Cataracts
also known as Cataract
Last updated July 26, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.


Overview
A cataract is a cloudy area that forms inside the eye’s normally clear lens, scattering light and making vision look foggy, hazy, or dim. Cataracts most often happen with age as lens proteins break down, but they can appear sooner after eye injury, surgery, or certain medical problems. More than half of all Americans will develop a cataract or have cataract surgery by age 80 2. Around the world, cataracts remain the leading cause of reversible blindness, yet modern outpatient surgery can restore sharp sight in minutes. Knowing the early signs and risk factors can help you and your ophthalmologist decide when treatment is right for you 1.
Symptoms
Cataracts usually grow slowly. Early on you might not notice anything, but as the lens gets cloudier you can experience:
- Blurry, dim, or cloudy vision that won’t clear even with a new glasses prescription.
- Glare, halos, or star-bursts around lights, especially at night.
- Difficulty with night driving or reading small print.
- Faded or yellowed colors.
- Frequent prescription changes for glasses or contacts.
- Double vision in one eye (monocular diplopia).
If you ever notice a sudden shower of floaters, flashes of light, or a curtain over part of your vision, call an eye-care professional right away—those symptoms are usually not cataracts but can mean a retinal emergency 3 4.
Causes and Risk Factors
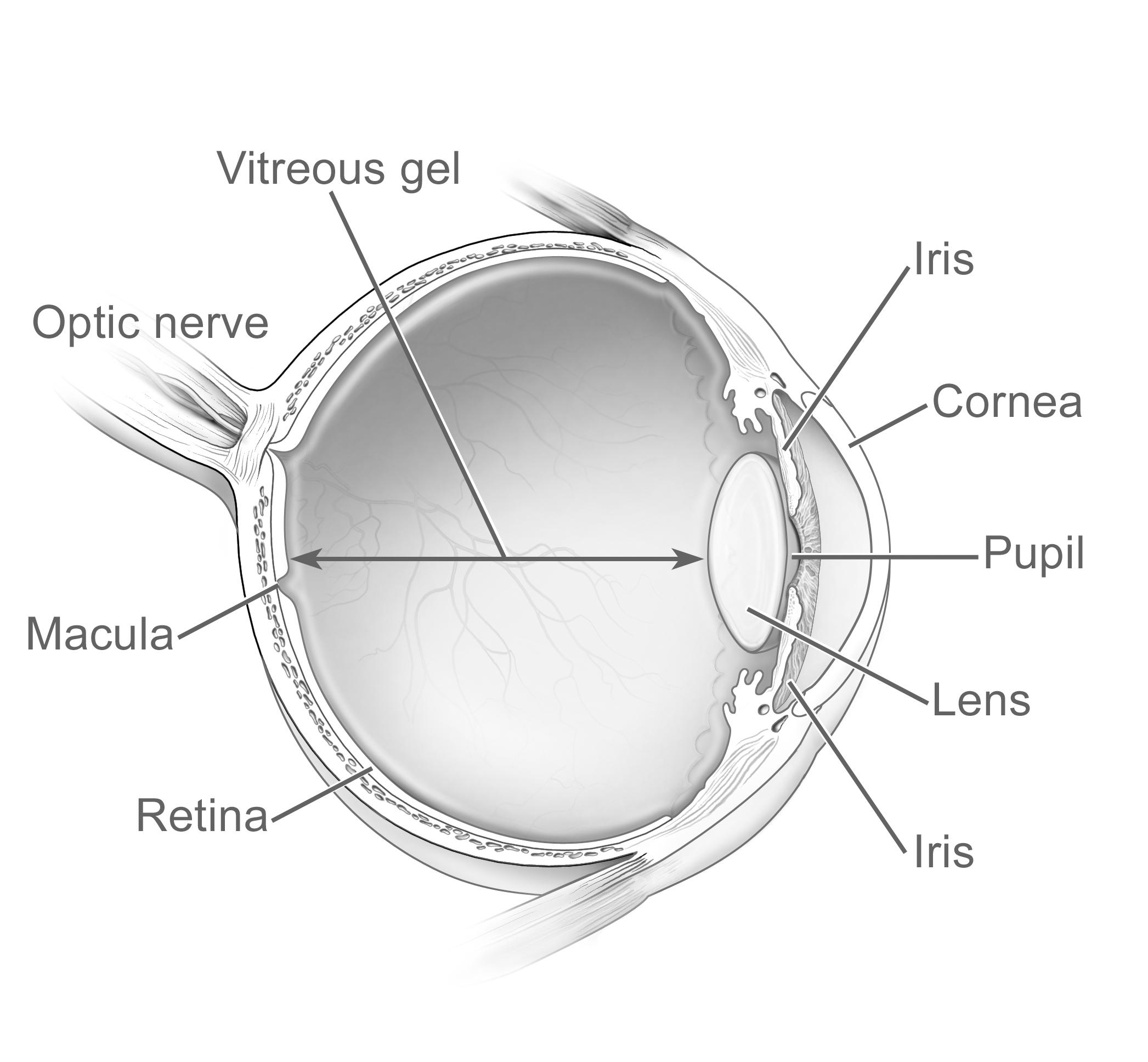
The lens sits just behind the colored iris and is made mostly of water and transparent proteins. With time (or added stress), those proteins clump together and turn the lens milky. Factors that speed the process include:
- Aging – the No. 1 cause.
- Diabetes – high blood sugar accelerates lens clouding.
- Excessive UV exposure – lifelong sun without UV-blocking eyewear.
- Smoking – doubles the risk in some studies.
- Long-term steroid use – pills, inhalers, or eye drops.
- Eye trauma or surgery.
- Family history – genetics can make the lens more vulnerable.
- Other factors – obesity, hypertension, heavy alcohol use, or radiation treatment.
Managing blood sugar, quitting tobacco, and wearing wrap-around sunglasses with 100 % UVA/UVB protection can all help delay progression 5 6.
Cataract Risk Estimator
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
An ophthalmologist can confirm a cataract during a painless, dilated eye exam:
- Visual-acuity test (refraction) checks how clearly you read letters of different sizes.
- Slit-lamp exam magnifies the front of the eye so the doctor can see tiny lens opacities.
- Dilated retinal exam lets the doctor judge how much your cataract blocks the view of the retina and rule out other problems.
- Additional tests such as optical coherence tomography (OCT) or specular microscopy may be used to plan surgery.
Cataracts are staged as mild, moderate, or severe based on how much they limit daily activities. Surgery is considered when reading, driving, or hobbies become difficult, not on an arbitrary vision number 7 8.
Treatment and Management
Early cataracts can be managed with brighter lighting, high-contrast reading material, anti-glare coatings, or magnifiers. Once the cloudiness interferes with daily life, the only effective treatment is cataract surgery.
The procedure is usually done under local anesthesia in 15–20 minutes. The surgeon removes the cloudy lens (typically with ultrasound or a femtosecond laser) and replaces it with a clear intra-ocular lens (IOL). Modern IOL choices include:
- Monofocal – sharpest quality at one distance, glasses needed for the rest.
- Toric – corrects astigmatism.
- Extended-depth-of-focus or multifocal – designed to reduce dependence on reading glasses.
Cataract surgery is one of the safest operations anywhere, with vision improving in more than 98 % of otherwise healthy eyes 9. Post-op drops or dropless injections prevent infection and inflammation, and most people return to normal activities within a week 10.
Living with Cataracts and Prevention
Between diagnosis and surgery, simple lifestyle tweaks can keep vision as clear as possible:
- Use brighter task lighting and position light behind your shoulder when reading.
- Choose high-contrast, large-print books or e-reader settings.
- Wear polarized sunglasses outdoors to cut glare.
- Limit night driving if halos become distracting.
You can’t fully prevent cataracts, but you can slow them down:
- Schedule a comprehensive dilated eye exam every 1–2 years after age 60.
- Stop smoking—tobacco doubles risk.
- Eat a diet rich in leafy greens, colorful fruits, and omega-3 fats.
- Keep blood sugar and blood pressure in a healthy range.
- Limit alcohol to moderate levels.
These steps also support overall eye health and may delay other age-related eye diseases 11 12.
Latest Research & Developments
Researchers are exploring ways to treat cataracts before surgery is necessary. In 2024, NIH scientists identified a protein called RNF114 that reversed lens clouding in animal models, a discovery that could pave the way for drop-based therapy 13. Surgical technology keeps evolving too—femtosecond-laser assisted cataract surgery (FLACS) can create ultra-precise incisions and reduce ultrasound energy, improving astigmatism correction and early visual recovery 14.
Next-generation extended-depth-of-focus and AI-designed multifocal IOLs are also in late-stage trials, promising sharper vision at multiple distances with fewer halos. Keep an eye on our curated research feed for updates.
Recently Published in Peer-Reviewed Journals
BMC ophthalmology
July 1, 2025
Ocular findings in children, adolescents and young adults with type 1 diabetes mellitus in ghana: a cross-sectional study.
Asafo-Agyei SB, Ameyaw E, Aikins A
Investigative ophthalmology & visual science
July 1, 2025
Mettl3 Regulates Lens Development by Promoting the Differentiation Processes of Secondary Fiber Cells.
Hu L, Ma J, Guo J, et al.
American journal of ophthalmology
June 20, 2025
The Associations Between Glaucoma and Circadian Rhythm Sleep Disorders in California Medicare Beneficiaries.
Ramirez M, Kitayama K, Puran A, et al.
Next Steps
If cloudy vision is affecting your life, don’t wait.
See a cataract surgeon (anterior-segment ophthalmologist) for a full exam. They will confirm the diagnosis, measure your eyes for the best IOL, and discuss timing.
How to schedule:
- Referral path: Ask your optometrist or primary-care doctor for a surgical referral.
- DIY path: Use the American Academy of Ophthalmology’s “Find an Ophthalmologist” directory and filter for “Cataract & Refractive Surgery.” Mention night-driving glare when you call so staff know it’s time-sensitive 15.
- Virtual path: Many cataract surgeons now offer tele-consults. Upload your latest eye-exam report so the surgeon can focus on goals and lens options.
The National Eye Institute also lists tips for finding local eye-care providers and what to expect at an exam 16. Even if surgery isn’t needed yet, an early visit can reassure you and help you plan ahead.
Trusted Providers for Cataracts

Dr. Connie Wu
Specialty
Glaucoma
Education
The Warren Alpert Medical School of Brown University

Dr. Dane Slentz
Specialty
Oculoplastics
Education
Oculoplastics

Dr. Emily Eton
Specialty
Retina/Vitreous
Education
Harvard Medical School

Dr. Emily Schehlein
Specialty
Glaucoma
Education
Glaucoma

Dr. Grayson Armstrong
Specialty
Retina/Vitreous
Education
Ophthalmology

Dr. Jose Davila
Specialty
Retina/Vitreous
Education
Retina/Vitreous Surgery

Dr. Karen Chen
Specialty
Glaucoma
Education
Glaucoma

Dr. Levi Kanu
Specialty
Cornea and External Disease
Education
Cornea and External Disease

Dr. Nicholas Carducci
Specialty
Retina/Vitreous
Education
University of Pennsylvania Perelman School of Medicine