Geographic Atrophy
also known as GA
Last updated August 21, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.


Overview
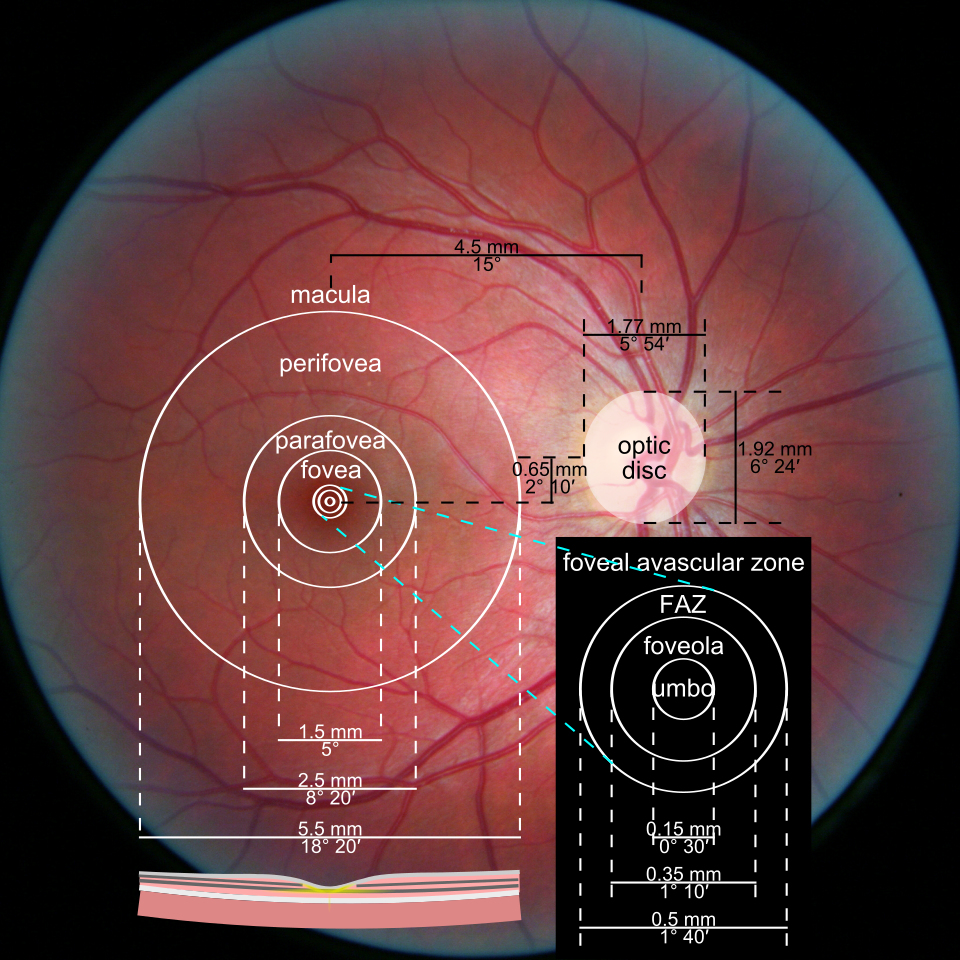
Geographic atrophy (GA) is an advanced stage of the “dry” form of age-related macular degeneration (AMD). It causes patches of retinal cells in the macula to wear away over time. The macula lets you see fine details, read, and recognize faces.
When GA grows toward the center of the macula, central vision gets worse. Side (peripheral) vision usually stays, so GA does not cause total blindness. GA tends to progress slowly, but it can still have a big impact on daily life.
Treatments are now available that can slow GA growth, though they cannot cure it or restore lost vision yet.
In 2023, the U.S. FDA approved the first medicines for GA after years of research into the eye’s “complement” immune pathway. These medicines are given by injection into the eye and are designed to slow how fast GA expands. 1 3
Symptoms
GA often starts with no symptoms. As areas of atrophy grow, you may notice:
- Blurry or dim central vision, especially when reading
- A gray or blank spot near the center of what you see
- Need for brighter light or more time to adapt when going from bright to dim places
- Colors looking less vivid
These symptoms usually happen in one eye first. Straight lines that look wavy or sudden vision changes can be a sign of wet AMD, which needs urgent care. 1 2
Causes and Risk Factors
GA is part of AMD and happens as the light-sensing cells and support tissue under the macula break down. The exact cause is complex. Age and genes play a role, and the body’s complement immune system can become overactive in the retina.
Key risks include:
- Age: Risk rises after age 55.
- Family history and genetics: Having a close relative with AMD raises risk.
- Smoking: Strongly linked to AMD.
- Other factors: High blood pressure and high cholesterol may add risk.
Healthy habits—like not smoking, staying active, and eating leafy greens and fish—may lower overall AMD risk. 1
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
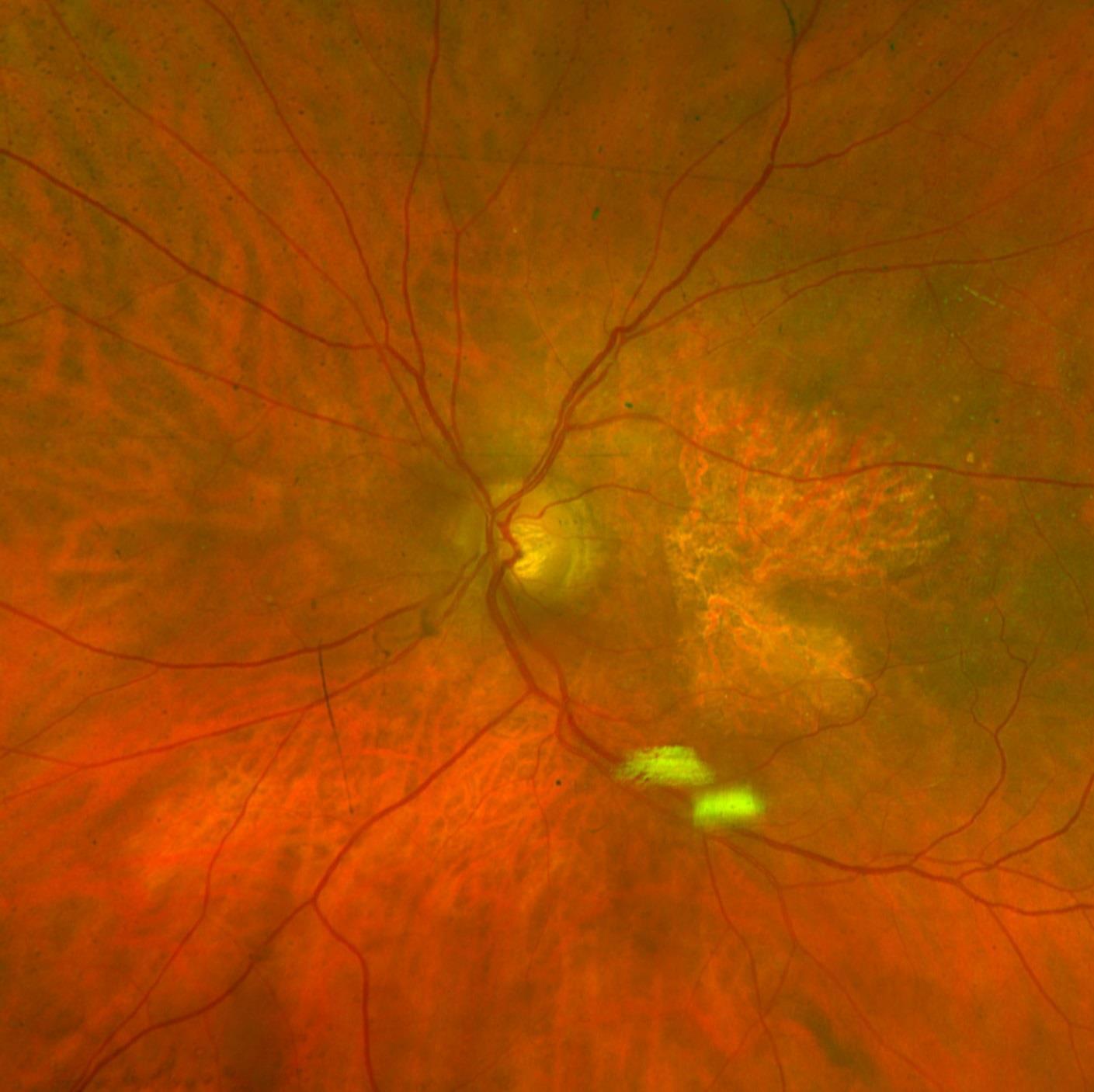
Eye doctors diagnose GA during a dilated eye exam and with imaging tests:
- Retinal photos: Show pale areas where tissue has thinned.
- Optical coherence tomography (OCT): Cross-section pictures of the retina help confirm atrophy and check for wet AMD.
- Fundus autofluorescence (FAF): Highlights stressed and atrophic retinal areas to track change over time.
These tests help your doctor measure lesion size, monitor growth, and plan treatment. 2
Treatment and Management
Two prescription medicines can slow GA growth. They do not reverse damage. Both are given by an eye specialist as injections in the clinic:
- Pegcetacoplan (SYFOVRE): A complement C3 inhibitor. Recommended dose: 15 mg (0.1 mL) injected every 25 to 60 days. Risks include discomfort, infection, and possible wet AMD.
- Avacincaptad pegol (IZERVAY): A complement C5 inhibitor with monthly dosing. Risks are similar, requiring close monitoring.
Other supportive measures:
Living with Geographic Atrophy and Prevention
Living with GA takes planning and support. Many people keep driving and working for years by making small changes. Consider:
- Use bright, even light and reduce glare at home.
- Try large-print books, audiobooks, or apps with zoom and voice.
- Ask your doctor about vision rehabilitation for training and devices.
- Protect your other eye: do not smoke, manage blood pressure, stay active, eat leafy greens and fish.
- Consider AREDS2 vitamins if appropriate for your AMD stage. 6
Latest Research & Developments
GA research is moving fast. Scientists discovered that over-active complement proteins can damage the retina in AMD. Targeting these proteins led to the first FDA-approved GA drugs in 2023.
Ongoing studies are testing:
- Longer-term outcomes
- Ways to predict who benefits most
- New approaches like gene and cell therapies
Your retina specialist will weigh benefits against risks and tailor dosing schedules. 3 8
Recently Published in Peer-Reviewed Journals
Investigative ophthalmology & visual science
August 1, 2025
Progression Patterns in Foveal-Sparing Geographic Atrophy With Double-Layer Sign Due to Neovascularization or Basal Laminar Deposits.
Fragiotta S, Parravano M, Sacconi R, et al.
Investigative ophthalmology & visual science
August 1, 2025
Evaluating the Progression of Retinal Sensitivity Loss in Geographic Atrophy Using Machine-Learning-Based Structure-Function Correlation (OMEGA 2).
Ansari G, Schärer N, Pfau K, et al.
Investigative ophthalmology & visual science
August 1, 2025
Dynamics of the EZ/RPE Loss Ratio on OCT Over Time During Geographic Atrophy Progression and Treatment With Pegcetacoplan.
Mai J, Reiter GS, Riedl S, et al.
Next Steps
If you notice vision changes, schedule a comprehensive, dilated eye exam. Ask about imaging (OCT, retinal photos) and whether GA is present.
Who to see: A retina specialist (ophthalmologist with retina training).
If appointments are full, ask for a cancellation list or nearby clinics.
Bring your glasses, medication list, and any home testing notes (e.g., Amsler grid).
You can also connect with a board-certified retina specialist on Kerbside for educational consults (not a patient–physician relationship).
For low-vision support, ask about vision rehabilitation resources. 6
Trusted Providers for Geographic Atrophy

Dr. Emily Eton
Specialty
Retina/Vitreous
Education
Harvard Medical School

Dr. Grayson Armstrong
Specialty
Retina/Vitreous
Education
Ophthalmology

Dr. Jose Davila
Specialty
Retina/Vitreous
Education
Retina/Vitreous Surgery

Dr. Nicholas Carducci
Specialty
Retina/Vitreous
Education
University of Pennsylvania Perelman School of Medicine