Neovascular Glaucoma
also known as NVG
Last updated September 5, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.

Overview
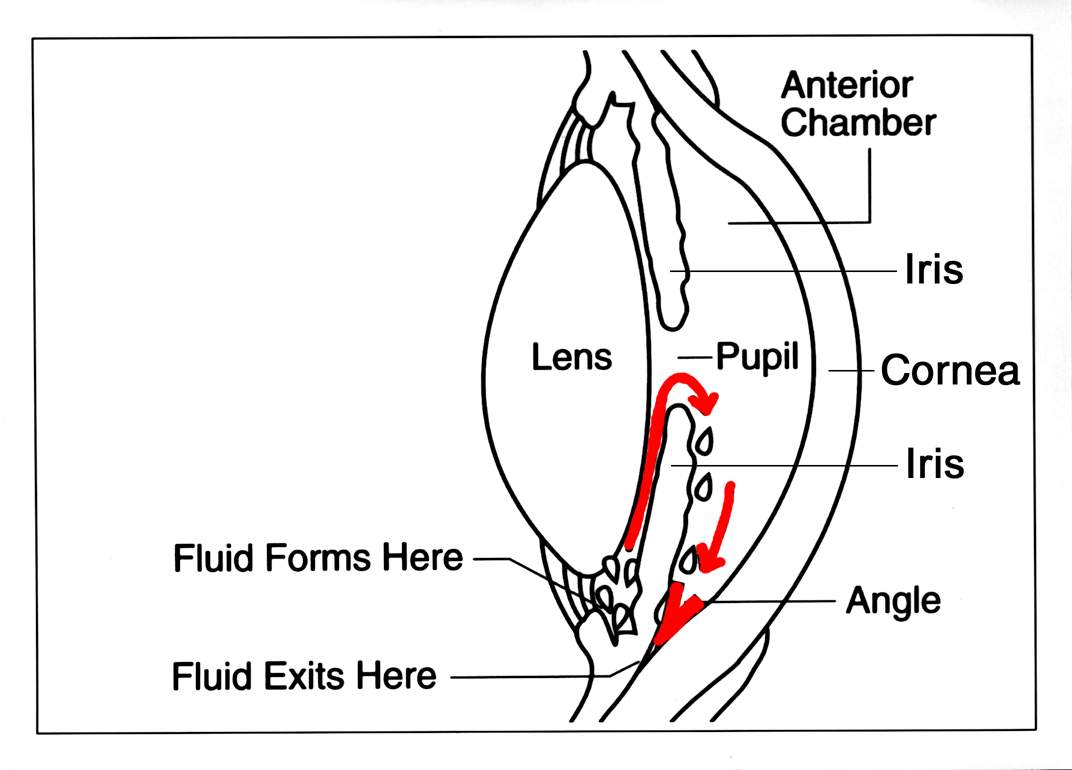
Neovascular glaucoma (NVG) is a serious glaucoma that occurs when abnormal new blood vessels grow on the iris (colored part of the eye) and in the drainage angle. These fragile vessels signal poor retinal oxygen supply and can form a scar-like membrane that blocks the drain, raises eye pressure, and damages the optic nerve. NVG is most often caused by another eye problem (e.g., advanced diabetic eye disease or severe retinal vein occlusion), can progress quickly, and may be painful—so prompt treatment is critical. 1
Because NVG begins with retinal ischemia (too little blood flow), care focuses on treating the retina and lowering eye pressure to protect vision. With timely retinal laser, anti-VEGF medicines, and sometimes surgery, many people can control disease and pain. 4
Symptoms
NVG may start quietly but often becomes noticeable as pressure rises.
- Eye pain, redness, and light sensitivity
- Blurred vision or sudden vision drop; halos around lights
- Headache
- Sometimes blood in the front of the eye (hyphema)
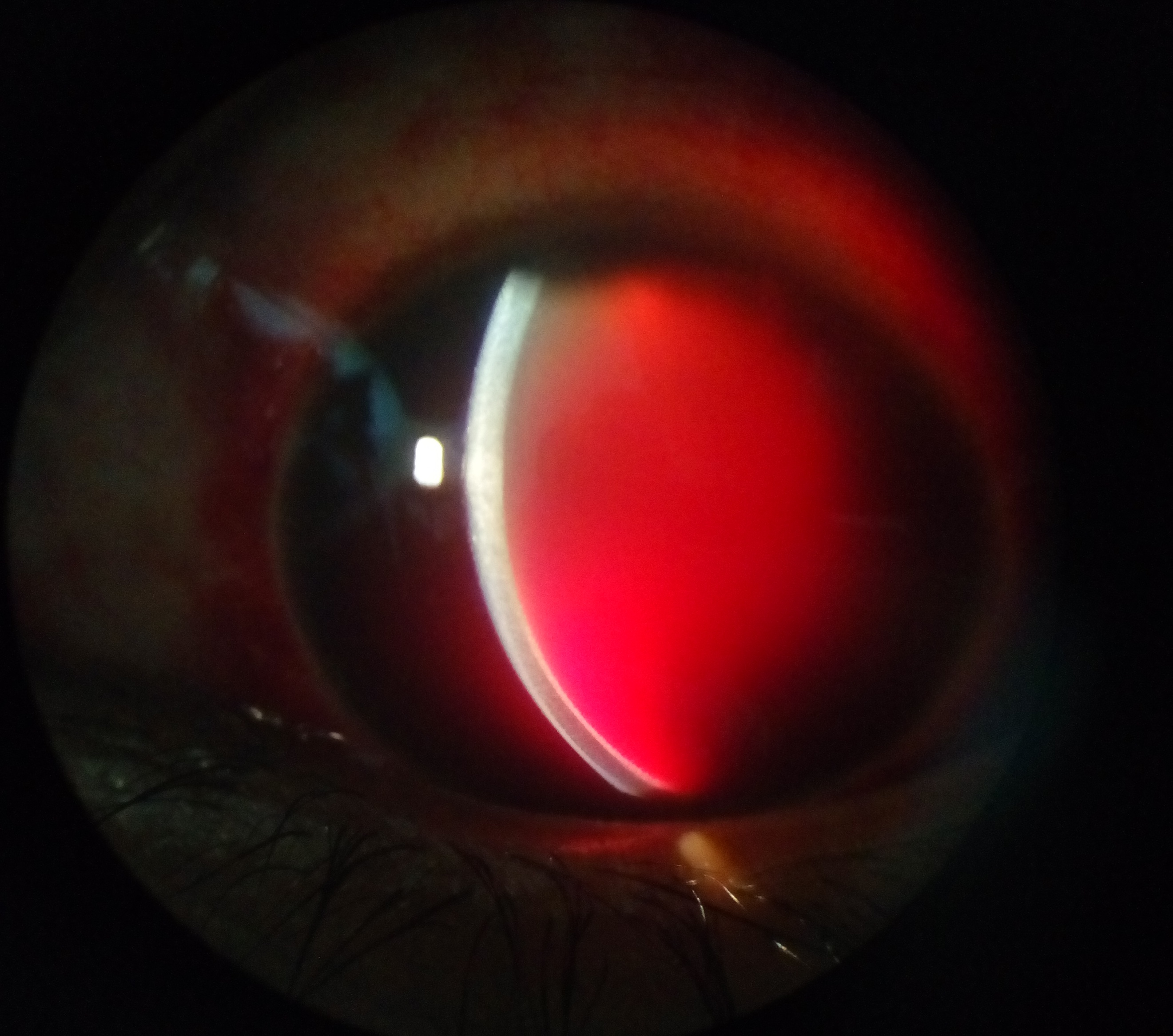
These symptoms need urgent care. Exams may show fine new vessels on the iris (rubeosis) and in the angle where fluid drains. 1 Patient-friendly glaucoma education explains why pressure control and follow-up are essential. 3
Causes and Risk Factors
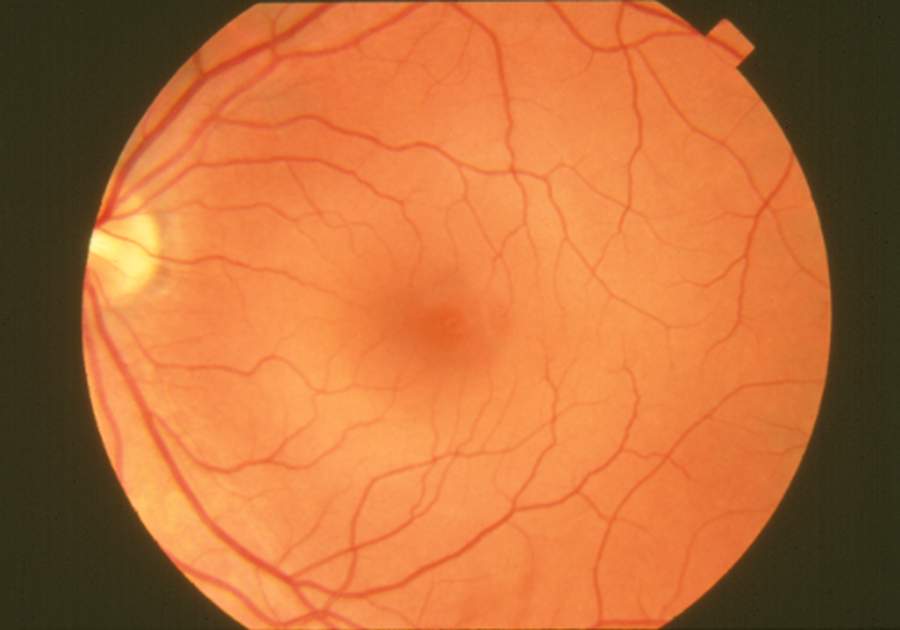
NVG is usually a secondary glaucoma, developing because another eye disease starves the retina of oxygen. Ischemic retina releases signals (e.g., VEGF) that drive abnormal vessel growth in the front of the eye.
Common causes:
- Proliferative diabetic retinopathy (PDR)
- Central or hemi-central retinal vein occlusion (CRVO/HRVO)
- Ocular ischemic syndrome (very poor ocular blood flow)
Additional risks include long-standing uncontrolled diabetes, hypertension, and delayed care after a vein occlusion. Severe RVO can lead to anterior segment neovascularization and NVG. 1 9
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
Diagnosis is made by an eye specialist after a complete exam.
- Slit-lamp exam: fine iris vessels (rubeosis), hyphema
- Gonioscopy: new vessels or fibrous membrane closing the angle
- Eye pressure (IOP) checks: often repeated
- Dilated retinal exam & imaging: diabetic changes or vein occlusion; OCT and fluorescein angiography as needed
- Visual field & optic nerve imaging: to assess damage
These tests confirm NVG, uncover the cause, and guide treatment urgency. 1 8
Treatment and Management
Care targets two goals: (1) treat ischemic retina to stop the drive for new vessels and (2) lower IOP to protect the nerve and relieve pain.
Treat the retina
- Panretinal photocoagulation (PRP): Laser to the peripheral retina reduces oxygen demand and helps abnormal vessels regress; may be done during vitrectomy or after pressure control if media is cloudy. 2
- Anti-VEGF injections (e.g., bevacizumab): Often used early to shrink vessels quickly and enable PRP or surgery; short-term repeats may be needed. 5
Lower the pressure
- Drops and pills: Aqueous suppressants (beta-blockers, alpha-agonists, carbonic anhydrase inhibitors); steroid and cycloplegic drops for inflammation/pain. Medications alone are often insufficient in NVG.
- Laser & surgery: If IOP remains high, many require a glaucoma drainage implant (tube shunt) or cyclophotocoagulation (CPC). Tube shunts (valved or non-valved) are frequently chosen because they can work despite scarring. 2
Costs & practical tips
- Clinic lasers (PRP, CPC): Usually outpatient; request a pre-estimate (facility + physician fees) and check deductible/coinsurance.
- Anti-VEGF injections: Costs vary by drug/site; ask about buy-and-bill vs. pharmacy-supplied meds, prior authorization, and assistance programs.
- Tube shunt surgery: Depends on implant type, site, and anesthesia; request itemized in-network quote and ask about global period/post-op coverage.
- Medicines: Bring your formulary; ask about generics, 90-day fills, and savings cards where appropriate.
Daily habits: Take drops exactly as prescribed, keep every follow-up, control blood sugar and blood pressure, and call promptly if pain or vision worsens. 5
Living with Neovascular Glaucoma and Prevention
NVG is challenging, but a steady plan can protect comfort and vision.
- Stay on schedule: PRP and anti-VEGF often need timely, multiple visits.
- Manage health conditions: Keep diabetes and blood pressure controlled; quit smoking.
- Know warning signs: New pain, redness, halos, or sudden vision drop warrant same-day contact.
- Protect the eye: Use shields as directed after surgery; avoid rubbing.
There’s no guaranteed way to prevent NVG, but fast treatment of diabetic eye disease and vein occlusions—plus good systemic control—reduces risk of abnormal vessel growth and pressure spikes. See patient guidance from the Glaucoma Research Foundation. 4
Latest Research & Developments
Coordinated care improves safety: Reviews emphasize best outcomes when retina and glaucoma specialists coordinate—using anti-VEGF to quiet vessels, completing PRP, and timing pressure-lowering surgery appropriately. 6
Which tube implant? Comparative studies of valved (e.g., Ahmed) vs. non-valved (e.g., Baerveldt) implants show both can work; selection depends on eye status and surgeon preference. Evidence summaries continue to refine choices. 10
Recently Published in Peer-Reviewed Journals
Ophthalmology. Retina
September 1, 2025
Association of Anti-VEGF Therapy with Reported Ocular Adverse Events: A Global Pharmacovigilance Analysis.
Lakhani M, Kwan ATH, Kundapur D, et al.
The British journal of ophthalmology
August 31, 2025
Reactivation of retinopathy of prematurity after anti-VEGF treatment: a review.
Kumawat D, Kandasamy S, Chandra P
Ophthalmology. Glaucoma
August 28, 2025
Causes and treatments of malignant glaucoma in the United States: Analysis of IRIS® Registry (Intelligent Research in Sight).
Fujita A, Kearney WC, Friedman DS, et al.
Next Steps
If you have signs of NVG—or were just diagnosed—the best specialist to see is a glaucoma specialist (ophthalmologist). Many people also need a retina specialist to treat the underlying retinal disease.
How to schedule:
- Ask for a “neovascular glaucoma evaluation.”
- Bring glasses/contact info, medication list, and prior eye records/photos.
- If your insurance needs a referral, call your primary care office first.
Timing tips: NVG can change quickly—request the cancellation list and alert the clinic if you have pain, redness, or sudden vision loss for sooner triage.
What to expect: You may need same-day retina treatment (injection or laser) and pressure-lowering steps. Bring a driver if possible.
Fast guidance: You can connect with the right specialist on Kerbside for a medical education consult to prepare for your visit (educational only; no physician–patient relationship).


