Vitrectomy
also known as Pars Plana Vitrectomy, PPV
Last updated August 6, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.


Overview
Vitrectomy is a microsurgical operation that removes the eye’s natural gel (vitreous) so a retina specialist can clear blood, scar tissue or repair a detached retina. Performed through hair-thin ports, the surgery lets light reach the retina again and can prevent permanent vision loss. Most procedures take 30–90 minutes and are done in an outpatient setting with twilight or general anesthesia. Success rates for common problems such as macular hole or vitreous hemorrhage exceed 85 percent, and modern techniques have greatly reduced recovery time.12
How the Procedure Works & Options
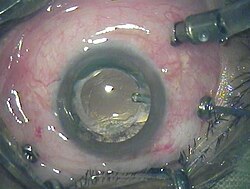
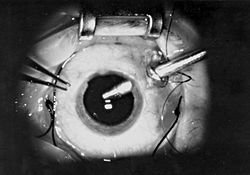
Surgeons enter the eye through the sclera about 3 mm behind the cornea, using tiny cannulas (27-, 25- or 23-gauge). A vitrector cuts and aspirates the cloudy gel while an endo-illuminator lights the retina. Depending on the disease, the surgeon may peel membranes, apply laser, place a gas bubble or fill the eye with silicone oil. Small-gauge systems often seal without stitches, and newer dual-blade cutters allow up to 10 000 cuts per minute, lowering traction on delicate tissue. Choice of tamponade (air, SF₆, C₃F₈, silicone) is customized to each case.12
Who Is a Candidate?
You may be a candidate if you have visually significant floaters, non-clearing vitreous hemorrhage, retinal detachment, macular hole, macular pucker or an infection called endophthalmitis. Good candidates have vision impacted in daily life, a treatable retinal condition and overall health stable enough for anesthesia. Extra discussion is needed in people with uncontrolled glaucoma, recent heart attack or inability to maintain face-down positioning after a gas bubble. Your retina specialist will balance potential vision gain against surgical risks.12
Vitrectomy Suitability Score
Enter your details below to check your suitability for this treatment
Suitability Level
Recommendation
Cost and Price
In the United States, Medicare lists the national average facility and professional fee for outpatient vitrectomy (CPT 67113) at roughly USD 4,200, of which typical Part B coinsurance is 20 percent. Private insurance plans usually follow similar coverage rules once medical necessity is documented. Self-pay prices range from USD 6,000–9,000 per eye, varying by region, surgeon experience, anesthesia type and whether a hospital or ambulatory center is used. Pre-op testing and postoperative drugs can add USD 200–400 to the total.12
Benefits and Limitations
Vitrectomy can restore or stabilize sight, relieve distortion and give surgeons direct access to treat retinal disease. Reported visual improvement rates are 70-90 percent for macular hole and 80 percent for diabetic vitreous hemorrhage. Potential downsides include cataract acceleration, temporary high eye pressure, infection (≈0.05 %), and recurrent detachment. Most complications are manageable, but a small number of eyes may lose vision despite treatment.12
Recovery and Long-Term Care
After surgery you’ll wear an eye shield and use antibiotic-steroid drops for 1–2 weeks. Vision is blurry at first, especially if a gas bubble obscures the view; bubbles absorb over 2–8 weeks. Some patients must keep a face-down posture so the bubble presses the retina flat. Light activity resumes in a few days, but avoid air travel and nitrous-oxide anesthesia until the gas fully dissolves. Full visual recovery can take three months, and yearly retina checks remain important.12
Latest Research & Innovations
Current studies explore 27- and 29-gauge instrumentation, hypersonic liquefaction probes that cut without blades, and intra-operative OCT to guide membrane peeling. A recent meta-analysis found that high-speed dual-blade cutters lower iatrogenic retinal breaks by 35 percent while maintaining surgical efficiency.1 Trials are under way on sustained-release corticosteroid inserts and gene therapy delivered at the time of vitrectomy for diabetic retinopathy.2
Recently Published in Peer-Reviewed Journals
BMC ophthalmology
August 4, 2025
The efficacy of the three-port bimanual technique for direct perfluorocarbon liquid-silicone oil exchange in vitrectomy for the treatment of advanced proliferative vitreoretinopathy.
Zhang Z, Zhang X, Wang M, et al.
Ophthalmology. Retina
July 31, 2025
Retinoschisis after Incomplete Posterior Vitreous Detachment Vitrectomy.
Chou JF, Cheng CY, Chuang CC
Ophthalmology. Retina
July 31, 2025
Association of Low Serum Vitamin D Levels with Proliferative Vitreoretinopathy After Rhegmatogenous Retinal Detachment Repair.
Ness S, Mitsiades R, Poulaki V
Next Steps
If you notice sudden floaters, flashes, or a curtain over your vision—or if a chronic retinal condition is limiting your quality of life—schedule a prompt evaluation. A retina specialist will perform dilated imaging, discuss your medical history and outline whether vitrectomy or an alternative treatment is best. You can connect with the right specialist on Kerbside for a medical-education consult—no physician-patient relationship will be created.12