Retinal Detachment
Last updated July 24, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.

Overview
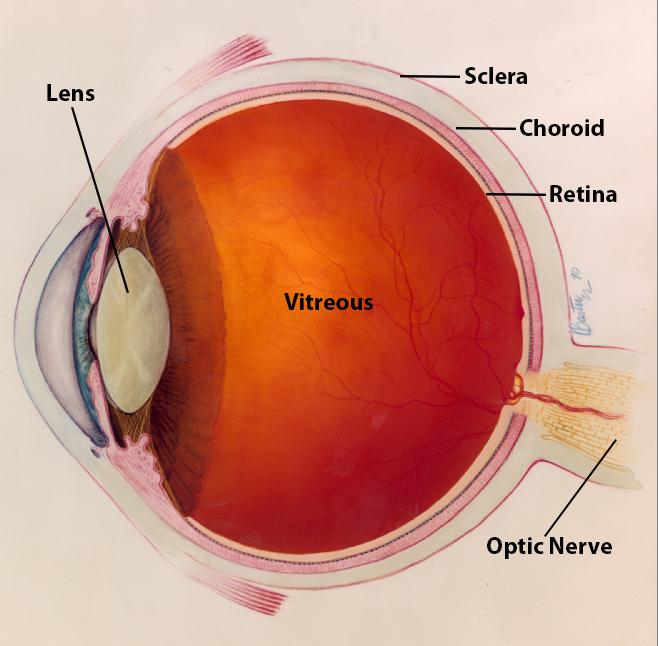
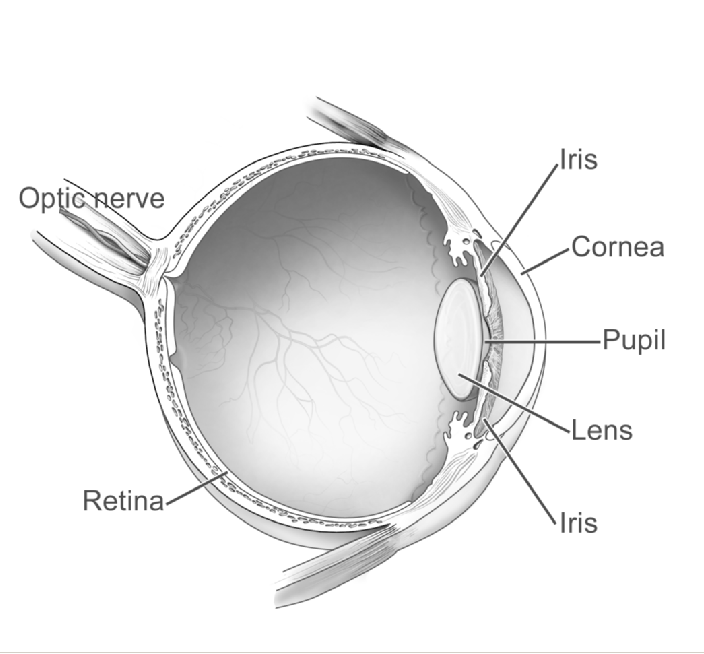
Retinal detachment (RD) occurs when the light-sensing retina pulls away from the supportive layer that supplies oxygen and nutrients. Without urgent care, the disconnected tissue cannot work, and permanent blindness can follow within hours to days. RD is a true ocular emergency; it affects about one person in every 10,000 each year and can strike at any age, although risk rises with mid- to later life. Because the early retina has no pain fibers, warning signs may be subtle or absent, making routine dilated eye exams and rapid attention to new visual symptoms critical for sight preservation 1 2.
Symptoms
RD is usually painless. Typical red-flag symptoms include:
- Sudden bursts of flashes of light (photopsias)
- A shower of new floaters—dark specks, cobwebs, or threads
- A shadow or curtain creeping over side or central vision
- Blurred or distorted sight that worsens over minutes or hours
These signs can appear alone or together and may wax or wane. Anyone who experiences them should seek same-day ophthalmic evaluation; delaying even 24 hours can markedly reduce final vision if the macula detaches 2 3.
Causes and Risk Factors
Most RDs are rhegmatogenous, triggered by a retinal tear that lets fluid slip under the retina. Less commonly, scar tissue (tractional RD) or fluid leaks (exudative RD) separate the layers. Key risk factors include:
- Age > 50 years or long-standing high myopia (especially > –6 diopters)
- Previous eye surgery—cataract removal is the most frequent surgical antecedent
- Significant blunt or penetrating eye trauma
- Family history of RD or inherited lattice degeneration
- Systemic or ocular diseases like diabetic retinopathy or posterior vitreous detachment
Population studies show that people with high myopia are 10-fold more likely to experience RD, and cataract surgery roughly triples lifetime risk 4 5.
Retinal Detachment Risk Estimator
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
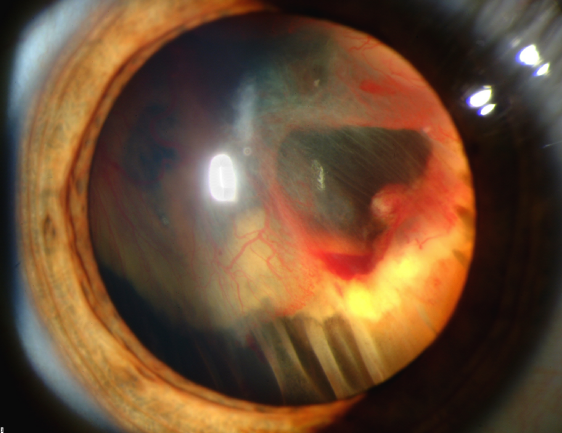
Diagnosis
An ophthalmologist performs a comprehensive dilated fundus examination using binocular indirect ophthalmoscopy and scleral depression to look for retinal breaks. When the view is hazy, B-scan ultrasound quickly confirms a detached, mobile membrane. Optical coherence tomography (OCT) helps identify subtle macular involvement, while ultrawide-field fundus photography documents break locations for surgery planning. Modern offices can complete these tests within minutes, allowing same-day treatment scheduling 1 3.
Treatment and Management
The choice of repair depends on tear size, location, and surgeon expertise:
- Pneumatic retinopexy – office injection of a gas bubble combined with laser or cryotherapy to seal a single superior break.
- Scleral buckle – a silicone band indents the eye wall, relieving traction and supporting multiple breaks.
- Pars plana vitrectomy – micro-incision removal of the vitreous gel plus laser, gas, or silicone oil; preferred for complex or posterior tears.
Success rates exceed 90 % with timely surgery. The American Academy of Ophthalmology advises repair within 24 hours if the macula is still attached, or within a few days if already off 6. Adjunctive laser or cryopexy prevents redetachment 7, while vitrectomy innovations—smaller gauges and wide-angle viewing—shorten recovery 8.
Living with Retinal Detachment and Prevention
After successful repair, most people resume normal activities within weeks, but follow-up visits are critical to detect new tears or elevated eye pressure. To reduce risk of a first—or second—detachment:
- Wear protective eyewear during sports, yard work, and high-speed activities
- Manage high myopia with regular retinal checks
- Report sudden floaters or flashes immediately
- Schedule a comprehensive dilated eye exam every 1–2 years, or sooner if advised
Patients who have had RD in one eye face up to a 10 % chance in the fellow eye; vigilant monitoring and healthy lifestyle habits (no smoking, good glycemic control) help safeguard the remaining retina 5 11.
Latest Research & Developments
Research is refining techniques and reducing the need for repeat surgery:
- The PIVOT randomized trial showed that pneumatic retinopexy can yield comparable anatomic outcomes to vitrectomy for selected detachments, with faster visual recovery 9.
- Real-world data suggest newer small-gauge vitrectomy systems lower postoperative inflammation and speed rehabilitation 10.
- Investigators are testing hydrogel and gene-based adhesives that could one day close retinal breaks without gas or scleral buckles.
These advances aim to simplify care, minimize face-down positioning, and improve long-term vision.
Recently Published in Peer-Reviewed Journals
The British journal of ophthalmology
July 22, 2025
Analysis of 24 pro-inflammatory cytokines in aqueous and serum of 94 patients without diabetes.
Kim SJ, Gangaputra S, Sheng J, et al.
BMC ophthalmology
July 22, 2025
Artificial intelligence in predicting macular hole surgery outcomes: a focus on optical coherence tomography parameters.
Ozturk Y, Ağın A, Yelmi B, et al.
Ophthalmology. Retina
July 21, 2025
Visual Outcomes in Cases of Endogenous Endophthalmitis (VOICE): a multicenter study.
Weng PJ, Woodward R, Duy W, et al.
Next Steps
If you experience flashes, new floaters, or a curtain-like shadow, treat it as a 911 for your eyes. Go to an emergency department or contact an on-call ophthalmologist the same day. People at high risk should keep a list of retina specialists and ask whether they offer 24-hour coverage. The American Academy of Ophthalmology’s online directory lets you filter for Retina/Vitreous surgeons in your zip code 3. Regular dilated exams—even after successful surgery—remain your best defense against permanent vision loss 1.
Trusted Providers for Retinal Detachment

Dr. Emily Eton
Specialty
Retina/Vitreous
Education
Harvard Medical School

Dr. Grayson Armstrong
Specialty
Retina/Vitreous
Education
Ophthalmology

Dr. Jose Davila
Specialty
Retina/Vitreous
Education
Retina/Vitreous Surgery

Dr. Nicholas Carducci
Specialty
Retina/Vitreous
Education
University of Pennsylvania Perelman School of Medicine