Macular Pucker
also known as Epiretinal Membrane
Last updated August 6, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.
Overview
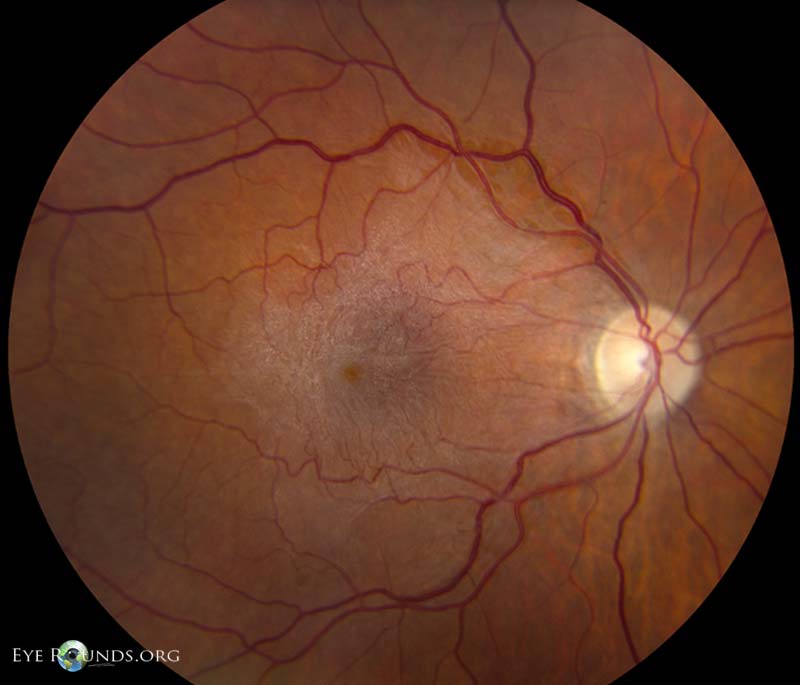
Macular pucker – also called an epiretinal membrane (ERM) – forms when a delicate sheet of scar tissue develops on the surface of the macula, the small retinal area that provides detailed central vision. As the membrane contracts it wrinkles, or “puckers,” the underlying retina, creating blurred or distorted sight that can make straight lines appear wavy and small print hard to read.1 The condition is common, affecting roughly 2 % of people over 50 and up to 20 % of those over 75 when mild, asymptomatic membranes are counted. Most cases remain stable and require only monitoring, but progressive puckers can compromise driving, reading, and independence unless surgically peeled.
Symptoms
The visual changes of an ERM develop slowly and may be noticed in only one eye at first because the brain suppresses the weaker image:
- Metamorphopsia – straight lines on a grid look bent or wavy.3
- Blurred or hazy central vision that glasses do not sharpen.
- Micropsia – objects appear smaller than they are.
- Difficulty reading fine print or seeing minute details on digital screens.4
- Rarely, double vision in one eye or a gray blind spot if the membrane is thick.
Peripheral or side vision is preserved, and there is no pain; sudden flashes, floaters, or a curtain over vision point instead to a retinal tear or detachment and need emergency care.
Causes and Risk Factors
An ERM forms when glial cells, retinal pigment epithelial cells, or inflammatory cells migrate onto the inner retinal surface after minor injury and secrete collagen. Triggers include:
- Posterior vitreous detachment (PVD), a normal aging change in which the gel inside the eye separates from the retina.5
- Retinal tears or detachment surgery and any previous laser or cryotherapy.
- Diabetic retinopathy, retinal vein occlusion or uveitis that disrupt the blood-retina barrier.6
- Ocular trauma – even years earlier.
- Age >60 and female sex (slight predominance).
Less often, membranes follow cataract surgery or radiation to the eye. They are not caused by reading in dim light, diet, or normal screen use.
Macular Pucker Progression Risk Score
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
A retina specialist confirms macular pucker with several painless tests:
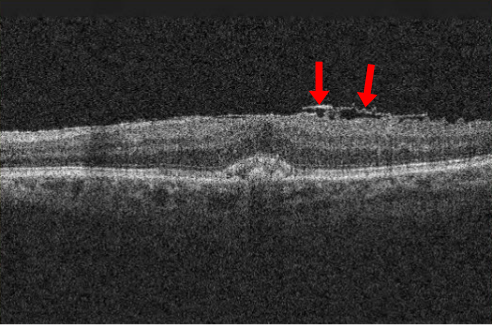
- Dilated fundus exam reveals a shiny, cellophane-like reflex or whitish preretinal sheet over the macula.7
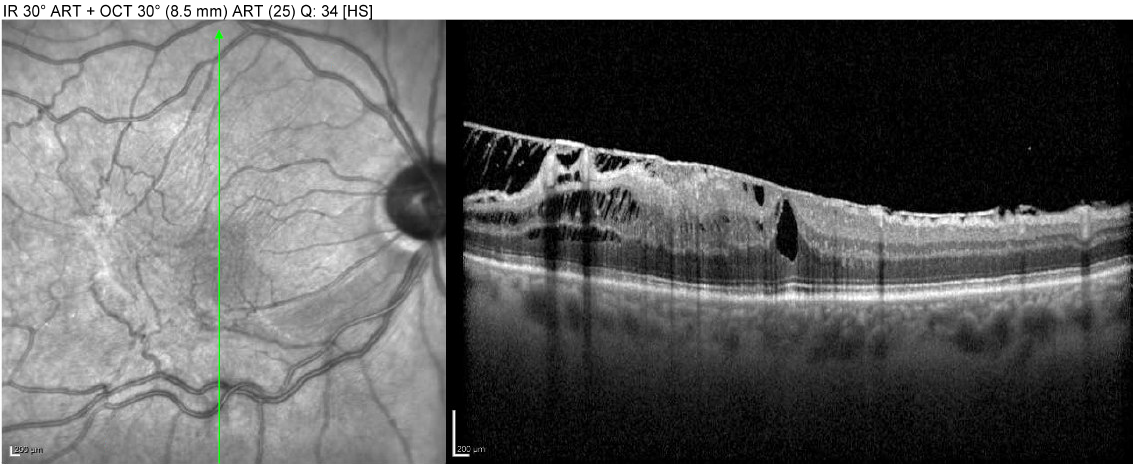
- Optical coherence tomography (OCT) provides high-resolution cross-sections showing a hyper-reflective membrane and wrinkled inner retina.8
- Amsler grid testing at home or in office documents metamorphopsia.
- Fluorescein angiography rules out macular edema from other retinal diseases when vision loss is pronounced.
Vision is measured with a standard Snellen chart; contrast sensitivity and reading speed tests help quantify functional impact when acuity seems only mildly reduced.
Treatment and Management
There is no medication or laser that dissolves an ERM. Management choices depend on symptom severity:
- Observation — up to 80 % of membranes stay stable or contract only slightly. Patients monitor at home with an Amsler grid and return every 6–12 months for OCT.9
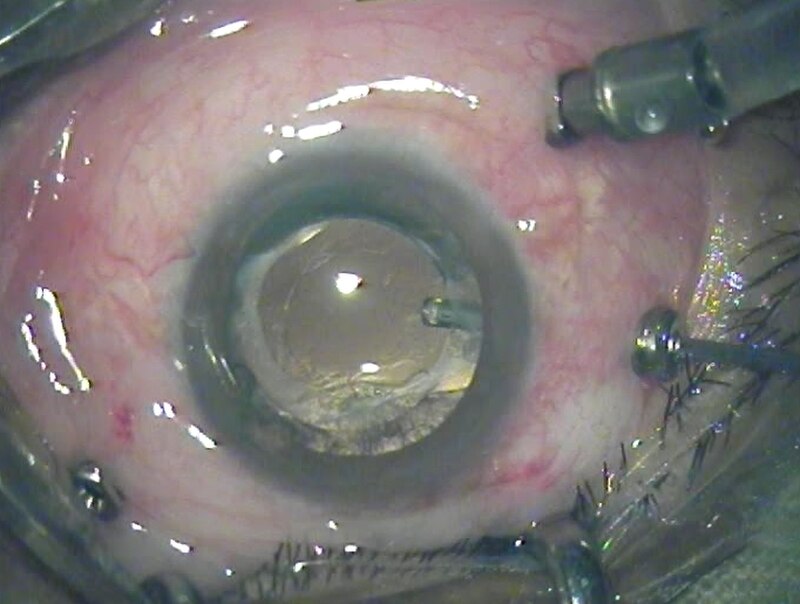
- Pars plana vitrectomy (PPV) with membrane peel — a microsurgical procedure that removes the vitreous gel, stains the ERM with a dye, and gently peels it off the macula. Visual acuity improves by two or more lines in about 70 % of eyes, and distortion lessens in most.10
- Combined cataract extraction is offered to phakic patients because cataract often accelerates after vitrectomy.
- Gas or oil tamponade is not usually required, and recovery seldom involves face-down positioning.
Risks of surgery include cataract progression, retinal tear or detachment (1-3 %), infection, and recurrence of membrane (5-10 %).
Living with Macular Pucker and Prevention
Everyday strategies can maximize vision and comfort:
- Optimize lighting during reading and hobbies; high-contrast LED lamps reduce strain.
- Use magnifiers, large-print books, or screen zoom settings to compensate for reduced acuity.
- Adjust monitor fonts and line spacing; dark mode often improves readability when contrast sensitivity falls.
- Maintain regular exercise and glucose control to limit vascular insults that can stimulate membrane formation.11
- Protect eyes from trauma with sports goggles and workplace safety glasses, as injury can initiate an ERM.
No proven diet or supplement prevents pucker, but a heart-healthy, antioxidant-rich diet supports overall retinal health. Routine eye exams after age 60 allow early detection before vision is noticeably affected.
Latest Research & Developments
Investigators are exploring less-invasive solutions:
- Enzymatic vitreolysis with ocriplasmin and newer collagenase blends aims to detach the vitreous and reduce membrane traction without surgery; early trials show modest success.12
- Ultra-high-resolution swept-source OCT can map individual retinal layers and predict visual recovery after peel more accurately than standard OCT.13
- Micro-incision 27-gauge vitrectomy tools shorten surgery time and speed healing compared with 23- or 25-gauge systems.
- Retinal prostaglandin inhibitors are under study to reduce post-operative cystoid macular edema, a leading cause of delayed visual gain.
- AI-driven OCT analytics may soon flag subclinical membranes in routine screenings.
Recently Published in Peer-Reviewed Journals
BMC ophthalmology
July 28, 2025
Endophthalmitis following inadvertent intravitreal injection of botulinum toxin: a case report and literature review.
Aljohani SM, Alharbi AS, Alhayaza RM
BMC ophthalmology
July 16, 2025
A case of nevoid basal cell carcinoma syndrome associated with optic nerve coloboma and epiretinal membrane.
Meng B, Cui M, Ji A
Retina (Philadelphia, Pa.)
July 10, 2025
Surgical outcomes of lamellar macular hole eyes with or without preservation of lamellar hole-associated epiretinal proliferation technique: a meta-analysis.
Yu Y, Wang YY, Tian M, et al.
Next Steps
If you notice new distortion, blurry central vision, or a decline in reading speed, arrange an evaluation with a vitreoretinal surgeon. They can confirm the diagnosis, explain OCT findings, and discuss whether observation or membrane peel best fits your goals.14 Consultation is urgent if vision drops two lines or more within six months, or if you develop flashes/floaters suggestive of a retinal tear.
How to schedule: Your optometrist or general ophthalmologist can refer you, but many retina clinics accept self-referrals. Kerbside can connect you to board-certified surgeons for virtual second opinions, individualized risk discussion, and convenient booking at high-volume surgical centers.
Trusted Providers for Macular Pucker

Dr. Emily Eton
Specialty
Retina/Vitreous
Education
Harvard Medical School

Dr. Grayson Armstrong
Specialty
Retina/Vitreous
Education
Ophthalmology

Dr. Jose Davila
Specialty
Retina/Vitreous
Education
Retina/Vitreous Surgery

Dr. Nicholas Carducci
Specialty
Retina/Vitreous
Education
University of Pennsylvania Perelman School of Medicine