Diabetic Macular Edema
Also known as DME
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.


Overview
Diabetic macular edema (DME) happens when diabetes causes tiny blood vessels in the back of the eye to leak. Fluid builds up in the macula—the spot that lets you read, drive, and see faces clearly—so vision becomes blurry or distorted. DME is a common cause of vision loss in people with diabetes, but modern treatments can help protect sight. 1
DME usually develops as part of diabetic retinopathy. Not everyone with retinopathy gets DME, but anyone with diabetes can be at risk. Good control of blood sugar, blood pressure, and cholesterol helps lower that risk. 2
Symptoms
DME often starts quietly. Many people do not notice changes until the swelling affects center vision. Symptoms can include:
- Blurry or wavy central vision (straight lines look bent).
- Colors may look faded.
- Trouble reading, recognizing faces, or seeing fine details.
- Pain is uncommon.
Regular dilated eye exams can catch DME early—before you notice vision changes. 3
Causes and Risk Factors
High blood sugar damages small retinal vessels. They can leak fluid and proteins into the macula, causing swelling. Over time, this swelling blurs vision.
Risk factors:
- Longer time with diabetes and higher A1c.
- High blood pressure and high cholesterol.
- Kidney disease, pregnancy, or sleep apnea.
- Existing diabetic retinopathy.
Keeping A1c, blood pressure, and cholesterol in target ranges lowers the chance of DME and slows worsening if it starts. 4 Helpful exam clues and imaging details are summarized by the American Academy of Ophthalmology’s EyeWiki. 3
DME: Simple 5-Factor Risk of Vision Impact (Assumption-Based)
Select your details to estimate risk factors.
Diagnosis
Your eye doctor will do a full exam. Common tests include:
- Dilated exam and retinal photos to look for leaking vessels and deposits.
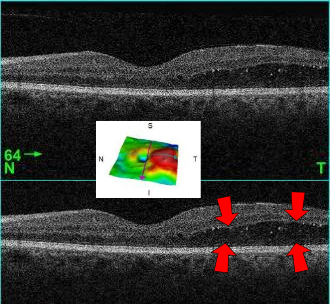
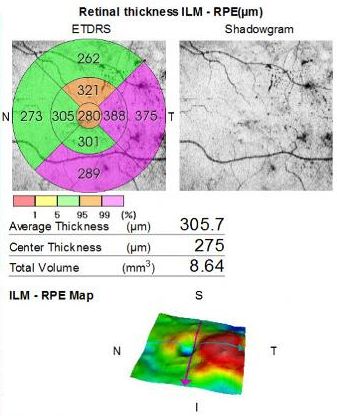
- OCT (Optical Coherence Tomography) to measure macular thickness and see tiny fluid pockets.
- Fluorescein angiography in selected cases to find exact leak areas or poor blood flow.
OCT is the main tool to confirm DME and to track response to treatment over time. 1 Clinical signs and OCT features are outlined on EyeWiki. 3
Treatment and Management
The main goal is to reduce swelling and protect vision. Your retina specialist will customize the plan based on involvement and vision.
- Anti-VEGF injections: Medicines like aflibercept, ranibizumab, or bevacizumab help reduce leakage and swelling. 5
- Observation: If center swelling is present but vision is good (20/25 or better), close monitoring may be reasonable. 6
- Focal/grid laser: Targeted laser may be used alone or with injections.
- Steroids: Short or long-acting forms may be used when anti-VEGF is not enough or unsuitable.
- Systemic care: Optimizing blood sugar, blood pressure, and cholesterol improves outcomes.
Costs & Practical Tips:
- Ask about drug options and insurance coverage.
- Injections may start monthly and then be spaced out if stable.
- Laser and steroid costs vary; request pre-estimates.
Many people need ongoing care. Sticking to the plan gives the best chance to keep vision. Evidence comes from DRCR Retina Network trials. 5 6
Living with Diabetic Macular Edema and Prevention
DME is manageable. Protect your vision by:
- Keeping regular eye visits and tests.
- Tracking A1c, blood pressure, and cholesterol.
- Following healthy routines: medication adherence, balanced diet, regular exercise, and no smoking.
- Watching for changes like worsening reading vision or distorted faces.
Latest Research & Developments
Long-term outcomes: With consistent follow-up, many patients keep vision gains from anti-VEGF therapy. 7
Newer medicines: Faricimab, which targets VEGF-A and Ang-2, may allow treatment intervals as long as 12–16 weeks for some patients. 8
Recent Peer-Reviewed Research
Quantifying the correlation of ocular manifestations and macular pigment optical density in albinism: a prospective cross-sectional study.
Bingöl Kızıltunç P, Atilla H
Quantifying Choriocapillaris Flow Deficits in Diabetic Retinopathy Using Projection-Resolved OCT Angiography.
Wang J, Hormel T, Park DW, et al.
Association of Anti-VEGF Therapy with Reported Ocular Adverse Events: A Global Pharmacovigilance Analysis.
Lakhani M, Kwan ATH, Kundapur D, et al.
Next Steps
If you have diabetes and notice vision changes, see a retina specialist. Your optometrist or general ophthalmologist can refer you.
- Ask for a "diabetic macular edema evaluation" when scheduling.
- Bring glasses/contact info, medication list, recent labs, and prior eye records.
- Request the cancellation list for sooner appointments.
You can also use Kerbside for a medical education consult to prepare for your visit (educational only).