Vabysmo
also known as Faricimab-svoa
Last updated August 21, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.
Overview
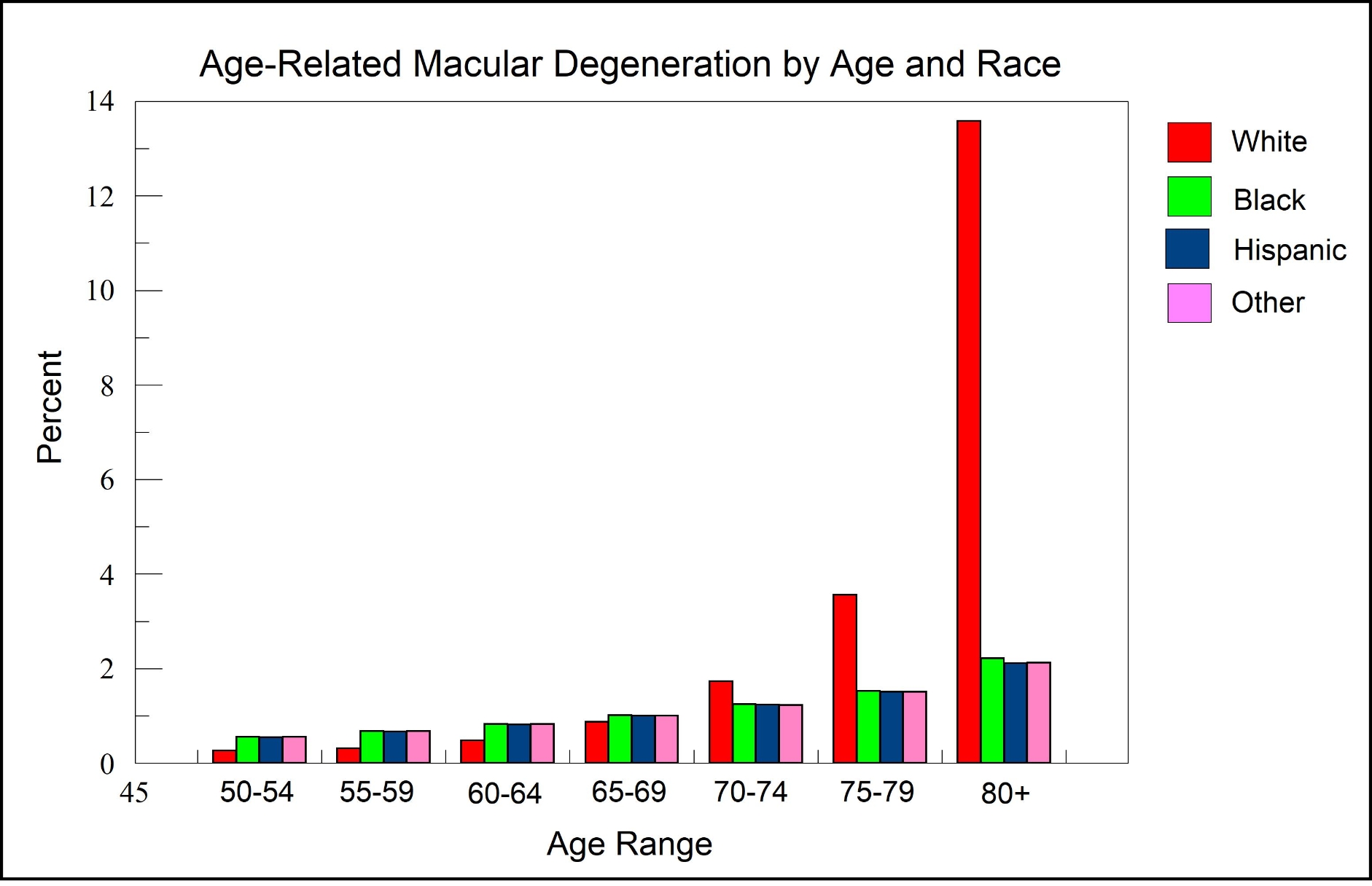
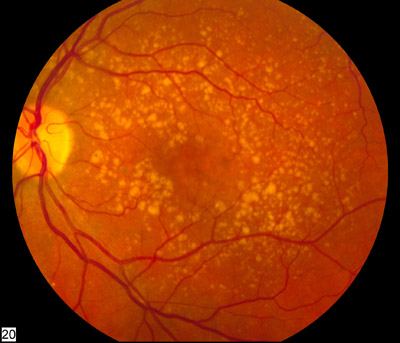
Vabysmo (faricimab-svoa) is a medicine given as an injection into the eye to treat three common retinal diseases: neovascular ("wet") age-related macular degeneration (nAMD), diabetic macular edema (DME), and macular edema following retinal vein occlusion (RVO). It can be dosed as often as every 8 weeks, and many patients can space treatments to every 12–16 weeks once the eye is stable, following the FDA label and your doctor’s plan. 1 Wet AMD damages the macula (the sharp-vision center of the retina) and can cause fast vision loss without treatment, making timely care very important. 2
Our goal with Vabysmo is to control leakage and swelling, protect central vision, and reduce how often you need injections over time, when possible. Many people notice clearer, sharper vision and less distortion as fluids dry up and the macula gets healthier.
How the Procedure Works & Options
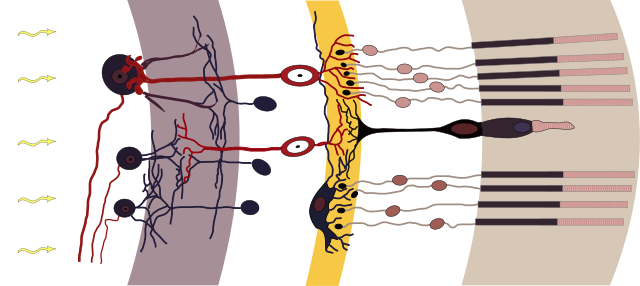
Vabysmo is a bispecific antibody. It blocks two pathways that drive leaking and abnormal vessel growth in retinal disease: VEGF-A and Angiopoietin-2 (Ang-2). By calming both, Vabysmo helps blood vessels stabilize and reduces swelling in the macula. 3 The medicine is placed directly into the eye (the vitreous) during a short in-office procedure using numbing drops and antiseptic to keep you comfortable and safe. 4
Common dosing paths include an initial “loading” phase (more frequent visits early) followed by treat-and-extend or fixed-interval maintenance, often stretching to 8–16 weeks if the eye stays quiet. Your retina specialist will tailor the plan to your OCT scans, vision, and exam. Options can be adjusted over time if your eye needs more or less treatment to stay dry and stable.
Who Is a Candidate?
You may be a good candidate if you have wet AMD, DME, or macular edema after a retinal vein occlusion and your retina specialist recommends anti-VEGF/Ang-2 therapy. The FDA label lists these uses and also notes you should not receive an injection if you have an eye or eyelid infection or active eye inflammation at the time of treatment. 5 If you have DME, it means diabetes has caused fluid to leak into the macula—drying that fluid is key to protecting sight. 6
Good candidates can attend follow-up visits, have OCT scans to check fluid, and understand that injections are usually ongoing. Your medical history, including recent strokes or heart attacks, and your comfort with eye injections will be reviewed so your plan is safe and realistic for you.
Enter your details below to check your suitability for this treatment
Suitability Level
Recommendation
Cost and Price
The total cost of care can include the drug, the injection procedure, imaging (like OCT), and clinic fees. Your out-of-pocket cost depends on your insurance plan and benefits. Retina practices follow safety and quality standards for intravitreal injections (sterile prep, numbing, post-injection checks), which are part of the service. 7 Vabysmo is supplied as a single-dose vial or prefilled syringe for a 6 mg intravitreal dose; your clinic’s pharmacy process follows the FDA label. 8
Ask your clinic about financial counseling. Many patients have some coverage through Medicare or commercial insurance. If you need help, your care team can explain prior authorization steps or patient assistance programs that may apply.
Benefits and Limitations
Benefits: In wet AMD, large clinical trials (TENAYA and LUCERNE) showed that faricimab was non-inferior to aflibercept for vision and allowed many patients to reach 12–16-week intervals. 9 In DME, YOSEMITE and RHINE also showed strong vision gains and durable control, with many eyes extending to every 16 weeks under protocol-guided dosing. 10
Limitations & risks: Vabysmo is not a cure; ongoing monitoring and repeat injections are usually needed. All eye injections carry small risks like infection (endophthalmitis), bleeding, inflammation, or a transient rise in eye pressure. Some eyes may need closer intervals or a different treatment if fluid persists or vision does not improve as expected. Your doctor will track your OCT and vision and adjust your plan to keep you safe and seeing your best.
Recovery and Long-Term Care
After an injection, mild scratchiness, tearing, or a small floater bubble is common for a day or two. Call urgently if you notice strong pain, worsening redness, many floaters, light sensitivity, or a sudden drop in vision—these can be warning signs that need same-day care. Patient guides from retina specialist groups explain the steps and red flags to watch for. 11 Your follow-up timing and future interval (often 8–16 weeks once stable) follow the FDA label and your personalized plan. 12
Long-term success comes from steady follow-up, healthy blood sugar and blood pressure control (for diabetes), and sticking with your schedule even when vision is doing well. Skipping visits can let fluid return and harm central vision. Your team will teach you how to self-monitor and when to call in between visits.
Latest Research & Innovations
Two-year data from the nAMD program support a treat-and-extend approach with faricimab, showing durable control with individualized intervals and maintained vision outcomes in many patients. 13 For macular edema after retinal vein occlusion, the BALATON and COMINO trials demonstrated that faricimab improved vision and anatomy and supported less frequent dosing after loading, expanding options for people with BRVO and CRVO. 14
Ongoing studies and real-world reports continue to refine who benefits most, how quickly intervals can extend, and how to combine imaging biomarkers with flexible dosing. Ask your specialist how the latest data fit your specific eye findings.
Recently Published in Peer-Reviewed Journals
BMC ophthalmology
July 31, 2025
Comparative efficacy of photodynamic therapy (PDT), ranibizumab, aflibercept monotherapy, and combination therapies for polypoidal choroidal vasculopathy: a network meta-analysis of randomized controlled trials.
Quiroz-Reyes MA, Quiroz-Gonzalez EA, Quiroz-Gonzalez MA, et al.
BMC ophthalmology
July 1, 2025
Real-world outcomes of a loading phase with intravitreal faricimab in refractory Neovascular Age-Related Macular Degeneration (nAMD) patients.
Yufeng X, Ningxi H, Mingzhi S, et al.
Ophthalmology science
April 10, 2025
Quantification of Hyperreflective Foci in Age-related Macular Degeneration by Polarization-Sensitive OCT.
Terao R, Aoki S, Kitamoto K, et al.
Next Steps
If your doctor suspects wet AMD, DME, or RVO-related swelling, early treatment helps protect central vision. The Mayo Clinic explains how wet AMD harms the macula and why quick care matters. 15 The right next step is an exam with a retina specialist (a fellowship-trained ophthalmologist focused on retina diseases). Learn what retina specialists do and how they care for people with macular conditions. 16
How Kerbside can help: We can connect you with the right type of specialist for a medical education consult about your options. This is for learning and planning only and does not create a physician-patient relationship. Bring your questions, your medication list, and your prior eye records if you have them.
Trusted Providers for Vabysmo

Dr. Emily Eton
Specialty
Retina/Vitreous
Education
Harvard Medical School

Dr. Grayson Armstrong
Specialty
Retina/Vitreous
Education
Ophthalmology

Dr. Jose Davila
Specialty
Retina/Vitreous
Education
Retina/Vitreous Surgery

Dr. Nicholas Carducci
Specialty
Retina/Vitreous
Education
University of Pennsylvania Perelman School of Medicine