Eye Floaters
also known as Vitreous Floaters, Myodesopsias, Floaters
Last updated July 31, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.


Overview
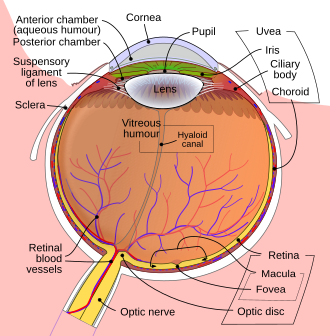
Eye floaters are tiny clumps of collagen that cast drifting shadows on the retina. They can look like translucent threads, cobwebs, or spots that move when your eye moves and dart away when you try to look at them directly. In most people, floaters appear gradually as the clear, gel‑like vitreous slowly liquefies with age.1 Although usually harmless, a sudden shower of new floaters—especially when paired with flashes of light—can signal a retinal tear that needs same‑day care.2 Understanding when floaters are benign and when they are an emergency empowers you to protect your sight.
Symptoms
- Moving specks or threads that drift across vision and fade when you stop chasing them
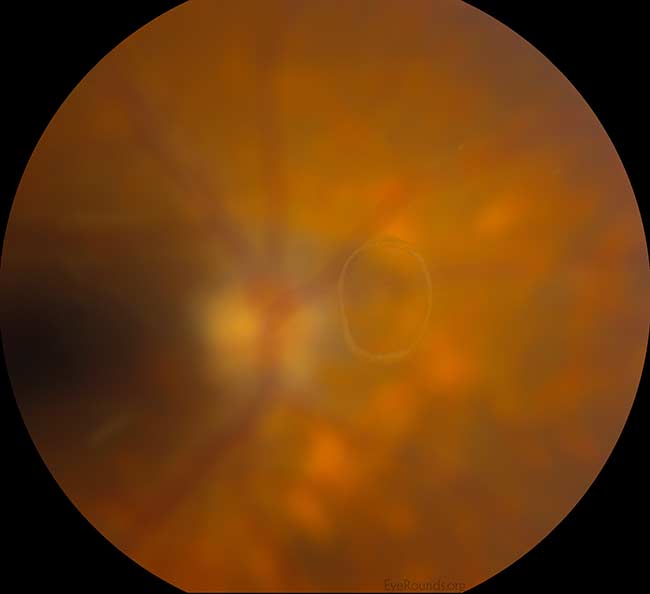
- Shadowy rings (Weiss ring) after a posterior vitreous detachment
- Flashes of light in peripheral vision if the vitreous tugs the retina
- Blurred or hazy spots that clear with blinking
Floaters stand out most against bright, uniform backgrounds such as a blue sky or white wall.3 Occasional floaters that do not change over months are generally harmless. Seek care quickly if you notice a burst of new floaters, flashes, or a curtain‑like shadow—possible signs of retinal detachment.4
Causes and Risk Factors
Common causes
- Age‑related vitreous liquefaction leading to collagen clumping
- Posterior vitreous detachment (PVD)—the vitreous pulls away from the retina, often producing a large circular floater (Weiss ring)5
- Retinal tears or detachments that shed cells into the vitreous6
- Inflammation (uveitis), bleeding, or crystal deposits (asteroid hyalosis)
Risk factors
Retinal Tear Risk After New Floaters
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
An ophthalmologist will dilate your pupils and use slit‑lamp and indirect ophthalmoscopy to inspect the vitreous and retina. Dilated exam rules out retinal tears, detachments, or inflammation. Optical coherence tomography (OCT) can document PVD or subtle retinal holes.7 If inflammation or bleeding is suspected, ultrasound or laboratory tests may follow. Most people leave the office reassured that their floaters are benign; however, follow‑up in two to six weeks helps catch late‑appearing tears.8
Treatment and Management
For typical age‑related floaters, watchful waiting is safest; the brain often learns to ignore them over several months.9 In troublesome cases:
- Nd:YAG vitreolysis uses focused laser pulses to vaporize discrete opacities. A 2017 masked trial showed symptom improvement over sham treatment, but long‑term safety data are limited.10
- Pars plana vitrectomy surgically removes the vitreous gel, eliminating floaters but carrying risks of cataract and retinal detachment. It is reserved for severe, vision‑degrading cases.
- Address underlying disease (e.g., treat uveitis or control diabetes) when secondary floaters appear.
Living with Floaters and Prevention
Most people adjust to benign floaters. Helpful strategies include:
- Move your eyes in gentle circles to shift floaters away from the visual axis.
- Wear sunglasses to reduce glare that makes floaters stand out.
- Keep systemic conditions like diabetes and hypertension well controlled.
- Schedule a prompt dilated exam for any sudden change in floaters or new flashes.11
Remember that sudden floaters, flashes, or a dark curtain may herald retinal detachment, a sight‑threatening emergency requiring same‑day surgery.12
Latest Research & Developments
- Laser advances: Newer ultrafast Nd:YAG platforms use lower pulse energy and computerized eye‑tracking, aiming to minimize retinal risk. Ongoing multicenter trials are comparing modern systems against sham treatment.
- Pharmacologic vitreolysis: Researchers are exploring enzymatic agents that could safely liquefy the vitreous and clear floaters without surgery.
- Updated laser data: The randomized SATURN trials continue to report durable symptom relief at 24 months, though critics note modest sample sizes.1314
Recently Published in Peer-Reviewed Journals
Ophthalmology. Retina
May 15, 2025
Clinical Management of Vision Degrading Myodesopsia from Vitreous Floaters: Observation vs. Limited Refractive Vitrectomy.
Boneva SK, Nguyen JH, Mamou J, et al.
Investigative ophthalmology & visual science
May 1, 2024
Light Scattering by Vitreous of Humans With Vision Degrading Myodesopsia From Floaters.
Paniagua-Diaz AM, Nguyen JH, Artal P, et al.
BMC ophthalmology
October 20, 2023
Vision degrading myodesopsia assessed with optos ultra-widefield scanning laser ophthalmoscope.
Lin T, Shi C, Wu B, et al.
Next Steps
If you experience a sudden shower of floaters, flashes of light, or loss of side vision, contact an eye‑care provider immediately. For routine floaters that simply annoy you, schedule an exam with a retina specialist or comprehensive ophthalmologist to confirm your retina is healthy. Referral paths include calling your optometrist, using your insurance directory, or asking your primary‑care doctor. Many retina clinics offer same‑day urgent appointments for new‑onset floaters. You can also connect directly to a qualified specialist through Kerbside to streamline scheduling and care.
Bring a list of symptoms, medications, and eye‑surgery history to your visit for the most efficient evaluation.1516
Trusted Providers for Eye Floaters

Dr. Emily Eton
Specialty
Retina/Vitreous
Education
Harvard Medical School

Dr. Grayson Armstrong
Specialty
Retina/Vitreous
Education
Ophthalmology

Dr. Jose Davila
Specialty
Retina/Vitreous
Education
Retina/Vitreous Surgery

Dr. Nicholas Carducci
Specialty
Retina/Vitreous
Education
University of Pennsylvania Perelman School of Medicine