Wet Age-Related Macular Degeneration
also known as Wet AMD
Last updated August 21, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.
Overview
Wet age-related macular degeneration (wet AMD) happens when fragile, abnormal blood vessels grow under the macula and leak fluid or blood. This damages the part of the retina that gives us sharp, straight-ahead vision.
Wet AMD is less common than the dry form but can cause faster vision loss. The good news: modern treatments can slow or stop the damage in many people.
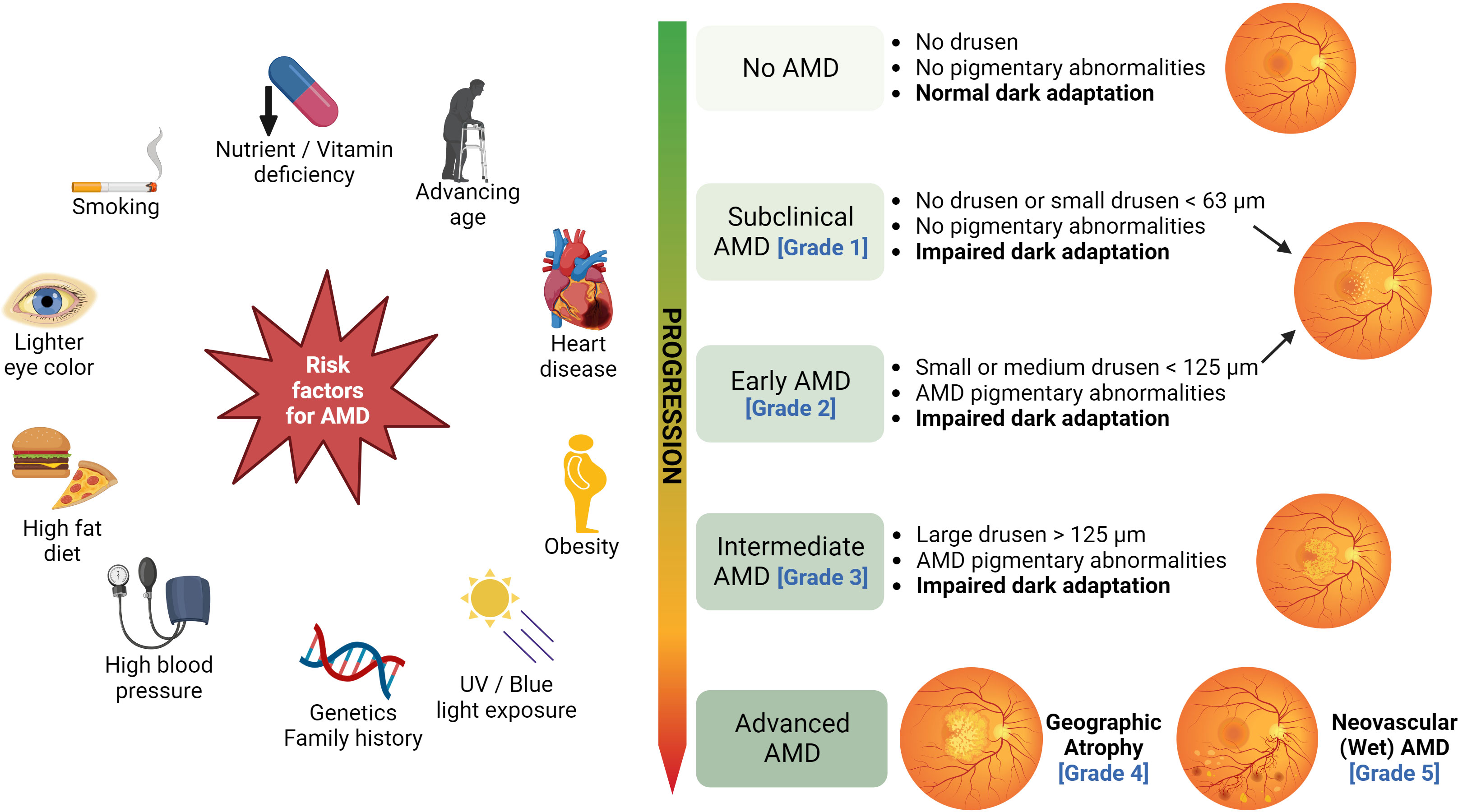
AMD overall is a leading cause of central vision loss in older adults and often starts as the dry type before progressing to the wet type in some people. 1 2
Symptoms
Wet AMD symptoms usually begin in one eye and may come on suddenly. Common signs include:
- Blurry or dark spot in the center of your vision (noticed while reading or recognizing faces).
- Distortion — straight lines look wavy or bent (metamorphopsia).
- Colors appear faded or washed out.
- Need for brighter light and trouble seeing in low light.
If you notice these changes, call an eye doctor right away. Early treatment gives the best chance to protect vision.
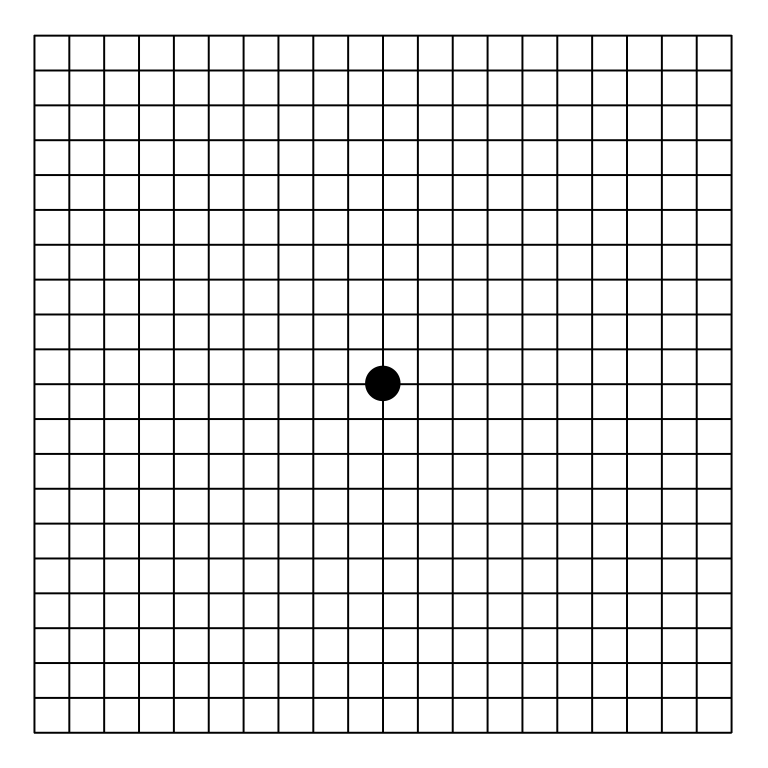
Many people use an at-home Amsler grid to check for new waves or blank spots between visits. 3 4
Causes and Risk Factors
In wet AMD, new blood vessels grow from the choroid (a layer behind the retina). These vessels are weak and tend to leak. Over time, leaking causes swelling, scarring, and central vision loss.
You can’t do anything about age — the biggest risk factor — but you can address others. Key risks include:
- Age 55+ and a family history of AMD.
- Smoking — the most important modifiable risk; it raises the chance of AMD and speeds progression.
- Light skin/European ancestry and certain genetic variants.
- Cardiovascular factors such as high blood pressure.
Stopping smoking and managing overall health can help lower risk. 5 6
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
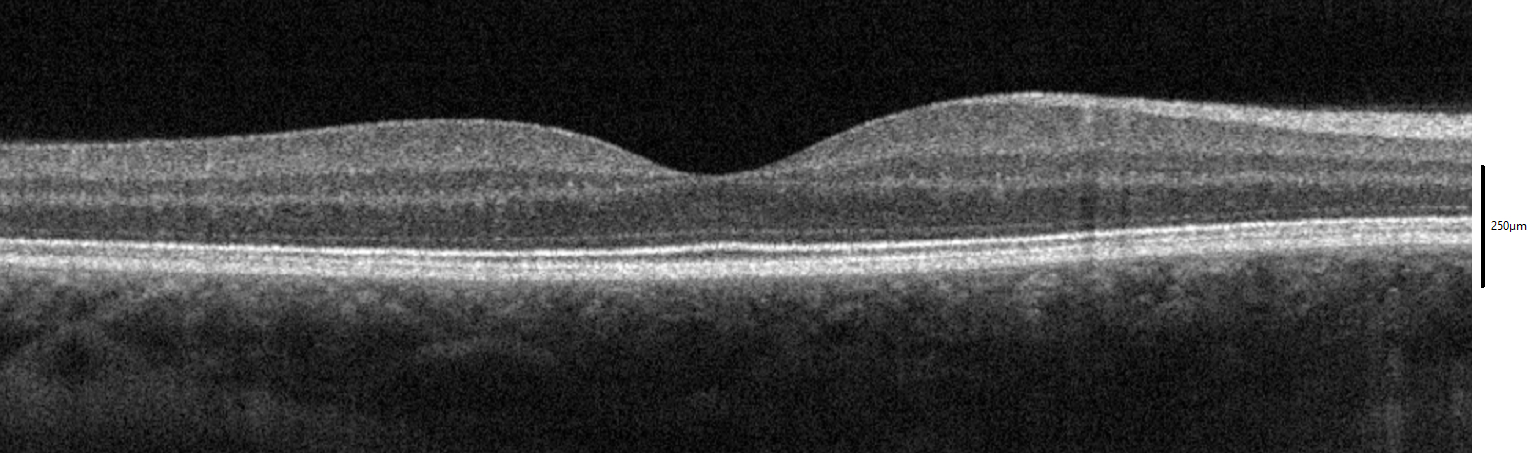
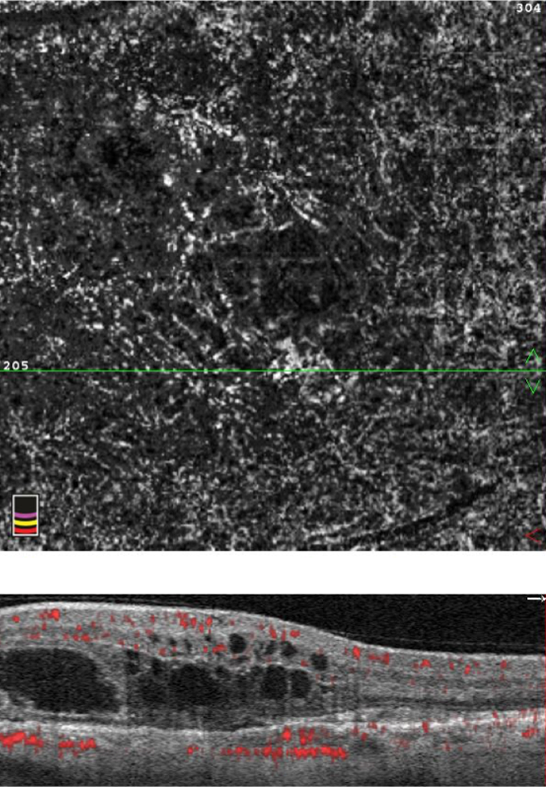
To check for wet AMD, an eye doctor will perform a dilated eye exam and specialized imaging:
- Optical coherence tomography (OCT): a painless scan that shows swelling, fluid, or bleeding under the retina.
- Fluorescein or indocyanine green angiography: a dye test that highlights leaking blood vessels.
- Amsler grid: to monitor central distortion between visits.
These tests help confirm wet AMD and guide treatment plans. 7 4
Treatment and Management
The main treatment for wet AMD is anti-VEGF injections. These medicines (such as aflibercept, ranibizumab, faricimab, or off-label bevacizumab) block a growth signal called VEGF, helping stop leaks and new vessel growth.
Injections are given in the office. Many people start with monthly doses and then move to a “treat-and-extend” schedule where visits gradually space out if the eye stays quiet.
- Photodynamic therapy (PDT) for certain lesion types.
- Thermal laser in rare situations away from the very center of vision.
- Low-vision rehabilitation (magnifiers, lighting, training) to make day-to-day tasks easier.
Your retina specialist will tailor a plan based on how your eye responds. 8 1
Living with Wet AMD and Prevention
You can take steps that support eye health and make life easier:
- Don’t smoke. If you smoke, ask your doctor for help to quit.
- Use an Amsler grid daily (one eye at a time). If you notice new waviness or a dark spot, contact your eye doctor.
- Protect your heart health: manage blood pressure, cholesterol, and diabetes with your primary care team.
- Nutrition: If you have intermediate AMD or advanced AMD in one eye, AREDS2 vitamins can lower the chance of progression to late AMD (but they are not a cure).
Routine follow-up is critical: keep injection and monitoring visits so problems are caught early. 9 2
Latest Research & Developments
Research is focused on making treatment more durable so people need fewer injections. Examples:
Recently Published in Peer-Reviewed Journals
The British journal of ophthalmology
August 18, 2025
Advanced imaging of corneal neovascularisation with a novel swept-source AS-OCTA system.
Lucchino L, Vaccaro S, Airaldi M, et al.
BMC ophthalmology
August 18, 2025
Multimodal imaging of tumour-related lipid exudation and exudative retinal detachment following brachytherapy in choroidal melanoma.
Ros-Sanchez E, Oliver-Gutierrez D, Buck P, et al.
BMC ophthalmology
August 18, 2025
Clinical characteristics and risk factors of ocular hypertension: a case-control study.
Hu F, Luo L, Yang H, et al.
Next Steps
Who to see: A retina specialist (ophthalmologist) is the best clinician for suspected or known wet AMD.
How to schedule: If you have new central blur, wavy lines, or a dark spot, ask for an urgent appointment. Clinics often reserve same-day or next-day slots for sudden vision changes.
If your primary eye doctor or PCP needs to refer you, request that they mark the referral as urgent and send recent notes and imaging.
If appointments are full, ask to be placed on a cancellation list and check nearby practices.
After the visit: Follow the treatment plan, return for all injections/monitoring, and use an Amsler grid at home. If you want a second opinion or education about options, you can connect directly with a board-certified retina specialist on Kerbside for a medical education consult (this does not establish a patient–physician relationship).
Trusted Providers for Wet Age-Related Macular Degeneration

Dr. Emily Eton
Specialty
Retina/Vitreous
Education
Harvard Medical School

Dr. Grayson Armstrong
Specialty
Retina/Vitreous
Education
Ophthalmology

Dr. Jose Davila
Specialty
Retina/Vitreous
Education
Retina/Vitreous Surgery
Dr. Nicholas Carducci
Specialty
Retina/Vitreous
Education
University of Pennsylvania Perelman School of Medicine