Anti-VEGF Intravitreal Therapy
also known as Anti-VEGF
Last updated August 20, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.


Overview
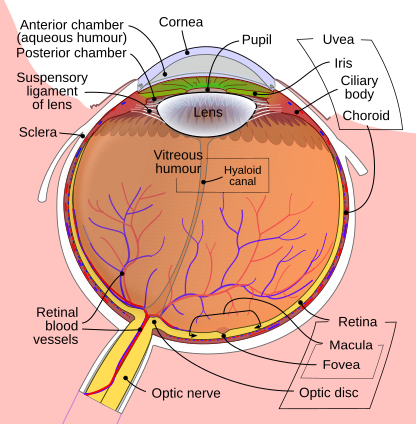
Anti-vascular endothelial growth factor (anti-VEGF) injections are the mainstay treatment for sight-threatening conditions such as wet age-related macular degeneration (AMD), diabetic macular edema (DME), and macular edema after retinal vein occlusion. By blocking VEGF, these medicines stop leaky, abnormal blood vessels from damaging the retina and can even improve vision. Several FDA-approved agents—ranibizumab, aflibercept, faricimab, and brolucizumab—are given directly into the eye in the office. Most patients notice retinal drying and sharper central vision after the first few doses, with continued benefit when therapy is maintained.12
How the Procedure Works & Options
The eye is numbed with topical anesthetic drops, the surface is cleaned with iodine, and a tiny needle delivers 0.05 mL of medication into the vitreous cavity. The drug rapidly diffuses to the macula, binding VEGF within minutes. Most regimens begin with monthly injections, then extend to every 8–16 weeks once the retina is dry (treat-and-extend). Three common molecules—bevacizumab (off-label), ranibizumab, and aflibercept—showed equivalent one-year vision gains in the landmark CATT and DRCR trials, while newer agents like faricimab combine dual-target inhibition for longer durability.34
Who Is a Candidate?
Adults with active choroidal neovascularization from wet AMD, center-involved DME, macular edema after vein occlusion, or myopic CNV benefit most. Candidacy is especially strong when:
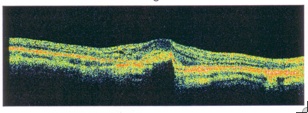
- Optical coherence tomography (OCT) shows intra- or sub-retinal fluid
- Visual acuity ranges between 20/30 and 20/400
- Patients can attend follow-up every 4–8 weeks
Anti-VEGF is less effective for geographic atrophy, chronic scar tissue, or eyes with end-stage vision loss. Comparative AAO data suggest treatment halved blindness from AMD in countries with robust access.56
Anti-VEGF Suitability Score
Enter your details below to check your suitability for this treatment
Suitability Level
Recommendation
Benefits and Limitations
Benefits
• Stabilizes or improves vision in up to 90 % of treated eyes.
• Rapidly reduces fluid and hemorrhage, often within weeks.
• Flexible dosing (treat-and-extend, PRN) minimizes unnecessary visits.
Limitations
• Requires repeated injections—often 6–8 times the first year.
• Vision can decline quickly if follow-ups are missed.
• Small but real risks of infection and stroke.
The DRCR Retina Network’s Protocol T showed aflibercept, bevacizumab, and ranibizumab all improved DME, with aflibercept offering a modest edge in eyes starting below 20/50.78
Risks and Side Effects
Common temporary effects include mild irritation, tiny floaters, and a red subconjunctival spot. Serious complications are rare:
- Endophthalmitis (≈0.03 % per injection)
- Retinal tear or detachment (≤0.01 %)
- Very small increases in stroke risk in patients with vascular disease
Proper sterile technique—povidone-iodine prep, mask use, and a new needle for each eye—keeps infection rates low.910
Recovery and Long-Term Care
Most people resume normal activities the same day. Your doctor will:
- Re-examine the retina and check OCT 4–6 weeks after each injection.
- Gradually lengthen the interval once fluid is dry.
- Continue AREDS2 vitamins, smoking cessation, and systemic control of diabetes or blood pressure.
Treat-and-extend schedules cut clinic visits by 30–40 % while maintaining vision in multiple real-world studies.1112
Latest Research & Innovations
Long-acting delivery systems aim to reduce treatment burden. The refillable Susvimo port-delivery implant releases ranibizumab for six months or more, while gene-therapy trials deliver anti-VEGF–secreting vectors in a single procedure. Faricimab, a bispecific antibody blocking both VEGF-A and Ang-2, extends dosing to 16 weeks in many eyes. Phase 3 Archway and Pagoda studies support non-inferiority of port delivery to monthly injections.1314
Recently Published in Peer-Reviewed Journals
BMC ophthalmology
July 31, 2025
Comparative efficacy of photodynamic therapy (PDT), ranibizumab, aflibercept monotherapy, and combination therapies for polypoidal choroidal vasculopathy: a network meta-analysis of randomized controlled trials.
Quiroz-Reyes MA, Quiroz-Gonzalez EA, Quiroz-Gonzalez MA, et al.
Ophthalmology
July 28, 2025
Disparities in Presentation & Anti-VEGF Therapy Initiation for Neovascular AMD: An Analysis of the Academy IRIS® Registry.
Acharya B, Momenaei B, Zhang Q, et al.
Retina (Philadelphia, Pa.)
July 22, 2025
Optical coherence tomography angiography (OCTA) analysis of cohort with peripapillary choroidal neovascularization.
Heinke A, Agnihotri A, Nagel ID, et al.
Next Steps – See a Retina Specialist
If you notice straight lines appearing wavy, have new central blur, or have been told fluid is present on OCT, schedule an appointment with a retina specialist. They will image your macula, discuss injection schedules, and explain how anti-VEGF therapy fits with your lifestyle. Connect with the right expert on Kerbside and take control of your vision journey today.
Bring your medication list and recent blood-sugar or blood-pressure readings to make the visit even more productive.1516
Trusted Providers for Anti-VEGF Intravitreal Therapy

Dr. Emily Eton
Specialty
Retina/Vitreous
Education
Harvard Medical School

Dr. Grayson Armstrong
Specialty
Retina/Vitreous
Education
Ophthalmology

Dr. Jose Davila
Specialty
Retina/Vitreous
Education
Retina/Vitreous Surgery

Dr. Nicholas Carducci
Specialty
Retina/Vitreous
Education
University of Pennsylvania Perelman School of Medicine