Presbyopia
also known as Age-Related Farsightedness
Last updated July 29, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.


Overview
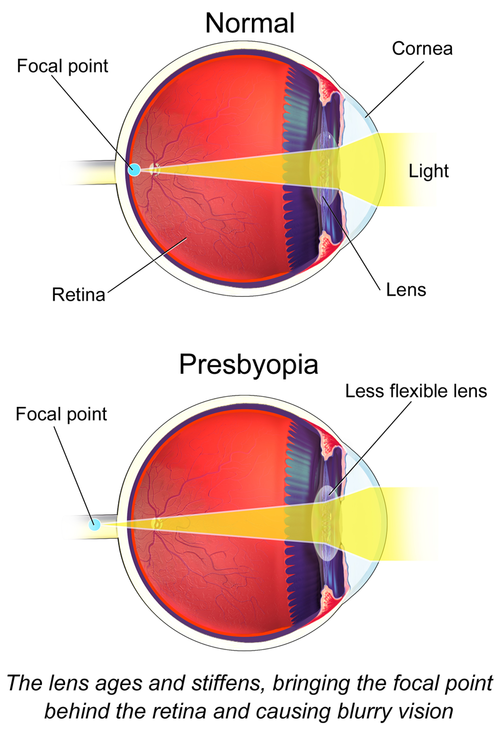
Presbyopia is an age-related refractive error in which the crystalline lens inside the eye gradually stiffens and can no longer change shape (accommodate) to focus on nearby objects. Most people first notice trouble with close work—such as reading a text message or threading a needle—sometime after age 40, and virtually everyone will be affected eventually.1 The change is a normal part of ocular aging rather than a disease, yet its impact on daily activities can be significant.2
Symptoms
Common signs include:
- Blurry near vision that improves when you hold material farther away.
- Eye strain or fatigue after prolonged reading.
- Headaches that start after close work.
Symptoms often progress slowly but predictably between the mid-40s and mid-60s.3 Many people notice they need brighter light to read small print, especially in dim restaurants or airplanes.4
Causes and Risk Factors
Presbyopia arises when lens proteins change and the lens capsule loses elasticity, reducing accommodative power. While aging is the primary driver, certain factors can accelerate onset:
- Uncorrected hyperopia (farsightedness).
- Systemic diseases such as diabetes or cardiovascular disease.
- Certain medications (antihistamines, diuretics, antidepressants).
- Extensive near-work or screen time.
- Low UV protection—sunlight may hasten oxidative changes within the lens.
Early presbyopia (before age 40) is uncommon but recognized.5 Healthy lifestyle habits—adequate lighting, balanced diet, and sunglasses—may modestly delay symptom severity.7
Presbyopia Symptom-Onset Risk Estimator
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
A comprehensive dilated eye exam with an optometrist or ophthalmologist confirms presbyopia. Testing usually includes:
- Refraction to measure distance and near prescriptions.
- Slit-lamp and retinal evaluation to rule out co-existing disease.
- Near-vision charts (+1.00 to +3.50 diopter range) to determine reading power.
The first baseline screening is recommended at age 40, followed by periodic exams tailored to personal risk.6 Regular check-ups also catch silent problems such as glaucoma or cataract.15
Treatment and Management
Treatments aim to compensate for lost accommodation rather than reverse aging changes.
Glasses & Contact Lenses
- Reading glasses (single-vision) are inexpensive and available over-the-counter in powers from +1.00 to +3.50 D.
- Bifocals, trifocals, or progressive lenses address both distance and near tasks in one pair.
- Multifocal or monovision contact lenses offer spectacle-free options.
Pharmacologic Therapy
Pilocarpine 1.25 % drops (brand name Vuity®) received U.S. FDA approval in 2021 for once-daily use, producing a temporary pupil constriction to increase depth of focus.9 Labeling notes headache and eye redness as the most common side effects.11
Surgical Options
- Refractive surgery (e.g., PresbyLASIK) reshapes the cornea to create multifocal zones.
- Corneal inlays use a small-aperture implant to expand depth of field (limited availability in the U.S.).
- Lens replacement with a multifocal or accommodating intraocular lens (IOL) can restore a range of focus, often combined with cataract surgery.6
Living with Presbyopia and Prevention
Simple adjustments keep close-up tasks comfortable:
- Use adequate, high-contrast lighting.
- Increase font size on digital devices.
- Take 20-second breaks every 20 minutes of near work.
- Wear sunglasses with 99–100 % UVA/UVB blocking when outdoors.
- Maintain systemic health—control blood sugar, blood pressure, and stop smoking.
Protecting eyes from ultraviolet light slows several age-related ocular changes.8 Public-health campaigns also emphasize regular exercise and a diet rich in leafy greens and omega-3 fats for overall eye wellness.14
Latest Research & Developments
Innovation is rapid in presbyopia care:
- Next-generation miotic drops and lens-softening agents are in phase 2–3 clinical trials, aiming for a longer-lasting effect than pilocarpine.10
- Accommodating and extended-depth-of-focus IOLs continue to evolve, with Bayesian meta-analysis showing significant gains in uncorrected near vision versus monofocal lenses.12
- Gene-based and electro-stimulative approaches to restore ciliary muscle function are under exploratory investigation; early feasibility data were presented in 2024.16
Recently Published in Peer-Reviewed Journals
The British journal of ophthalmology
July 7, 2025
Effectiveness of intraocular lenses designed to correct presbyopia after cataract surgery: an overview of systematic reviews.
Daka Q, Henein C, Fang CEH, et al.
BMC ophthalmology
May 19, 2025
Neurosensory binocular vision after bilateral implantation of an extended depth of focus intraocular lens with micro-monovision: a prospective cohort study.
Sun T, Zhao X, Liu Y, et al.
BMC ophthalmology
May 16, 2025
Assessing the clinical outcomes of a novel EDOF intraocular lens: a functional classification approach.
Győry JF, Németh G, Pesztenlehrer N
Next Steps
If you are struggling to read up close, schedule a comprehensive eye examination. The ideal provider is a board-certified ophthalmologist or optometrist experienced in refractive care. They can:
- Confirm the diagnosis and rule out other eye diseases.
- Discuss the full menu of nonsurgical and surgical options, tailoring them to your lifestyle.
- Create a follow-up plan, since your prescription typically changes every 2–3 years.
Waiting times for specialty clinics vary—some require primary-care or optometry referrals, while others allow self-booking. You can also connect directly with the right specialist on Kerbside to streamline the process.415
Trusted Providers for Presbyopia

Dr. Connie Wu
Specialty
Glaucoma
Education
The Warren Alpert Medical School of Brown University

Dr. Dane Slentz
Specialty
Oculoplastics
Education
Oculoplastics

Dr. Emily Eton
Specialty
Retina/Vitreous
Education
Harvard Medical School

Dr. Emily Schehlein
Specialty
Glaucoma
Education
Glaucoma

Dr. Grayson Armstrong
Specialty
Retina/Vitreous
Education
Ophthalmology

Dr. Jose Davila
Specialty
Retina/Vitreous
Education
Retina/Vitreous Surgery

Dr. Karen Chen
Specialty
Glaucoma
Education
Glaucoma

Dr. Levi Kanu
Specialty
Cornea and External Disease
Education
Cornea and External Disease

Dr. Nicholas Carducci
Specialty
Retina/Vitreous
Education
University of Pennsylvania Perelman School of Medicine