Retinal Vein Occlusion
Last updated July 31, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.
Overview
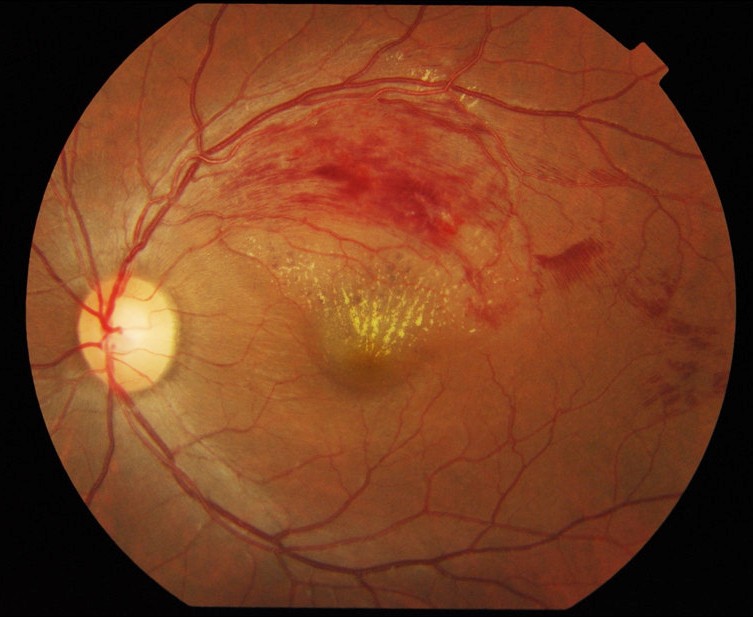
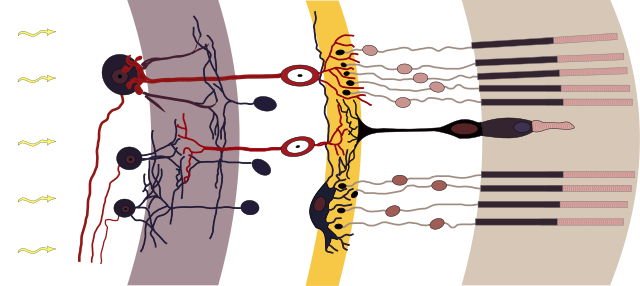
Retinal vein occlusion (RVO) is the second‑most‑common sight‑threatening vascular problem of the retina, surpassed only by diabetic retinopathy. It occurs when a blood clot or external compression blocks a retinal vein, preventing oxygen‑poor blood from leaving the eye. The backup of blood and fluid may cause retinal hemorrhages, macular edema and, in severe cases, blinding complications such as neovascular glaucoma. There are two main types: central retinal vein occlusion (CRVO), where the main vein is blocked, and branch retinal vein occlusion (BRVO), where an outflow branch is affected.1 Worldwide, RVO affects an estimated 16 million people and is most common after age 50.2
Symptoms
- Painless vision loss or blurring in one eye, which may occur suddenly or evolve over hours.3
- Floaters caused by tiny blood cells leaking into the vitreous.
- Distorted (wavy) vision from macular edema, especially when straight lines appear bent.
- Sectoral visual field defect—more typical of BRVO—matching the part of retina drained by the occluded vein.4
- Eye pain or redness is uncommon, but can signal neovascular glaucoma in longstanding ischemic CRVO.
Because early RVO can be subtle, any unexplained change in vision warrants a same‑week dilated eye examination.
Causes and Risk Factors
RVO reflects Virchow’s triad: vessel wall damage, sluggish blood flow, and hyper‑coagulability. Key risk factors include:
- Age > 50 years, with prevalence peaking in the 60s and 70s.5
- Systemic hypertension, diabetes, and hyperlipidemia—all contribute to atherosclerotic arterial stiffening that compresses adjacent veins.
- Glaucoma or ocular hypertension, which raise venous pressure inside the eye.6
- Smoking and elevated body‑mass index.
- Thrombophilia or oral contraceptive use—especially in patients <50 years or in bilateral disease.
About 10 % of patients will later develop an occlusion in the fellow eye, underscoring the need to address systemic risk factors.
Retinal Vein Occlusion Risk Estimator
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
An ophthalmologist—preferably a retina specialist—performs a comprehensive evaluation that typically includes:
- Dilated fundus exam revealing "blood and thunder" hemorrhages in CRVO or sectoral hemorrhage in BRVO.7
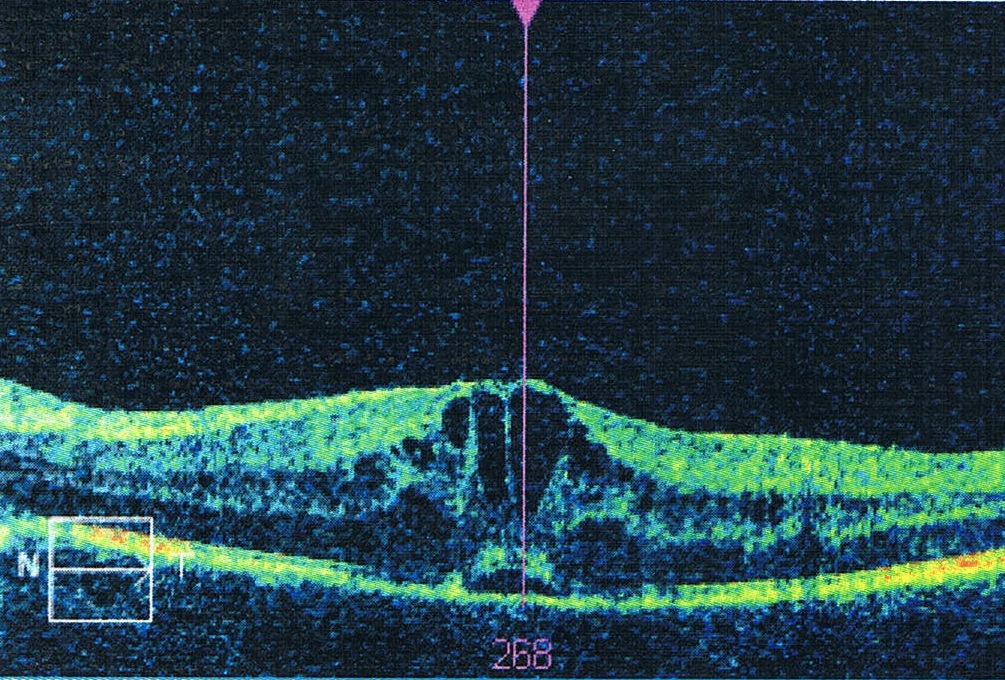
- Optical Coherence Tomography (OCT) to quantify macular edema and guide treatment.
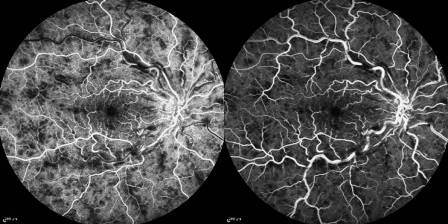
- Fluorescein angiography to map areas of non‑perfusion and detect neovascularization.8
- Blood pressure, fasting glucose/lipids, and thrombophilia work‑up (in younger or bilateral cases) coordinated with primary care.
Treatment and Management
While the blocked vein itself cannot be reopened, modern therapies can preserve and often improve vision:
- Intravitreal anti‑VEGF injections (bevacizumab, ranibizumab, aflibercept) are first‑line for macular edema and neovascularization, given monthly at first, then tapered individually.9
- Intravitreal corticosteroid implants (Ozurdex®) are alternatives for eyes unresponsive to anti‑VEGF but carry cataract and pressure‑rise risks.10
- Pan‑retinal laser photocoagulation is reserved for ischemic eyes with anterior‐segment or retinal neovascularization.
- Manage systemic disease: strict control of blood pressure, blood sugar, and cholesterol reduces recurrence risk.
Most eyes require a series of injections over months to years, but earlier initiation is linked to better long‑term vision.
Living with Retinal Vein Occlusion and Prevention
Life after an RVO can be active and fulfilling when patients understand the condition:
- Monitor vision at home with an Amsler grid; report new distortion, floaters or sudden dimming immediately.11
- Follow injection schedules faithfully; missing visits can allow edema or neovascularization to rebound.12
- Adopt heart‑healthy habits: quit smoking, exercise regularly, and keep blood pressure <130/80 mm Hg.
- Protect the fellow eye with yearly (or physician‑directed) dilated exams.
Low‑vision aids and orientation‑and‑mobility training can help people with permanent visual field loss maintain independence.
Latest Research & Developments
- SCORE2 five‑year data show that eyes receiving anti‑VEGF for CRVO retain about three lines of visual gain at 60 months, although many still need ongoing therapy.13
- Gene and RNA‑based anti‑VEGF delivery trials are under way, aiming for "one‑and‑done" sustained suppression of macular edema (e.g., NCT04507242).
- Artificial‑intelligence algorithms applied to OCT/angiography are being trained to predict which non‑ischemic CRVO eyes will convert to the ischemic form.
- Studies are exploring systemic anticoagulation in select young adults with hyper‑coagulable states, although consensus guidelines are pending.
Recently Published in Peer-Reviewed Journals
BMC ophthalmology
July 9, 2025
Central Retinal Vein Occlusion (CRVO) complicating post-cataract surgery: a case report and multifactorial analysis.
Xiaodong L, Xin L, Xuewei Q, et al.
BMC ophthalmology
July 1, 2025
Effect of combined therapy based on transscleral peripheral retinal cryotherapy in the treatment of open-angle neovascular glaucoma: a retrospective study.
Gao L, Huang J, Cao L, et al.
Retina (Philadelphia, Pa.)
June 24, 2025
The feasibility of Ultra-widefield SS-OCTA to guide laser photocoagulation in retinal vascular diseases.
Lan T, Huang C, Tao M, et al.
Next Steps - See a Retina Specialist
If you notice sudden vision loss, a shower of floaters, or distortion, ask for an urgent appointment with a board‑certified retina specialist—these physicians have the imaging tools and in‑office treatments needed to stabilize vision.15
Tell the scheduler you have "possible retinal vein occlusion with vision change" to secure a same‑day or next‑day slot. When referral pathways are slow, visiting an emergency department with eye‑care coverage is appropriate.16 You can also connect directly to the right specialist on Kerbside for rapid triage and second opinions.
Trusted Providers for Retinal Vein Occlusion

Dr. Emily Eton
Specialty
Retina/Vitreous
Education
Harvard Medical School

Dr. Grayson Armstrong
Specialty
Retina/Vitreous
Education
Ophthalmology

Dr. Jose Davila
Specialty
Retina/Vitreous
Education
Retina/Vitreous Surgery

Dr. Nicholas Carducci
Specialty
Retina/Vitreous
Education
University of Pennsylvania Perelman School of Medicine