Lattice Degeneration
Last updated August 21, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.
Overview
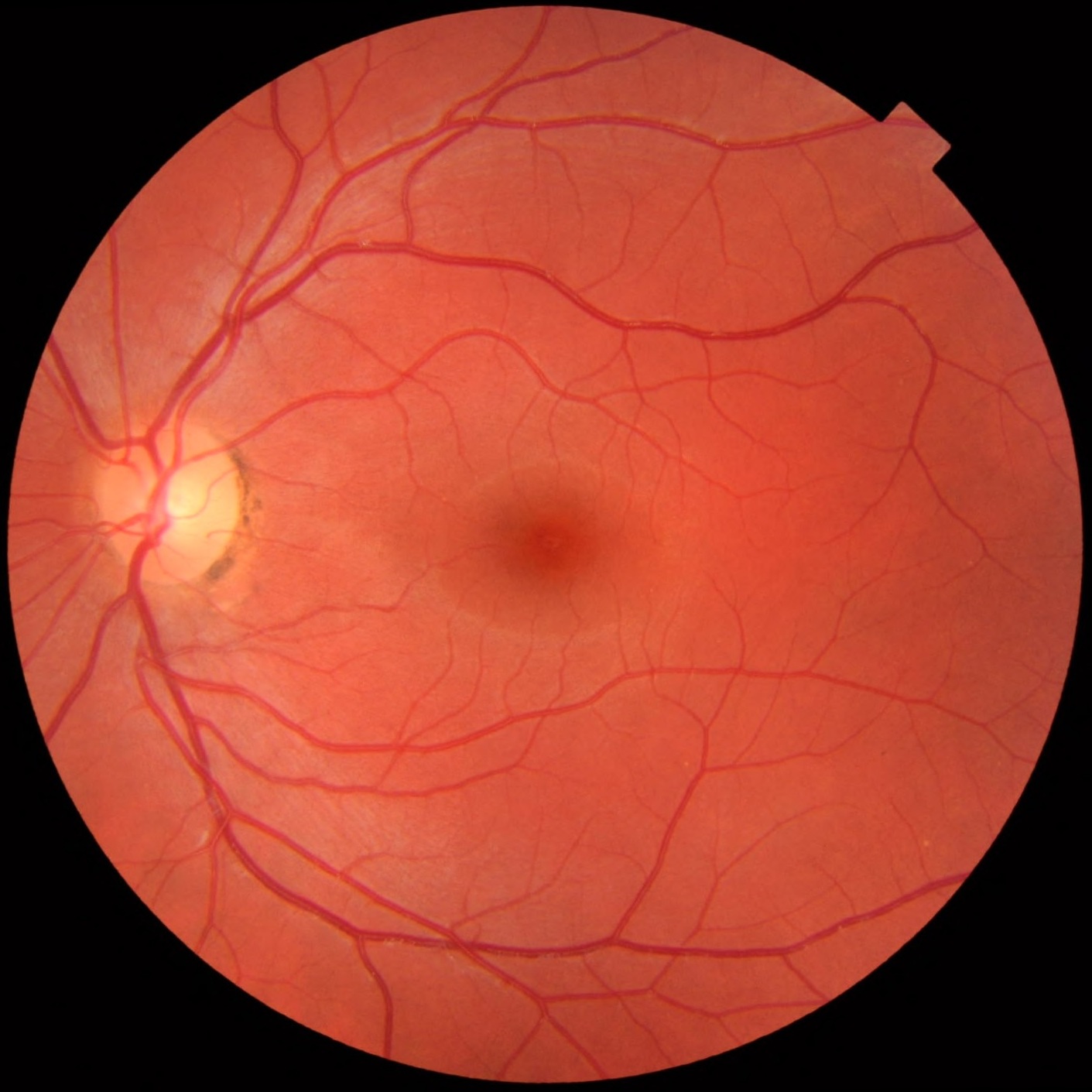
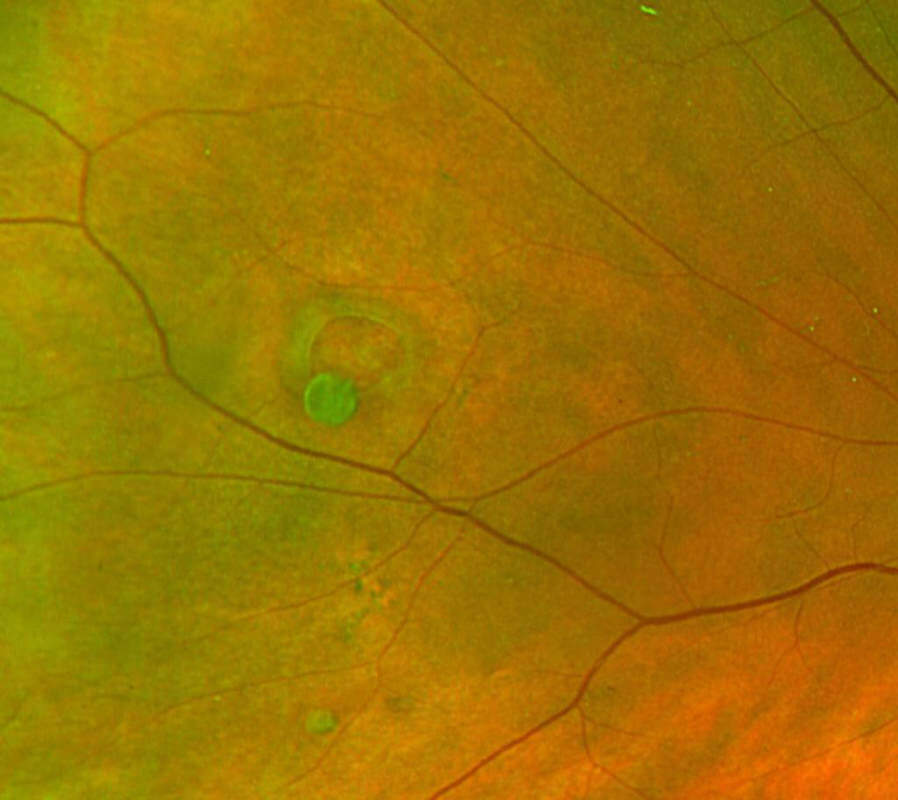
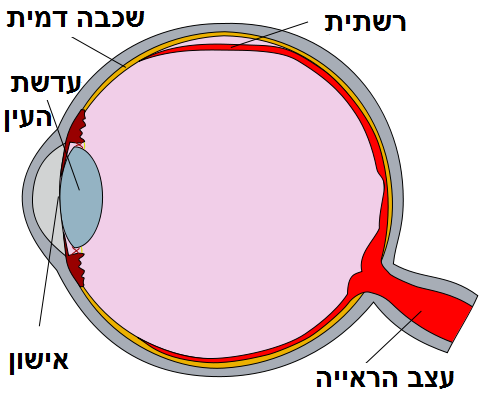
Lattice degeneration is a thinning and weakening of the outer (peripheral) retina. These areas can look like crisscross lines or patches on an eye exam, which is why the condition is called "lattice."
Many people never notice any problems, and the condition is often found during a routine, dilated eye exam. About 1 in 10 people have lattice degeneration, but only a small number ever develop a retinal tear or detachment from it. 2
Even though the overall risk of a serious complication is low, lattice degeneration matters because it slightly raises the chance of a retinal tear or a retinal detachment. Knowing the warning signs and keeping up with regular eye care can help protect your vision. 1
Symptoms
Most people with lattice degeneration have no symptoms. It is usually discovered by an eye care professional during a dilated exam.
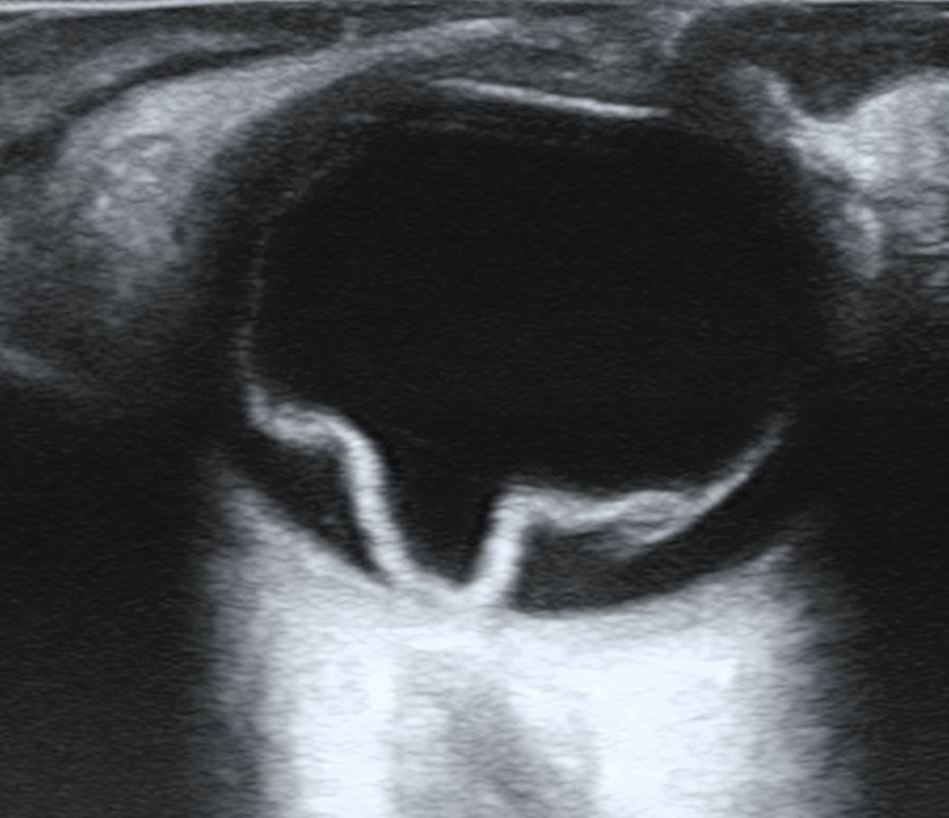
However, if a retinal tear or detachment develops, you may notice warning signs such as:
- Flashes of light (like camera flashes in the side vision)
- New or increasing floaters (small moving spots or strands)
- A shadow, curtain, or gray area moving across your vision
These symptoms are emergencies. If they appear, seek care right away because fast treatment can save vision. 4 5
Causes and Risk Factors
The exact cause of lattice degeneration is not fully understood. It is a change where the retina becomes thin with loose, watery gel (liquefied vitreous) over it and stronger attachments at the edges, making those edges more likely to tear if the gel pulls suddenly. These are well-described changes that eye doctors watch closely. 3
Factors that can raise risk include:
- Nearsightedness (myopia): Lattice occurs more often in people with myopia.
- Family or personal history: A retinal detachment in the other eye or in family members increases risk.
- Posterior vitreous detachment (PVD): Natural separation of the eye’s gel with age can tug on the retina and create tears along lattice edges.
- Eye surgery: Large studies show lattice degeneration is linked with a higher chance of retinal tear or detachment after cataract surgery, especially in younger patients and men. 7
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
Lattice degeneration is diagnosed during a dilated eye exam. Your ophthalmologist or optometrist looks carefully at the far edges of the retina using a bright light and special lenses, sometimes with gentle pressure on the eyelid (scleral depression) to view the periphery.
Photos (wide-field fundus imaging) may be taken to document the areas. Most of the time, no additional testing is needed unless symptoms suggest a tear or detachment. 2 4
Treatment and Management
For most people, lattice degeneration needs no treatment. The main approach is observation with regular dilated exams and clear guidance on warning symptoms.
If an eye has special, higher-risk features—such as:
- A fresh, symptomatic horseshoe tear near lattice
- A detachment in the fellow eye
- Very strong traction
…your eye doctor may recommend sealing a weak area with laser retinopexy or sometimes freezing (cryotherapy) to help prevent a detachment. 3
Importantly, high-quality reviews have not found solid evidence that treating asymptomatic lattice or small retinal holes prevents detachment, so routine “prophylactic” laser for every lattice lesion is not advised. Decisions are individualized based on risk and symptoms. 6
Living with Lattice Degeneration and Prevention
Most people with lattice degeneration live normal lives without vision loss. The best “prevention” is awareness and routine eye care.
- Ask your eye doctor how often to return; many people are checked every 1–2 years, or sooner if risks change.
- Learn the emergency signs (flashes, many new floaters, or a dark curtain) and get immediate care if they occur. 1
- General eye safety also helps: wear sports eye protection during high-impact activities, control overall health risks (like diabetes), and keep your glasses or contact lens prescription current so you can notice sudden changes quickly.
Latest Research & Developments
New analyses from large U.S. databases (IRIS® Registry) suggest that lattice degeneration is a significant factor for retinal tear or detachment following cataract surgery, particularly in younger patients and men. This helps doctors weigh risks and plan follow-up schedules around the time of surgery. 7
Clinical guidance continues to emphasize careful selection for preventive laser, focusing on symptomatic tears or clearly high-risk situations rather than routine treatment of all lattice lesions. Earlier evidence reviews in major ophthalmology journals highlight the limited proof for prophylactic therapy in asymptomatic cases, reinforcing a case-by-case approach. 8
Recently Published in Peer-Reviewed Journals
Retina (Philadelphia, Pa.)
July 8, 2025
Re: CURRAN PROPHYLACTIC TREATMENT OF LATTICE DEGENERATION IN FELLOW EYES AFTER REPAIR OF UNCOMPLICATED PRIMARY RHEGMATOGENOUS RETINAL DETACHMENT. Retina, 44 (1), 63-70. doi: 10.1097/IAE.0000000000003908.
Morris RE, Kuhn F, Baxter CR, et al.
BMC ophthalmology
June 6, 2025
Characteristics of myopic retinopathy and its awareness in adults: a hospital-based comparative study.
Syal AD, Satapathy J, Panigrahi PK
Retina (Philadelphia, Pa.)
June 1, 2025
NONDRAINAGE SCLERAL BUCKLING IN THE MODERN VITRECTOMY ERA.
Barile GR, Gupta R, Engelbert M, et al.
Next Steps
If you were told you have lattice degeneration, the best professional to see is a retina specialist (ophthalmologist). Many patients can continue routine care with their comprehensive ophthalmologist and see a retina specialist if risks or symptoms arise.
How to schedule: Start with your current eye doctor or primary care provider for a referral if your insurance needs one. Ask to be placed on a cancellation list to be seen sooner.
If you notice emergency symptoms (flashes, a lot of new floaters, or a curtain over your vision), go to an urgent eye clinic or emergency department right away. 1
You can also connect with the right specialist on Kerbside for a medical education consult to understand your findings and discuss questions. This is educational support only and does not create a patient–physician relationship.
Trusted Providers for Lattice Degeneration

Dr. Emily Eton
Specialty
Retina/Vitreous
Education
Harvard Medical School

Dr. Grayson Armstrong
Specialty
Retina/Vitreous
Education
Ophthalmology

Dr. Jose Davila
Specialty
Retina/Vitreous
Education
Retina/Vitreous Surgery

Dr. Nicholas Carducci
Specialty
Retina/Vitreous
Education
University of Pennsylvania Perelman School of Medicine