Retinal Tear
Last updated August 21, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.

Overview
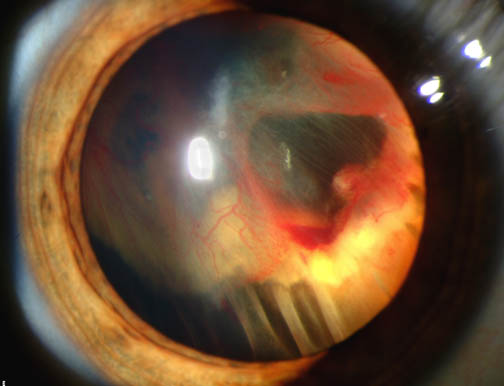
A retinal tear is a small rip or break in the thin, light-sensing tissue at the back of your eye. It often happens when the gel inside the eye (the vitreous) pulls on the retina as we age.
A tear is an emergency because fluid can slip through the opening and lift the retina off the back of the eye, causing a retinal detachment and permanent vision loss if not treated quickly. 1 2
The good news: most tears can be sealed with in-office treatments to protect your sight when caught early.
Symptoms
Retinal tears usually do not hurt. Warning signs often appear suddenly and can include:
- Flashes of light (like camera flashes) in one eye.
- New floaters (specks, cobwebs, or a ring) that appear all at once or seem to multiply.
- A shadow or gray curtain at the edge of your vision.
- Blurred or reduced side vision.
If you notice these symptoms, especially after a new shower of floaters, call an eye doctor the same day or go to the emergency department. Fast care helps prevent a retinal detachment. 3 5
Causes and Risk Factors
Most tears happen during a normal age-related change called posterior vitreous detachment (PVD). As the vitreous gel shrinks, it can tug on the retina hard enough to cause a break.
Other risks include:
- Age (more common after 50).
- Nearsightedness (myopia), especially high myopia.
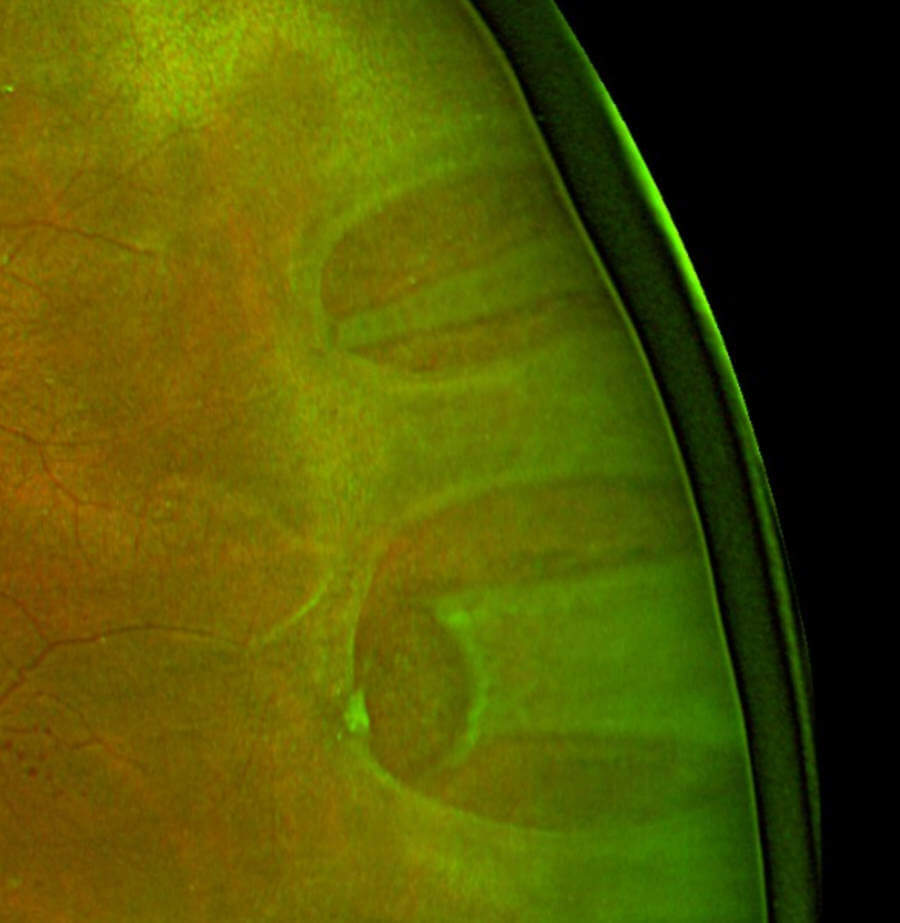
- Lattice degeneration (thin, weak areas in the far retina).
- Eye trauma or recent eye surgery (like cataract surgery).
- Family or personal history of tears or detachment.
These factors raise the chance of a tear and of a detachment if a tear is left untreated. 4 2
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
Eye doctors diagnose a retinal tear with a dilated eye exam. They use bright light and special lenses to see the far edges of the retina. Gentle pressure on the eye (scleral depression) may be used to view the far periphery.
If the view is cloudy from bleeding, an ultrasound (B-scan) can help. If central vision is affected, OCT imaging may be done to check the macula.
Because the risk of detachment is highest early on, a same-day exam is recommended when symptoms start. 3 5
Treatment and Management
Treatment aims to seal the tear so fluid cannot pass through it. Common options include:
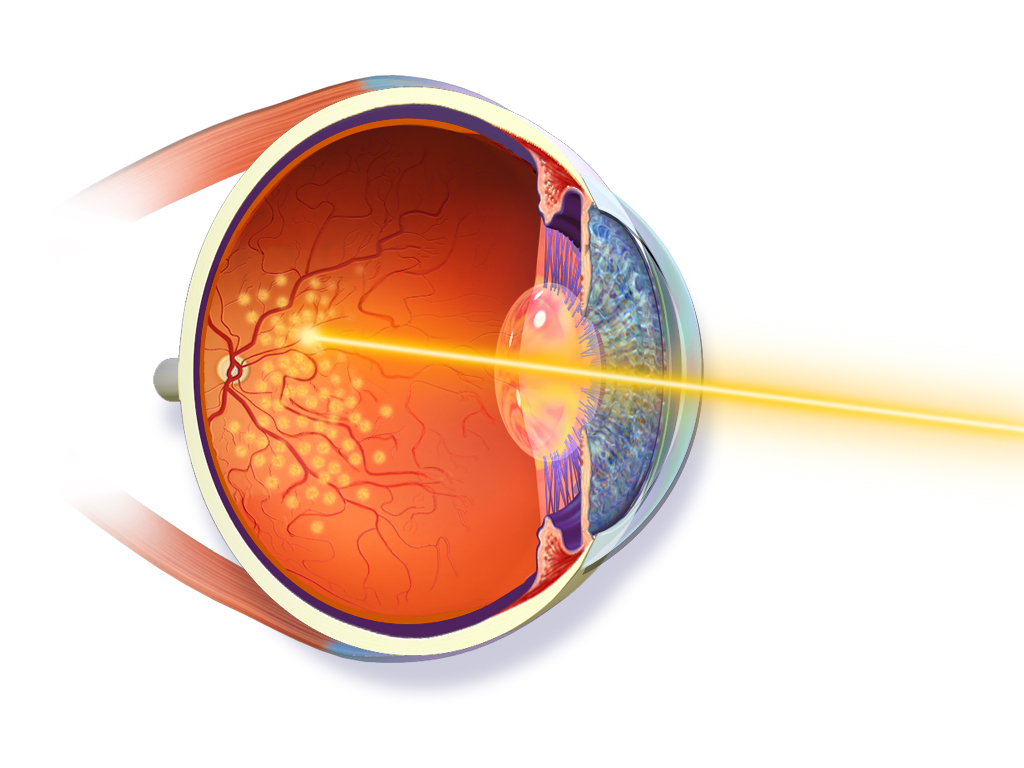
- Laser retinopexy (photocoagulation): a laser makes a ring of tiny burns around the tear, forming a scar that seals it.
- Cryopexy: a very cold probe freezes the area around the tear from outside the eye, also creating a sealing scar.
Both are usually quick, in-office procedures with numbing. Your eye may feel sore for a day or two. You may need to avoid heavy lifting or high-impact activity briefly while the seal forms.
Some small, asymptomatic holes in thin retina may be observed rather than treated if there is no traction or fluid spread; your specialist will explain when observation is safe.
Untreated, certain tears (like symptomatic horseshoe tears) can progress to retinal detachment, which often needs surgery such as:
- Pneumatic retinopexy (gas bubble)
- Vitrectomy (removing the vitreous gel and sealing the tear)
- Scleral buckle (a supportive band placed outside the eye) 6 2
Living with Retinal Tear and Prevention
After treatment, most people return to normal activities quickly. You may still see some floaters; these often fade with time.
Call your eye doctor right away if you notice new flashes, a shower of floaters, or a shadow in your vision—these can signal a new tear or detachment. Keep all follow-up visits; some patients can develop delayed tears weeks to years later, especially with lattice degeneration 7.
Prevention tips:
- Wear eye protection during sports and yard work.
- Manage diabetes and other health conditions.
- Keep up with dilated eye exams if you have high myopia or a prior tear.
You cannot fully prevent age-related changes in the vitreous, but these steps lower risk. 4
Latest Research & Developments
Recent studies help doctors fine-tune who needs closer follow-up after a PVD and tear. Research shows some people develop delayed retinal tears well beyond the traditional 6-week window, especially those with lattice degeneration—so your doctor may individualize follow-up timing based on your risk.
Community-based data also estimate that:
- About 1 in 10 people with symptomatic PVD have a tear at diagnosis.
- A small percentage with an initially normal exam develop a tear over the next months.
This supports repeat checks if symptoms persist or worsen. 8
Updated professional guidelines (Preferred Practice Pattern) outline when to treat versus observe certain small breaks, and emphasize prompt sealing of symptomatic tractional tears to prevent detachment. 5
Recently Published in Peer-Reviewed Journals
American journal of ophthalmology
September 1, 2025
Association of Glucagon-Like Peptide-1 Receptor Agonists With Optic Nerve and Retinal Adverse Events: A Population-Based Observational Study Across 180 Countries.
Lakhani M, Kwan ATH, Mihalache A, et al.
Retina (Philadelphia, Pa.)
June 13, 2025
Risk Factors for Hypotony Following Sutureless Vitrectomy in Patients with Epiretinal Membrane.
Mito T, Okemoto H, Sasaki M, et al.
Retina (Philadelphia, Pa.)
May 12, 2025
FIBRIN GLUE-ASSISTED PRE-TREATED LYOPHILIZED HUMAN AMNIOTIC MEMBRANE TECHNIQUE FOR RETINAL DETACHMENT WITH INFERIOR RETINAL BREAK.
Lin W, Jin Y, Lin X, et al.
Next Steps
If you think you have a retinal tear, seek care today.
Who to see: The best specialist is a retina specialist (vitreoretinal surgeon).
How scheduling usually works:
- Your optometrist, ophthalmologist, or ER can make an urgent referral.
- Retina clinics keep space for emergencies; if the first office is full, ask about sister locations.
- You can also ask to be placed on a cancellation list for the earliest opening.
What to expect: Bring a driver (your pupils will be dilated). Treatment (laser or cryopexy) may happen the same day if a tear is confirmed.
How we can help: You can connect directly to the right specialist on Kerbside for a medical education consult about what to ask and how to prepare. This consult supports your understanding and care coordination; it does not create a patient–physician relationship.
Do not wait: If you notice new flashes, a burst of floaters, or a shadow, fast treatment protects vision. 1 2