Photorefractive Keratectomy
also known as PRK
Last updated August 2, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.


Overview
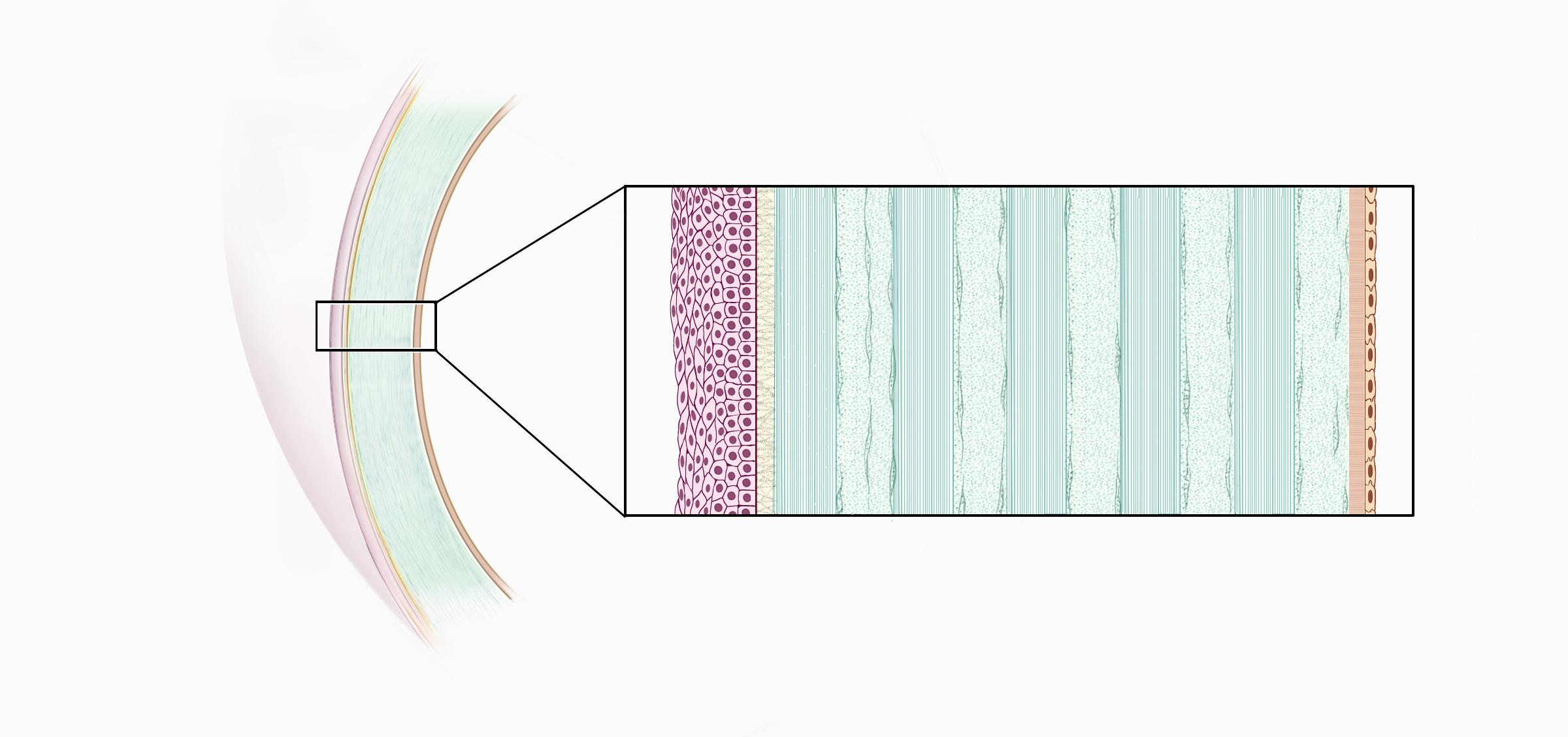
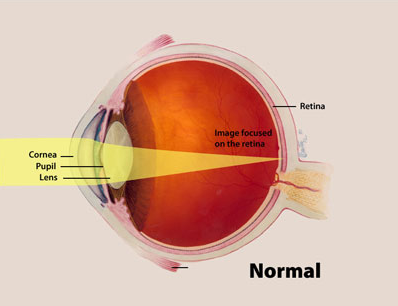
Photorefractive Keratectomy (PRK) was the first laser vision-correction procedure approved by the FDA. Instead of creating a corneal flap like LASIK, surgeons gently remove the paper-thin surface layer (epithelium) and use an excimer laser to reshape the underlying tissue. By changing the corneal curve, PRK corrects nearsightedness, farsightedness, and astigmatism so light focuses sharply on the retina. Over 90 % of treated eyes reach 20/40—or legal-driving—vision, and most achieve 20/20 once healing finishes.12
How the Procedure Works & Options
Under numbing drops, the epithelium is brushed off or dissolved with a dilute alcohol solution. Cool ultraviolet light from an excimer laser then removes microscopic layers of corneal tissue—about the thickness of a human hair—based on your exact prescription. A sponge with mitomycin-C may be applied for high corrections to prevent haze. Finally, a soft, clear bandage contact lens protects the eye while the epithelium grows back over three to five days.
PRK can be wavefront-guided to cut glare and topography-guided to treat irregular corneas. For thin corneas, PRK is often preferred over LASIK because no flap is created.34
Who Is a Candidate?
Good candidates are 18 + with a stable glasses or contact-lens prescription for a year, healthy eyes, and adequate corneal thickness. PRK is especially helpful when the cornea is too thin or irregular for a LASIK flap, or for military, law-enforcement, and contact-sport athletes who risk eye trauma. People with severe dry eye, keratoconus, uncontrolled diabetes, or autoimmune disease should avoid or delay surgery until those conditions are managed.56
PRK Suitability Score
Enter your details below to check your suitability for this treatment
Suitability Level
Recommendation
Benefits and Limitations
Benefits
• No corneal flap—so no risk of flap dislocation.
• Suitable for thinner or scarred corneas and some pilots or soldiers who cannot have LASIK.
• Vision remains stable long term; enhancement rates are low.
Limitations
• Healing is slower: functional vision returns in 3–7 days and may fluctuate for weeks.
• Mild to moderate pain, light sensitivity, and tearing are common the first 48 hours.
• Reading glasses are still needed later in life as presbyopia develops.
Large Mayo Clinic cohorts show 95 % satisfaction once the surface has healed, but realistic expectations—and patience during recovery—are key.78
Risks and Side Effects
The most common short-term effects are scratchy pain, light sensitivity, and hazy vision while the epithelium heals. Long-term complications are uncommon but may include:
- Corneal haze—usually mild and treatable with steroid drops
- Dry eye—managed with artificial tears or omega-3 supplements
- Infection or delayed healing—rare with proper drop use
Emerging research links certain tear-film proteins to lingering discomfort, which may someday help doctors predict who is prone to chronic pain after refractive surgery.910
Recovery and Long-Term Care
You’ll go home wearing dark glasses and rest the first day. Plan for:
- First week: bandage lens in place, antibiotic and steroid drops four times daily.
- Weeks 2-4: vision sharpens; resume driving, desk work, and light exercise.
- Months 1-3: final fine-tuning and possible enhancement check.
Avoid dusty environments, swimming pools, eye makeup, and contact sports until cleared. Most patients return to normal life after one week, with full visual stability by three months.1112
Latest Research & Innovations
New high-definition wavefront scanners tailor ablation patterns to each eye’s unique optical fingerprint, cutting night-time halos. Topography-guided PRK can treat irregular corneas after previous surgery or trauma. Studies also show that low-dose mitomycin-C and chilled irradiation reduce haze in high corrections.
AI-driven nomograms and tear-protein biomarkers are being explored to forecast healing speed and discomfort, aiming for truly personalized surface-ablation care.1314
Recently Published in Peer-Reviewed Journals
BMC ophthalmology
July 21, 2025
Effect of intraoperative mitomycin C application at different concentrations on corneal densitometry after SmartSurf(ACE) transepithelial photorefractive keratectomy.
Yu T, Yan C, Wang H, et al.
BMC ophthalmology
July 1, 2025
A comparative analysis of the 1-year outcomes of modified Athens protocol versus Cretan protocol in the treatment of progressive keratoconus.
Huang J, Wu J, Xiao W, et al.
BMC ophthalmology
May 7, 2025
A case report of implantable collamer lens removal with cataract extraction and TECNIS Symfony extended range of vision intraocular lens (ZXR00) implantation.
Yue P, Li E, Wang Z, et al.
Next Steps – See a Refractive Surgeon
If you’re interested in glasses-free vision but have been told your corneas are too thin for LASIK, schedule a consultation with a refractive surgeon. They’ll map your cornea, measure thickness, and explain how PRK, LASIK, or SMILE fit your goals. You can connect with the right specialist on Kerbside and take confident steps toward clearer sight.
Bring your latest glasses prescription and a list of medications so your surgeon can craft the safest plan.1516