Myopia
also known as Nearsightedness
Last updated July 28, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.


Overview
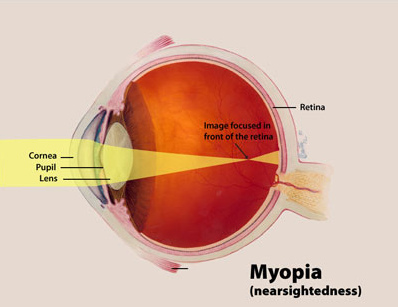
Myopia — often called nearsightedness — means distant objects look blurry because light focuses in front of, rather than directly on, the retina. More than 4 in 10 U.S. teens and young adults are affected, and modeling studies warn that half of the world’s population could be myopic by 2050, with nearly 1 billion facing sight-threatening high myopia complications.14 The American Academy of Ophthalmology (AAO) calls the trend a “global epidemic” because unchecked progression raises lifetime risks for retinal detachment, glaucoma and myopic maculopathy.5
Symptoms
Classic signs include:
- Blurred distance vision (difficulty reading the board or road signs)
- Squinting, eye strain or headaches after tasks requiring distance focus
- Sitting very close to TVs or holding books inches from the face
- Night-driving glare or haloes
Most children become symptomatic in early grade school; uncorrected myopia can impair learning and hand-eye coordination.2 Adults may notice progressive blur or frequent prescription changes, especially during prolonged digital work.3
Causes and Risk Factors
Myopia develops when the eye grows too long front-to-back or the cornea is too steep. Modern research shows both genes and environment matter:
- Having one myopic parent doubles risk; two parents triples it.
- Limited outdoor daylight and high “near-work” (screens, reading >3 h/day) accelerate axial elongation.7
- East Asian ancestry, urban living, and early age of onset (<8 years) are strong predictors of rapid progression.14
Systemic connective-tissue disorders or uncontrolled diabetes can also induce acquired myopia, though these cases are far less common.23
Myopia Risk Estimator
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
An eye-care professional will perform:
- Visual-acuity testing with a Snellen chart.
- Autorefraction and retinoscopy to estimate sphere, cylinder and axis.3
- Cycloplegic refraction after dilating drops — the Mayo Clinic notes this is crucial in kids to relax focusing muscles and reveal latent prescription.18
- Axial-length ultrasound or optical biometry to monitor progression.
Ancillary tests such as corneal topography help rule out keratoconus or measure suitability for refractive surgery.2
Treatment and Management
Optical Correction
Glasses or soft contact lenses provide instant clarity and are safe for all ages.2
Myopia-Control Strategies
- Toric and multifocal soft lenses designed for myopia control slowed progression by ~43% in a recent NEI-funded trial.8
- Orthokeratology (overnight corneal-molding RGP lenses) reshapes the cornea temporarily, giving clear daytime vision and 40–60 % control efficacy.9
- Low-dose atropine 0.05 % eye-drops reduce axial elongation up to 60 % with minimal side-effects, according to 3-year LAMP data and 2023 AAO reviews.1011
Refractive Surgery
Adults seeking freedom from lenses may choose LASIK, PRK or SMILE. Cole Eye Institute reports 94 % of post-LASIK eyes reach 20/20 vision at 3 months.12
Living with Myopia and Prevention
Daily habits can slow progression and protect eye health:
- Follow the 20-20-20 rule (look 20 ft away for 20 s every 20 min).
- Encourage ≥2 hours of outdoor play — each extra weekly hour outdoors cuts risk ~2 %.7
- Balance screen time with breaks and good lighting; AAO’s Myopia Control campaign offers printable tips for families.6
- Attend yearly dilated exams to detect retinal holes or myopic degeneration early.13
Community programs in Taiwan that added “two hours of sunshine” to the school day cut new-onset myopia by one-third, underscoring the power of prevention.17
Latest Research & Developments
- LAMP-5-Year Data: Extended follow-up confirms atropine 0.05 % maintains control benefits for five years with no serious adverse events.16
- DIMS & Stellest Spectacle Lenses: Novel defocus-incorporated optics show ~50 % efficacy and are now FDA-cleared.6
- Genetics & Environment: Global NEI collaborations are mapping gene–light interactions to design personalized prevention.1415
Recently Published in Peer-Reviewed Journals
JAMA ophthalmology
July 24, 2025
Interpreting Myopia Control Modalities in a 2-Year Trial.
Polling JR, Klaver CCW
The British journal of ophthalmology
July 24, 2025
Effect of daily disposable Defocus Incorporated Soft Contact lens on myopia control: a 1-year multicentre randomised controlled trial.
Liu L, Wang J, Tse DY, et al.
The British journal of ophthalmology
July 24, 2025
Advanced maternal reproductive age elevates myopia risk in offspring.
Qi J, Lin J, Zhang K, et al.
Next Steps
Best specialist to see: a pediatric ophthalmologist or cornea & refractive surgeon experienced in myopia control. Start with a comprehensive exam; if axial length is >26 mm or annual change exceeds 0.50 D, request referral to a dedicated myopia-management clinic such as Cleveland Clinic’s Cole Eye Institute or Mayo Clinic’s Pediatric Myopia Service.318
Kerbside can connect you directly with these subspecialists, streamline insurance pre-authorization, and coordinate follow-up scheduling — so you spend less time searching and more time seeing clearly.
