Macular Edema
Last updated July 31, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.
Overview
Macular edema is a sight‑threatening condition in which fluid leaks from damaged retinal blood vessels and collects within the macula—the small, central area of the retina responsible for sharp, detailed vision. As the macula swells and thickens, central vision becomes blurred or distorted.1 Although macular edema most often occurs in people with diabetic retinopathy, it can also arise after eye surgery, vein occlusion, uveitis, age‑related macular degeneration, or trauma.2 Early diagnosis and timely treatment—usually a combination of medicines injected into the eye, laser therapy, or surgery—can preserve or restore vision in most cases.
Symptoms
Macular edema may develop gradually or suddenly, and early stages can be symptom‑free. When symptoms occur, they typically include:
- Blurry or fuzzy central vision that makes it hard to read or recognize faces.
- Colors that appear washed out or less vivid.
- Wavy (distorted) straight lines on a grid or door frame.
- Dark or blind spot in the center of vision.
Because peripheral (side) vision is often intact, you might not notice the problem until everyday tasks become difficult.3 People with diabetes should watch for any change in vision and report it promptly; studies show that close monitoring combined with timely treatment can maintain good vision in eyes that still see 20/25–20/32 at baseline.4
Causes and Risk Factors
The macula can swell whenever the delicate retinal capillaries are weakened or inflamed. Major causes and risk enhancers include:
- Diabetes — especially >10 years’ duration or poor glycemic control.5
- Hypertension, high cholesterol, and kidney disease, which further stress retinal vessels.
- Retinal vein occlusion (branch or central) leading to back‑up of venous pressure and leakage.
- Recent eye surgery (post‑cataract Irvine–Gass syndrome) or ocular trauma.
- Chronic uveitis or other inflammatory diseases.
- Use of certain medications, such as prostaglandin‑analog eye drops.
Poor systemic control of blood sugar (HbA1c >9%) and long‑standing diabetes roughly double the 5‑year risk of diabetic macular edema.6
Macular Edema Risk Score
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
A comprehensive retinal exam includes:
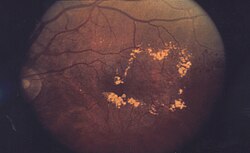
- Dilated ophthalmoscopy and fundus photography to document exudates, hemorrhages, or cystoid changes.
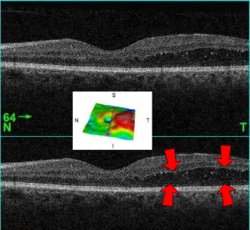
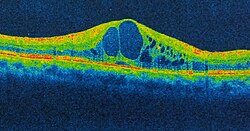
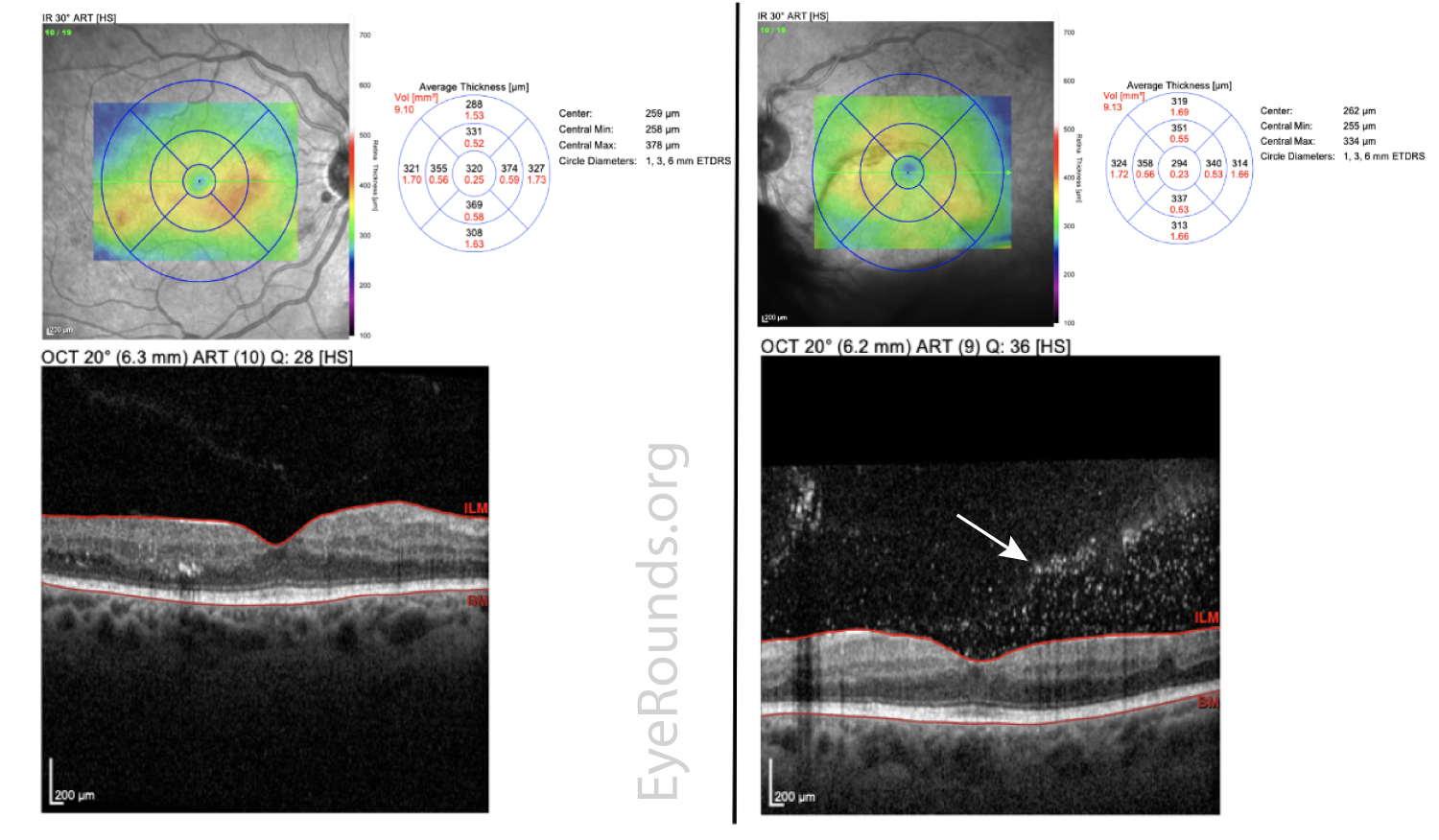
- Optical coherence tomography (OCT)—the gold‑standard, non‑invasive scan that measures retinal thickness and reveals fluid pockets.7
- Fluorescein angiography to identify leaking micro‑aneurysms or blocked capillaries when planning laser treatment.8
Baseline OCT thickness maps establish severity, guide therapy choice, and allow objective monitoring of response to treatment.
Treatment and Management
Management is tailored to the underlying cause, severity, and visual impact:
- Intravitreal anti‑VEGF injections (aflibercept, ranibizumab, faricimab) reduce vascular leakage and are first‑line for diabetic or vein‑occlusion‑related edema. In a landmark DRCR.net trial, aflibercept (Eylea) yielded greater visual gains than bevacizumab in eyes starting at 20/50 or worse.9
- Focal or grid laser photocoagulation seals micro‑aneurysms when edema is non‑center‑involving or persistent after injections.10
- Corticosteroid therapy—either injectable (triamcinolone), implant (dexamethasone), or sustained‑release fluocinolone—helps inflammatory or refractory cases.
- Emerging therapies: faricimab (Vabysmo®) received FDA approval in 2022 for diabetic macular edema, offering a dual VEGF/Ang‑2 blockade and longer dosing intervals.11
Optimal systemic control of blood glucose, blood pressure, and lipids is crucial and synergistic with ocular treatments.
Living with Macular Edema and Prevention
You can protect your vision and overall eye health by:
- Keeping HbA1c below 7%, monitoring blood pressure, and managing cholesterol with your primary‑care team.12
- Scheduling dilated retinal exams at least once a year—or every 2–4 months if you already have edema.
- Following the injection schedule your retina specialist recommends; missing visits risks irreversible vision loss.
- Adopting a healthy lifestyle: balanced diet, regular exercise, smoking cessation, and limiting alcohol.
- Understanding “step‑therapy” options: some patients start with lower‑cost bevacizumab and switch to aflibercept if needed—an approach shown to achieve comparable vision with fewer injections.13
Latest Research & Developments
Research is rapidly advancing:
- Sustained‑release corticosteroid versus methotrexate: An NEI‑funded trial found repeat steroid injections offered superior visual outcomes for uveitic macular edema.14
- OCT biomarkers such as disorganization of retinal inner layers (DRIL) predict visual acuity better than retinal thickness alone, guiding individualized care.15
- Preventive anti‑VEGF in non‑proliferative diabetic retinopathy lowers the rate of edema but shows no long‑term visual benefit, underscoring the importance of treating only when necessary.16
- Gene‑therapy and nanoparticle drug delivery platforms are in early‑phase trials aiming for once‑a‑year treatments.
Recently Published in Peer-Reviewed Journals
Retina (Philadelphia, Pa.)
July 23, 2025
Impact of the Dexamethasone Implant on Slowing Diabetic Retinopathy Progression: Post Hoc Analysis of the MEAD Study.
Blinder KJ, Wykoff CC, Ferencz JR, et al.
BMC ophthalmology
July 15, 2025
Clinical observations and outcomes of dengue-associated retinopathy at a tertiary eye hospital in Nepal.
Pradhan E, Gurung R, Shrestha S, et al.
Retina (Philadelphia, Pa.)
July 14, 2025
IMPACT OF FARICIMAB VERSUS AFLIBERCEPT ON EPIRETINAL MEMBRANE FORMATION OVER 2 YEARS IN PATIENTS WITH DIABETIC MACULAR EDEMA IN THE PHASE 3 YOSEMITE AND RHINE TRIALS.
Jaffe GJ, Deák G, Gibson K, et al.
Next Steps – See a Retina Specialist Promptly
Who to see: The ideal provider is a retina specialist—an ophthalmologist with fellowship training in medical and surgical diseases of the retina.
How to schedule: Ask your primary eye‑care doctor or endocrinologist for an urgent referral if you notice new blurring, waviness, or difficulty reading. Retina clinics often reserve same‑day slots for sudden vision changes. You can also self‑refer to hospital‑based eye institutes with advanced imaging and injection facilities.17
What Kerbside offers: Our platform helps match you directly with board‑certified retina specialists for second opinions, injection scheduling, and long‑term follow‑up. Early engagement is key—most patients maintain 20/40 or better vision when treatment begins before severe edema develops.18
Trusted Providers for Macular Edema

Dr. Emily Eton
Specialty
Retina/Vitreous
Education
Harvard Medical School

Dr. Grayson Armstrong
Specialty
Retina/Vitreous
Education
Ophthalmology

Dr. Jose Davila
Specialty
Retina/Vitreous
Education
Retina/Vitreous Surgery

Dr. Nicholas Carducci
Specialty
Retina/Vitreous
Education
University of Pennsylvania Perelman School of Medicine