Hyperopia
also known as Farsightedness
Last updated July 28, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.
Overview
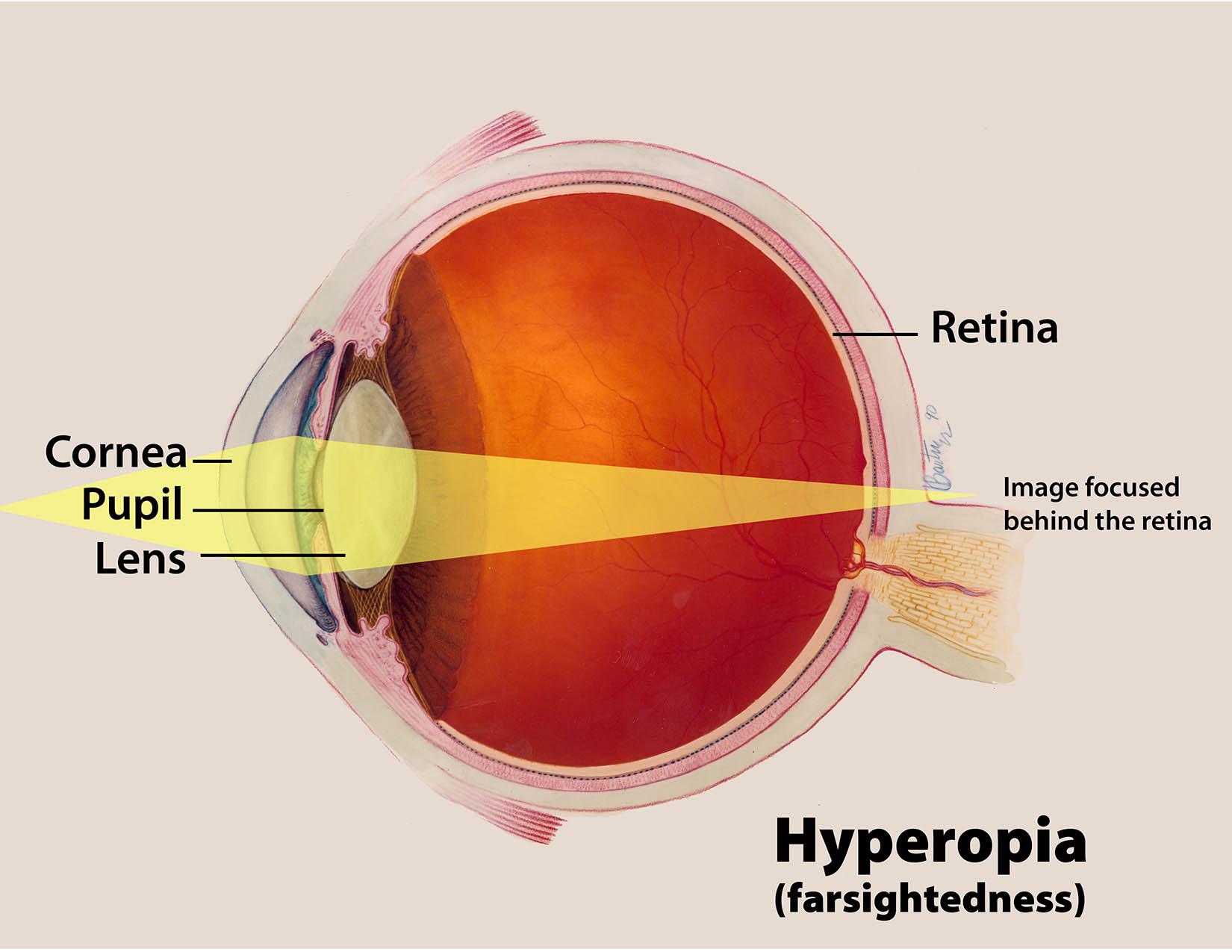
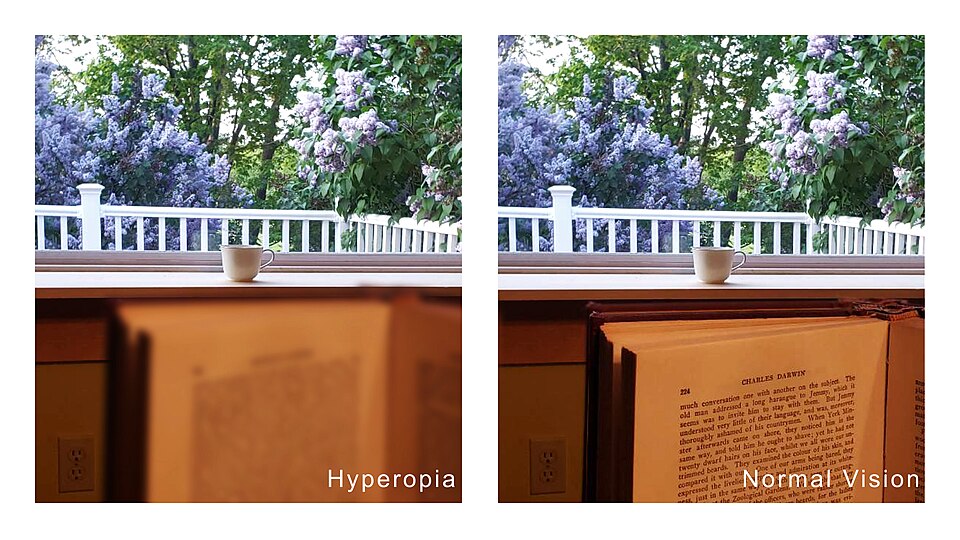
Hyperopia (farsightedness) means distant objects look clear, but anything up close is blurry because incoming light focuses behind the retina instead of on it.1 About 10–14 % of U.S. school-age children and roughly 10 % of adults still have clinically significant hyperopia—enough to affect reading comfort and, later, eye health.2 Uncorrected higher amounts raise the risk of amblyopia (lazy eye) or accommodative esotropia (crossed eyes) in kids, while adults may experience chronic eyestrain and headaches.3
Symptoms
Because the crystalline lens can compensate for small errors, mild hyperopia may go unnoticed. When demands rise—during close reading, computer use, or with age-related lens stiffening—people often report:
- Blurry vision at near or after prolonged reading
- Eye fatigue, burning, or tearing
- Frontal headaches after close work
- Difficulty maintaining attention on near tasks (children)
- Eye crossing in toddlers when they try to focus up close
Children rarely describe blur; instead they avoid near tasks or read slowly.3 A National Eye Institute (NEI) study found that moderate hyperopia in preschoolers was linked to lower early-literacy scores until properly corrected.4
Causes and Risk Factors
Hyperopia occurs when the eye’s optical power is too weak or its axial length too short. Key contributors include:
- Genetics: Having one farsighted parent nearly doubles risk; two parents triples it.3
- Premature birth & low birth weight: Incomplete ocular growth leaves the eye shorter than average and predisposes to hyperopia.5
- Maternal smoking or alcohol use during pregnancy
- Systemic conditions such as Down syndrome
- Age: After 40, the lens hardens (presbyopia), revealing latent hyperopia.2
Hyperopia Risk Estimator
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
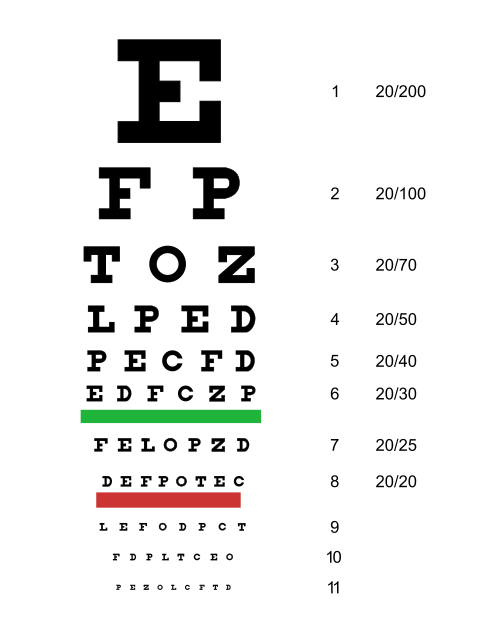
A comprehensive eye exam typically includes:
- Visual-acuity testing with a Snellen or LEA chart.
- Autorefraction or retinoscopy to estimate refractive error objectively.3
- Cycloplegic refraction after dilating drops—crucial in kids because it relaxes accommodation and reveals hidden hyperopia.6
- Cover testing to detect accommodative esotropia.
- Ocular-health check with slit-lamp and dilated retinal exam.
Treatment and Management
Eyeglasses
Plus-powered lenses move the focal point forward onto the retina and remain the safest, easiest treatment at any age.1
Contact Lenses
Soft or rigid gas-permeable lenses provide a wider field of clear vision and are popular in active teens and adults.
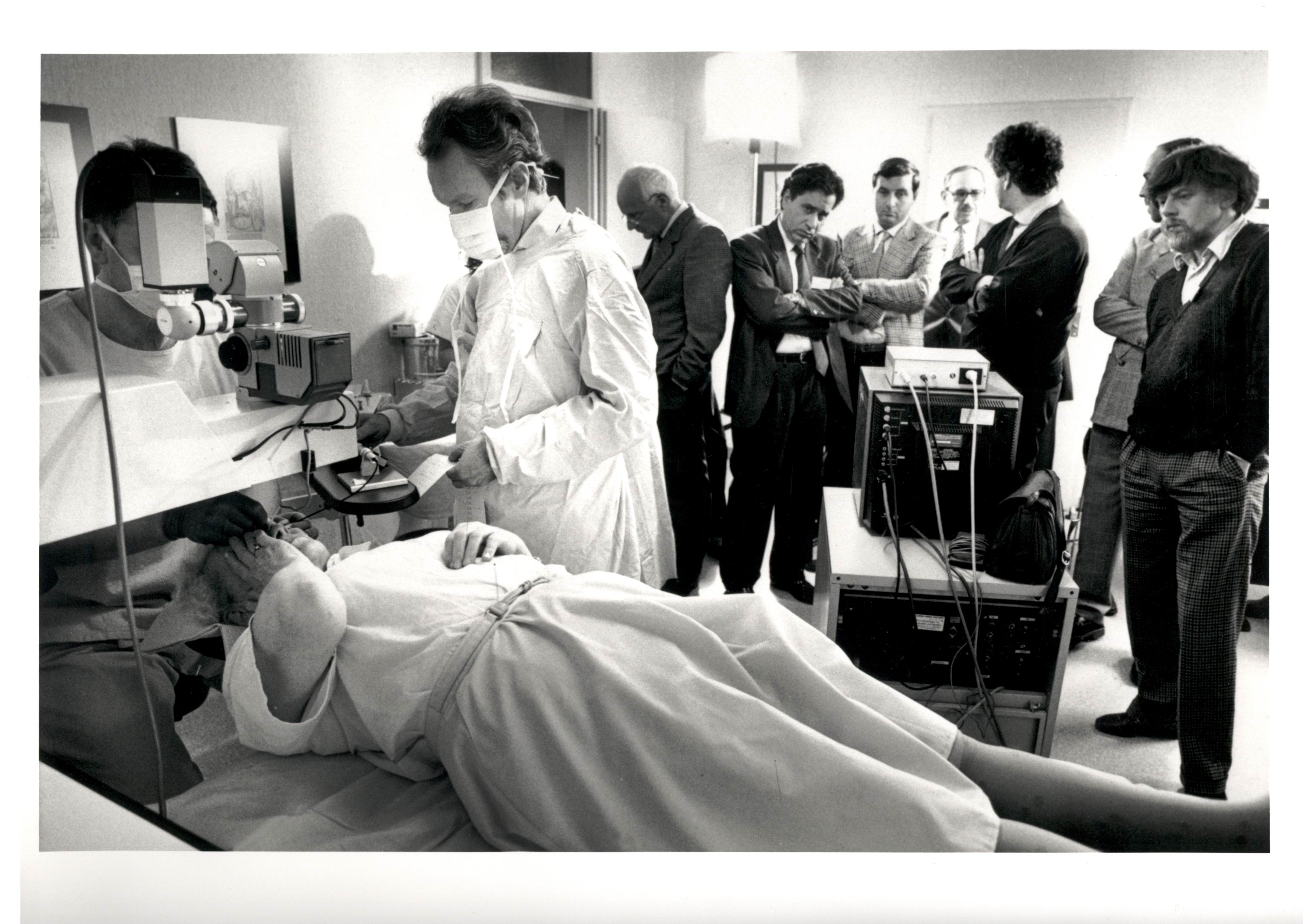
Refractive Surgery
LASIK and PRK can correct up to about +6 D; SMILE and phakic IOLs are under study for higher ranges.7 In a 2024 Cleveland Clinic outcomes series, 67 % of hyperopic LASIK eyes achieved 20/20 uncorrected vision within 3 months.8
Vision Therapy
Office-based exercises can improve accommodative stamina in children with focusing fatigue.
Living with Hyperopia and Prevention
You can’t always prevent hyperopia, but you can protect eye comfort and reduce complications by:
- Regular eye exams—infants at 6–12 months, children every 1–2 years, adults every 2 years (yearly after 40).
- Ergonomic reading habits: good lighting, 14–16-inch working distance, 20-20-20 break rule.
- Protective eyewear for sports or hazardous work.
- Healthy lifestyle: outdoor play, balanced diet, smoke-free environment.
The CDC stresses that early correction improves academic and socio-emotional outcomes.9 The Vision In Preschoolers–Hyperopia (VIP-HIP) study showed timely glasses halved amblyopia risk in preschoolers.4
Latest Research & Developments
- SMILE for hyperopia: A 2025 multicenter study reported 81 % of eyes within ±0.50 D at 12 months, matching LASIK accuracy with less dry-eye.11
- Next-generation accommodating IOLs: Spring 2024 updates highlight Juvene and FluidVision lenses entering pivotal FDA trials with promising 3-year visual-acuity data.12
- Genomics: GWAS meta-analyses have identified more than 30 loci linked to axial-length shortening and hyperopia risk, paving the way for personalized prediction tools.13
Recently Published in Peer-Reviewed Journals
BMC ophthalmology
July 22, 2025
Prevalence and patterns of subnormal visual acuity and refractive errors among preschool children in Sucheng district: a cross-sectional study.
Shen L, Cui Y, Zhao N, et al.
The British journal of ophthalmology
July 17, 2025
Prevalence and associations of spectacle adherence among school children in a multicentre Indian study.
Kuyyadiyil S, Jain E, Borah RR, et al.
BMC ophthalmology
July 9, 2025
Safety and efficacy of stromal lenticule addition keratoplasty in the treatment of hyperopia: a retrospective study.
Zhang J, Sun F, Hou J, et al.
Next Steps
Best specialist to see: a pediatric ophthalmologist (for children) or a cornea & refractive surgeon (for adults considering surgery). Begin with a comprehensive exam from an optometrist or general ophthalmologist; if hyperopia exceeds +4.00 D, eyes cross, or amblyopia is suspected, request prompt referral to a pediatric specialist. Adults with significant blur or presbyopia complaints may benefit from surgical consultation at tertiary centers such as Mayo Clinic or Cleveland Clinic.1415
You can streamline scheduling, insurance authorization, and post-visit follow-up by connecting directly with the right specialist through Kerbside.
