Flashes of Light
also known as Photopsia
Last updated August 20, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.
Overview
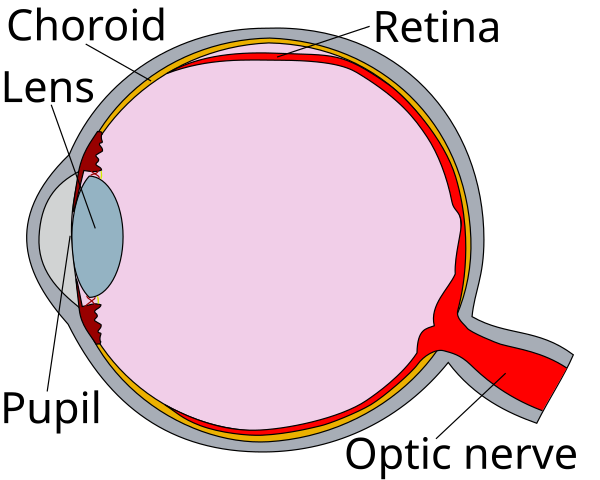
Flashes of light (also called photopsia) are brief, bright streaks, sparks, or arcs that appear even when no light is actually there. They happen when the light-sensing layer in the back of your eye (the retina) is tugged or stimulated.
Flashes are common as we age and the gel inside the eye (vitreous) changes, but sudden or repeated flashes—especially with new floaters or a dark curtain in vision—need same-day eye care because they can be a warning sign of a retinal tear or detachment. 1
A retinal detachment is an emergency that can cause permanent vision loss if not treated quickly. 2
Symptoms
People describe flashes in different ways. Common descriptions include:
- Quick arcs or "lightning" in the side vision, often easier to notice in dim rooms or at night.
- Sparkles or camera-flash bursts that last seconds.
- Flashes with new floaters (specks or cobwebs drifting in vision), which may happen when the vitreous pulls away from the retina.
- A dark shadow or curtain coming over part of the view—this can mean a detachment.
- Zigzag, shimmering patterns that move across vision for 5–60 minutes (usually a migraine aura from the brain, not the eye).
If floaters suddenly increase—especially with flashes or vision loss—seek immediate care. 3 7
Causes and Risk Factors
Most flashes come from changes in the vitreous gel:
- Posterior vitreous detachment (PVD): The gel naturally shrinks with age and can separate from the retina, triggering brief flashes. PVD is common after age 50 and usually not sight-threatening, but sometimes leads to a tear.
- Retinal tear or detachment: A strong tug can rip the retina. Fluid may then slip behind it and cause detachment—an emergency.
- Migraine aura: Zigzag or shimmering lights, often in both eyes, caused by brain activity changes.
Risk factors for retinal tear when PVD occurs include:
- Very recent symptom onset (<24 hours).
- Blood in the eye (vitreous hemorrhage).
- Vision drop at presentation. 5
- High myopia, lattice degeneration, family/personal history of retinal detachment, recent cataract surgery, or trauma. 6
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
The safest step is a prompt, dilated eye exam by an eye doctor. Expect:
- History and vision testing (onset, frequency, floaters, curtain of vision loss).
- Dilated retinal exam with scleral depression to look for tears.
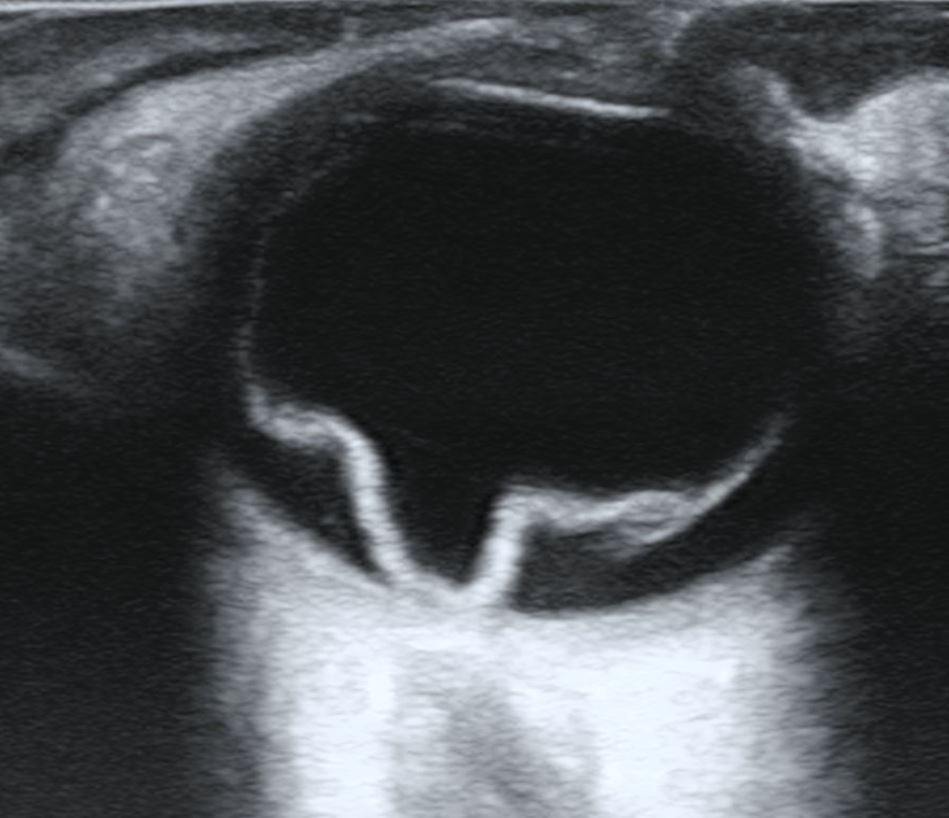
- Imaging when needed: ocular ultrasound (if cloudy view) or OCT to check retina/vitreous.
Red-flag symptoms needing same-day care:
- Sudden shower of new floaters.
- Many flashes.
- Shadow in side vision.
- Gray curtain across vision. 1
Your provider may also ask about migraine-like zigzags and triggers like stress or foods. 4
Treatment and Management
Treatment depends on the cause:
- PVD without a tear: Observation. Flashes fade over weeks; floaters become less noticeable. Follow-up exams and return precautions are important.
- Retinal tear: Treated urgently with laser or freezing to seal the tear and prevent detachment.
- Retinal detachment: Surgery (vitrectomy, pneumatic retinopexy, scleral buckle). 2
- Migraine aura: Lifestyle changes and migraine medicines guided by a clinician; no eye surgery needed.
Warning signs for urgent re-check: sudden increase in floaters, more flashes, or any shadow/curtain in vision. 7
Living with Flashes of Light and Prevention
You can’t fully prevent age-related vitreous changes, but you can protect your sight:
- Act fast: for new flashes, many floaters, curtain of darkness, or vision loss—these can be emergencies. 3
- Schedule follow-ups: after PVD or treatment, so your doctor can re-check the retina.
- Use eye protection: for sports or risky work to reduce trauma-related tears.
- Manage health conditions: like diabetes and blood pressure, and don’t ignore sudden vision changes.
- Know your risks: high myopia, lattice degeneration, or recent eye surgery raise the chance of a tear—have a plan for urgent care. 6
Latest Research & Developments
Large studies continue to refine how we triage flashes and floaters:
- Researchers identified factors tied to higher risk of retinal tear/detachment at the time of acute PVD. 8
- Some patients without tears at first developed delayed tears later, supporting follow-up beyond the classic 6-week visit. 9
- New tools like ultra-widefield imaging and AI triage models are being explored to speed evaluations.
Recently Published in Peer-Reviewed Journals
Investigative ophthalmology & visual science
June 2, 2025
Impact of Second-Generation PDE 5 Inhibitor, Avanafil, on Retinal Function: Studies From Ex Vivo ERG.
Saeid S, Vinberg F, Koskelainen A
Ophthalmology. Retina
May 26, 2025
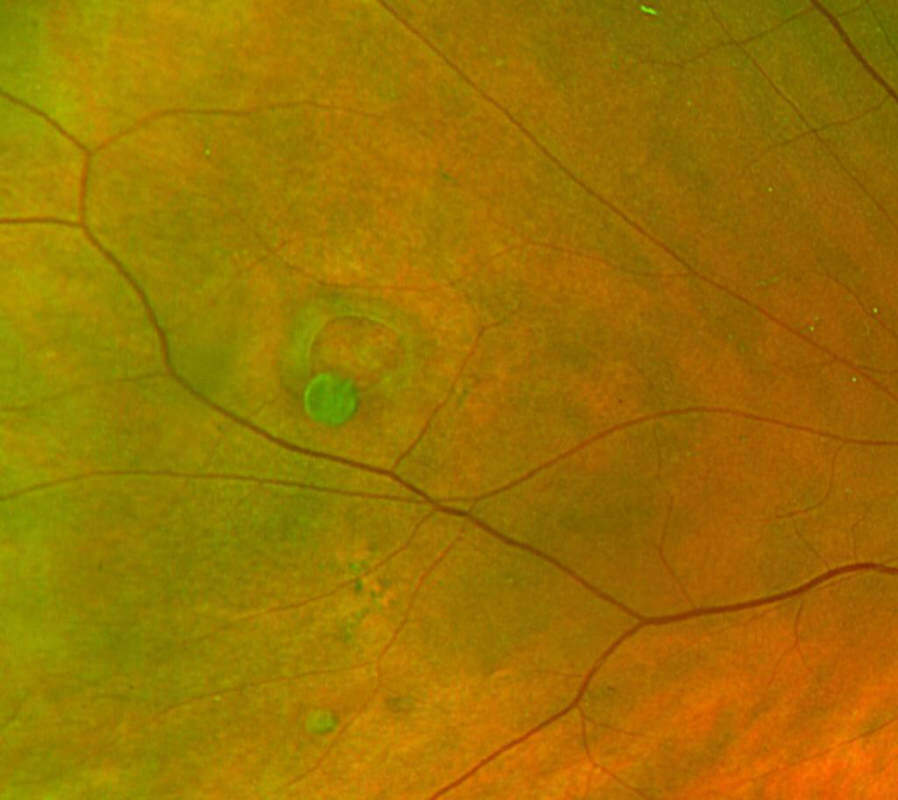
Clinical and Multimodal Imaging of Acute Outer Retinopathy: Expanding the Spectrum of Acute Annular Outer Retinopathy.
Ramtohul P, Cicinelli MV, Chen FK, et al.
Ophthalmology. Retina
October 27, 2023
Acute Macular Neuroretinopathy after COVID-19 Infection: Clinical Characteristics and Associated Factors.
Fang L, Tian T, Zhuang S, et al.
Next Steps
Who to see: If you have new or repeated flashes, especially with floaters or any shadow in your vision, arrange a same-day exam with a retina specialist (ophthalmologist). If not possible, go to urgent eye clinic or the emergency department. 1
How to schedule:
- Tell the scheduler you have "new flashes and floaters" or "a curtain in vision"—offices often keep urgent slots.
- If the first clinic is booked, ask to be placed on a cancellation list or try nearby practices.
- After treatment (laser/surgery), you’ll get follow-up dates and clear return precautions.
Kerbside option: You can connect with the right specialist on Kerbside for a medical education consult to understand your symptoms and care pathway. This is not a patient–physician relationship, but it can help you prepare informed questions and next steps.
Trusted Providers for Flashes of Light

Dr. Emily Eton
Specialty
Retina/Vitreous
Education
Harvard Medical School

Dr. Grayson Armstrong
Specialty
Retina/Vitreous
Education
Ophthalmology

Dr. Jose Davila
Specialty
Retina/Vitreous
Education
Retina/Vitreous Surgery

Dr. Nicholas Carducci
Specialty
Retina/Vitreous
Education
University of Pennsylvania Perelman School of Medicine