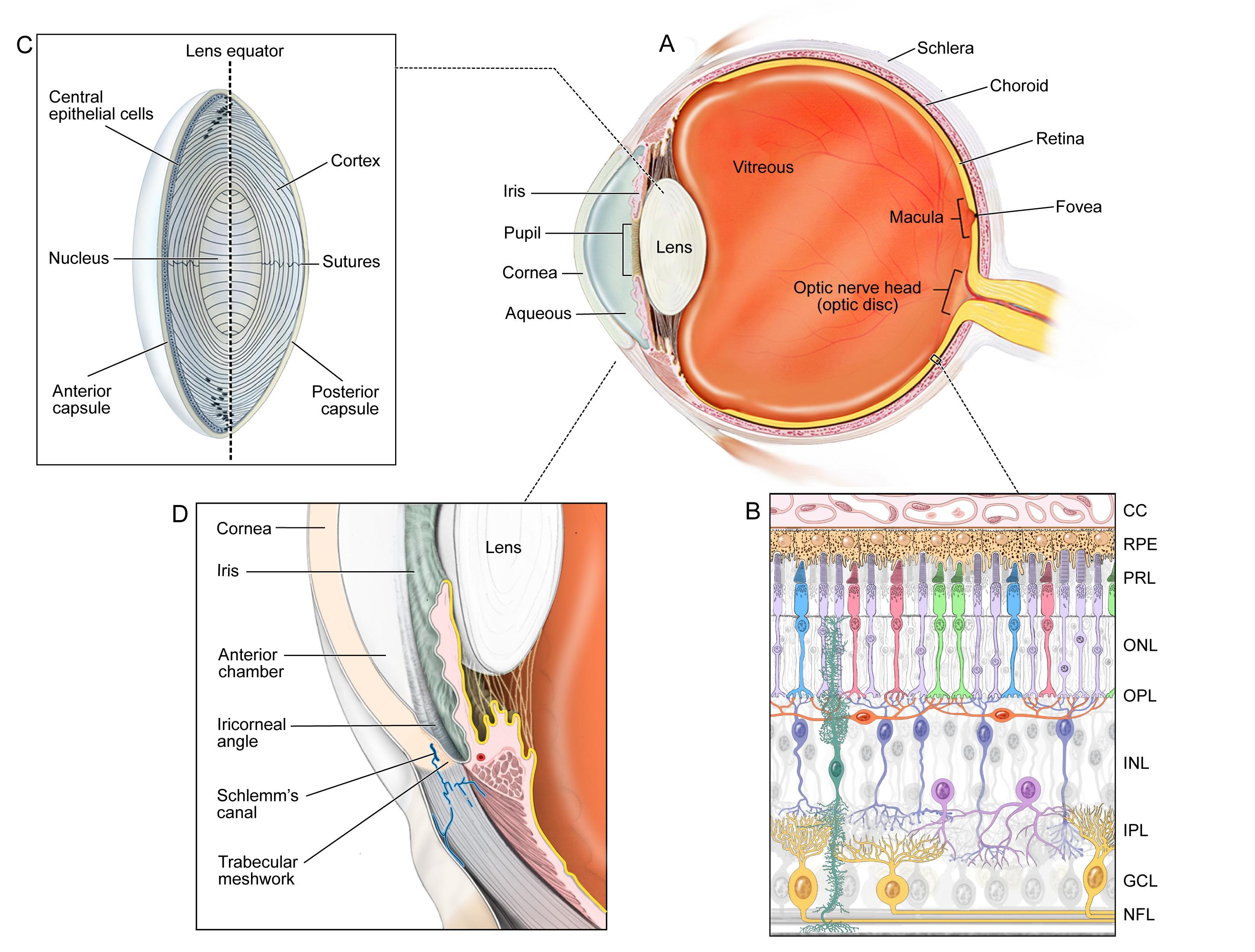
Direct Selective Laser Trabeculoplasty (DSLT) is a new, automated form of laser therapy that lowers eye pressure without touching the eye. The device delivers many gentle laser pulses straight through the limbus, aiming at the trabecular meshwork in a single 1‑to‑3‑second burst. Because no contact lens or gonioscopy is needed, the treatment is quicker and more comfortable than traditional SLT, making it easier to offer in busy clinics. Early studies show an average 25–30 % drop in intra‑ocular pressure (IOP), comparable to conventional SLT and better than a single glaucoma drop for many patients.12
How the Procedure Works & Options
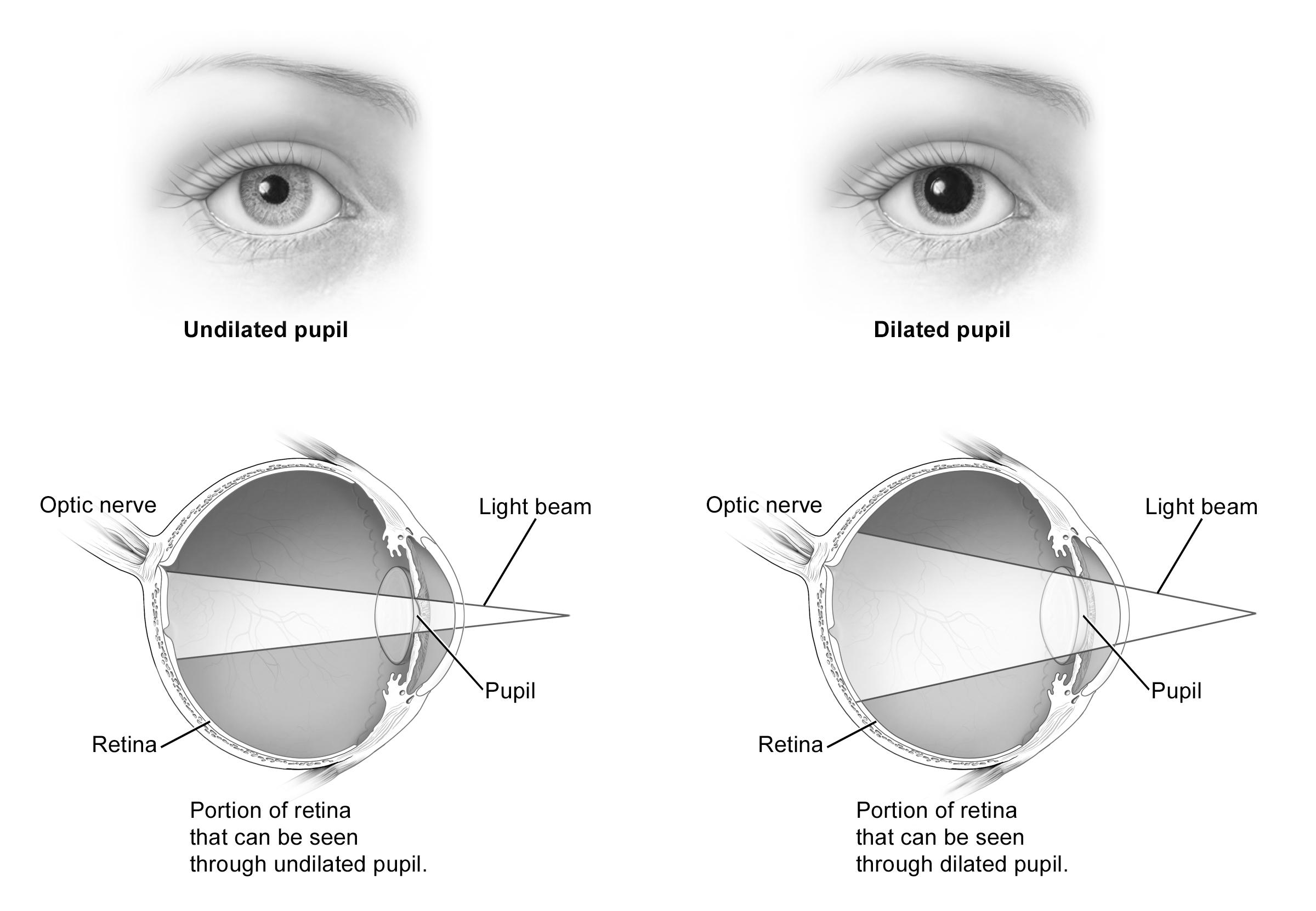
DSLT uses a low‑energy, 532‑nm, Q‑switched Nd:YAG laser. An eye‑tracking camera maps the angle, then the system fires about 100 micro‑pulses in a circular pattern through the clear cornea and sclera. The laser selectively activates pigment‑rich cells in the trabecular meshwork, prompting biologic changes that clear debris and widen outflow channels. Treatment covers 360° of the drainage tissue and is fully automated—no rotation of a contact lens is required.
The main commercially available platform is the Eagle system. Current clinical protocols include full‑circle DSLT as first‑line therapy and “re‑DSLT” if pressure rises again, similar to repeat SLT.34
Who Is a Candidate?
Adults with primary open‑angle glaucoma or ocular hypertension whose iridocorneal angles are open are prime candidates. DSLT is also being studied for some angle‑closure eyes after laser iridotomy. It suits people who:
- Struggle with daily eye‑drop schedules or cost
- Need extra IOP lowering on top of drops
- Prefer a non‑contact procedure
Eyes with active inflammation, neovascular glaucoma, or severely scarred angles are not good candidates. Early prospective data suggest that darker trabecular pigmentation and higher baseline IOP predict better pressure reduction.56
DSLT Suitability Score
Enter your details below to check your suitability for this treatment
Suitability Level
Recommendation
Benefits and Limitations
Key benefits
• Rapid, no‑touch treatment finished in seconds.
• Lowers IOP by roughly 25–30 %, delaying or replacing drops for many patients.
• Automated energy delivery reduces operator error.
Limitations
• Long‑term durability is still under study; retreatment may be needed in 3–5 years.
• Insurance coverage is expanding but not yet universal.
• Eyes with very light angle pigmentation may respond less.
The GLAUrious multicenter trial found DSLT non‑inferior to conventional SLT at six months, with similar IOP reduction and fewer transient pressure spikes.78
Risks and Side Effects
DSLT’s safety record is excellent. Mild redness, light sensitivity, or scratchy sensation can occur but usually fade within a day. Because no contact lens is used, the risks of corneal abrasion and infection are lower than with SLT. Rarely, a transient IOP spike may happen, so doctors check pressure within two hours.
Serious complications like sustained inflammation or peripheral anterior synechiae are uncommon. A short course of anti‑inflammatory drops is often prescribed to keep the eye comfortable.910
Recovery and Long‑Term Care
Most people return to normal activities the same day. Typical follow‑up steps are:
- Pressure check 1–2 hours after treatment
- Office visit at 4–6 weeks to judge full effect
- Routine glaucoma checks every 3–6 months
Existing eye‑drop plans are continued or tapered depending on the IOP response. If pressure creeps up over time, DSLT can be repeated, or other options like minimally invasive glaucoma surgery (MIGS) can be added.1112
Latest Research & Innovations
Investigators are refining energy‑dose algorithms and eye‑tracking software to enhance consistency. The ongoing TANGO and GLAUrious randomized trials continue to compare DSLT with standard SLT over several years. Imaging biomarkers, such as baseline Schlemm’s canal caliber, are being explored to predict who will respond best.
Future prototypes aim to integrate DSLT into routine screening devices, so a single machine could detect high IOP and treat it in one sitting—opening the door to mass prevention programs.1314
Next Steps
If you have rising eye pressure or glaucoma, meeting with a glaucoma specialist is the safest way to learn whether DSLT fits your needs. The doctor will review your pressure history, angle anatomy, and lifestyle demands to craft a personalized plan. You can connect with the right specialist through Kerbside and take proactive steps to protect your vision for life.
Bringing your current eye‑drop list and recent pressure readings will make the consultation even more productive.1516


