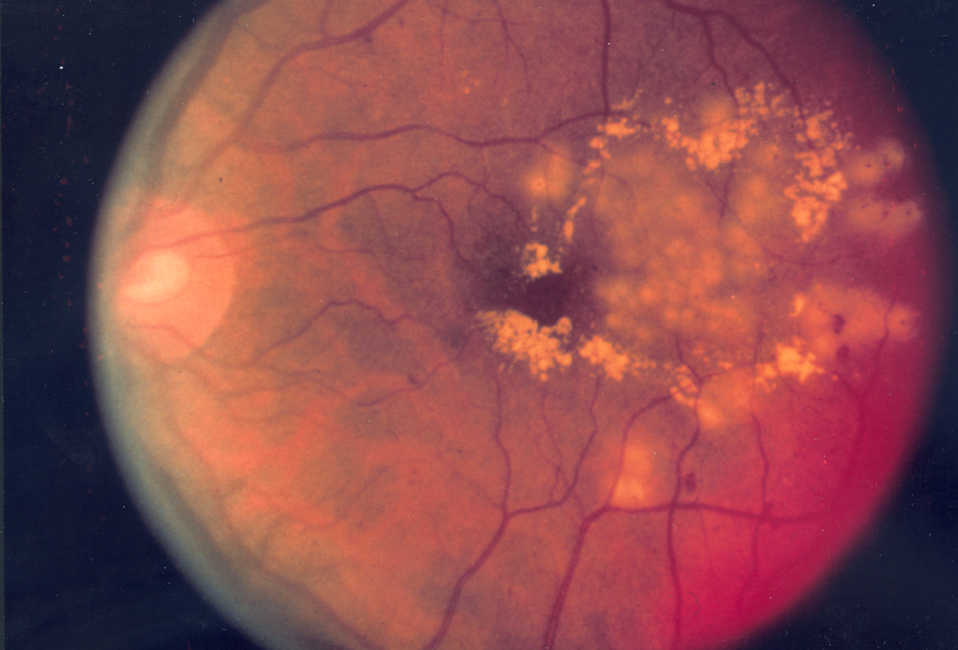
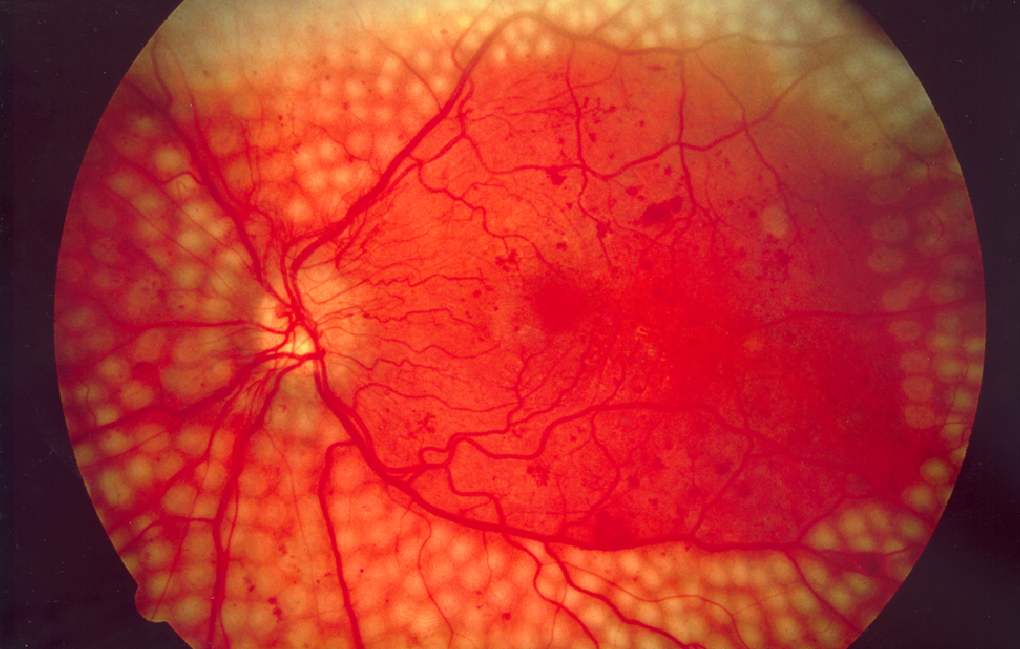
Diabetic Retinopathy
Last updated July 24, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.

Overview
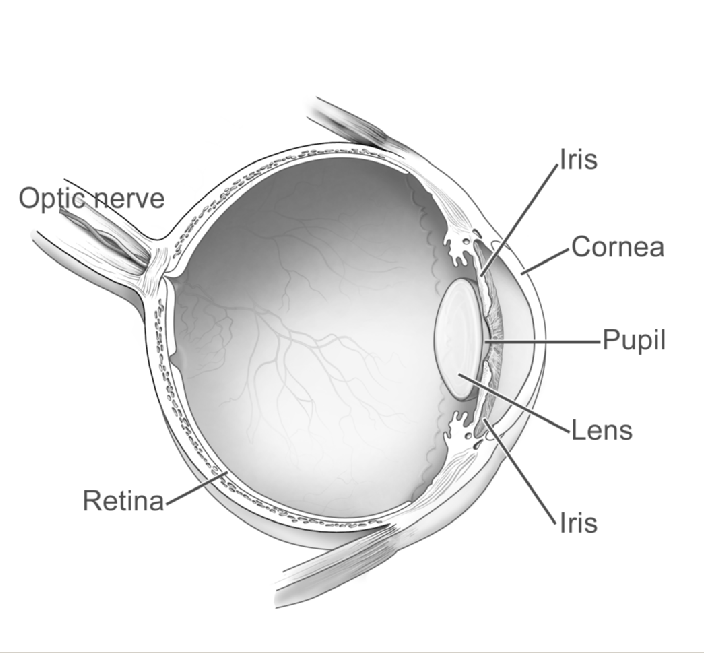
Diabetic retinopathy (DR) is a diabetes-related eye disease that harms the tiny blood vessels lining the retina—the light-sensing tissue at the back of your eye. Over time, high blood-sugar levels weaken these vessels, causing them to leak, close off, or grow abnormally. Left untreated, these changes can blur vision and eventually lead to permanent blindness. DR is one of the leading causes of preventable vision loss in working-age adults. Because early DR is usually silent, annual dilated eye exams are essential for catching problems early and starting treatment before vision is threatened 1. In the United States alone, an estimated 9.6 million people live with DR, including 1.8 million with sight-threatening forms 2.
Symptoms
Most people notice no symptoms in the early stages. As damage worsens, you may experience:
- Blurry or fluctuating vision
- Dark floaters or cobweb-like shapes
- Faded colors
- Dark or empty areas in your field of view
- Sudden vision loss (often from bleeding or retinal detachment)
If you suddenly see many new floaters, flashing lights, or a shadow across your vision, seek emergency eye care—these can signal a retinal detachment or hemorrhage that needs same-day treatment 3 4.
Causes and Risk Factors
DR is driven by chronically elevated blood glucose, which damages retinal capillaries. Key risk factors include:
- Longer duration of diabetes (type 1 or type 2)
- Poor glycemic control (high A1C)
- High blood pressure and high cholesterol
- Smoking
- Pregnancy
- Certain racial/ethnic groups (e.g., Black, Hispanic, Native American)
The longer you have diabetes, the higher your likelihood of developing DR—over half of people with diabetes will develop some stage after 20 years 5. Good control of blood sugar, blood pressure, and lipids can cut the risk of vision-threatening DR by up to 60 percent 6.
Diabetic Retinopathy Risk Estimator
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
DR is diagnosed during a comprehensive dilated eye exam. Your ophthalmologist may use:
- Optical Coherence Tomography (OCT) – cross-sectional images that reveal retinal swelling or fluid.
- Fluorescein Angiography – a dye test that highlights leaking or closed vessels.
- Fundus photography or OCT-Angiography for detailed documentation.
New FDA-cleared autonomous AI systems (e.g., IDx-DR, EyeArt) can screen for more-than-mild DR in primary-care settings, improving access where eye specialists are scarce 7 8.
Treatment and Management
While there is no cure, timely treatment can halt—or even reverse—vision loss.
- Anti-VEGF injections (ranibizumab, aflibercept, faricimab) shrink leaking vessels and reduce swelling.
- Laser photocoagulation (focal or pan-retinal) seals leaky areas and prevents abnormal vessel growth.
- Vitrectomy removes blood, scar tissue, or the gel-like vitreous in advanced cases.
The 2024 AAO Preferred Practice Pattern recommends anti-VEGF as first-line for center-involved diabetic macular edema and proliferative DR 9. Emerging data show anti-VEGF may also prevent progression when given earlier 10.
Living with Diabetic Retinopathy and Prevention
Daily diabetes care is your strongest defense against vision loss. Experts recommend:
- A1C <7 percent (or individualized target)
- Blood-pressure goal <130/80 mm Hg
- LDL cholesterol in guideline range
- No smoking; moderate exercise most days
- Yearly—or more frequent—dilated eye exams
Maintaining healthy numbers can cut DR risk dramatically, and prompt treatment of blood-sugar spikes protects the retina 11. These recommendations align with the American Diabetes Association’s 2025 Standards of Care 12.
Latest Research & Developments
Research is rapidly expanding treatment options and reducing the burden of frequent injections:
- Gene therapy RGX-314 (AbbVie/Regenxbio) is entering Phase 3 trials to provide long-term anti-VEGF expression after a single in-office injection 13.
- Port Delivery System with ranibizumab (Susvimo) showed non-inferior vision outcomes to monthly injections for diabetic macular edema while requiring refills only twice yearly 14.
- Next-generation AI tools and OCT-angiography are improving early detection and individualized risk profiling.
Recently Published in Peer-Reviewed Journals
American journal of ophthalmology
July 18, 2025
Burden and Predictors of Undetected Eye Disease in Adult African Americans: African American Eye Disease Study (AFEDS).
Dhablania N, Torres M, Burkemper B, et al.
Investigative ophthalmology & visual science
July 1, 2025
Exosomal miRNA Profiling in Liquid Biopsy of Vitreous in Proliferative Diabetic Retinopathy.
Yan B, Qiu J, Yang Y, et al.
Investigative ophthalmology & visual science
July 1, 2025
Predictors of Final Visual Outcome in Patients With Leber Hereditary Optic Neuropathy Treated With Lenadogene Nolparvovec Gene Therapy.
Sergott RC, Carelli V, Newman NJ, et al.
Next Steps
If you have diabetes—or notice any vision changes—schedule a comprehensive dilated eye exam as soon as possible. Most adults with diabetes need an exam every 12 months; pregnant patients often need more frequent checks 15. For specialized care, look for an ophthalmologist who focuses on the retina. The American Academy of Ophthalmology’s “Find an Ophthalmologist” directory lets you search specifically for Retina/Vitreous specialists in your area 16. Early detection, meticulous diabetes control, and prompt referral to a retina doctor remain the best recipe for protecting sight.
Trusted Providers for Diabetic Retinopathy

Dr. Emily Eton
Specialty
Retina/Vitreous
Education
Harvard Medical School

Dr. Grayson Armstrong
Specialty
Retina/Vitreous
Education
Ophthalmology

Dr. Jose Davila
Specialty
Retina/Vitreous
Education
Retina/Vitreous Surgery

Dr. Nicholas Carducci
Specialty
Retina/Vitreous
Education
University of Pennsylvania Perelman School of Medicine