Amblyopia
also known as Lazy Eye
Last updated August 31, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.
Overview
Amblyopia, often called “lazy eye,” is when vision in one eye does not develop normally in early childhood because the brain favors the other eye. 1
This can happen even if the eye looks healthy and even when glasses are worn, because the problem is in how the brain and eye work together. Amblyopia is most often found in young children and is a leading cause of vision loss in kids, but treatment is very effective when started early. 3
Parents, teachers, and pediatricians play a key role by noticing signs and helping children get vision screening and a full eye exam if something seems off.
Symptoms
Symptoms can be subtle, which is why routine screening matters. Children may squint or close one eye, tilt their head, bump into things on the weak side, or struggle with small print. Some kids have poor depth perception and seem clumsy with balls, stairs, or pouring. 2
In many cases the stronger eye masks the problem, so a child may not complain about blurry vision.
Common clues:
- Squinting; an eye turning in or out; head tilt
- Sitting very close to screens or books
- Covering one eye to read
Less obvious signs:
- Short attention for visual tasks
- Avoiding puzzles or detailed crafts
- Frequent eye rubbing
If you notice these signs—or if a teacher or pediatrician flags a concern—ask for an eye exam with a pediatric-savvy eye doctor. Early checks can catch amblyopia before schoolwork and sports are affected. 3
Causes and Risk Factors
Amblyopia develops when clear, equal images do not reach the brain from both eyes during early “wiring” years. Main causes:
- Strabismic amblyopia: One eye is misaligned, so the brain suppresses its input to avoid double vision.
- Refractive (anisometropic) amblyopia: One eye has a stronger prescription (near/far/astigmatism), making its image blurrier and ignored.
- Deprivation amblyopia: Something blocks vision (e.g., congenital cataract, dense droopy eyelid/ptosis, corneal opacity).
Risk factors: Family history of amblyopia/strabismus, prematurity or low birth weight, and certain genetic or developmental conditions. 1
Because the brain’s visual pathways are most flexible in early childhood, the sooner issues are found and treated, the better the chance for normal vision. 2
Amblyopia Risk Assessment Calculator
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
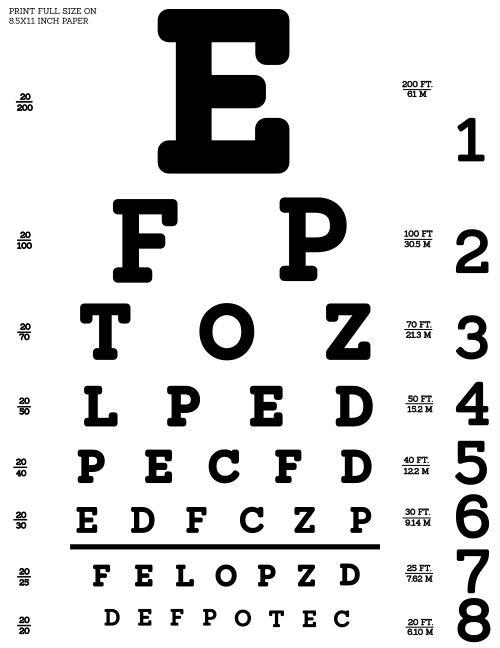
Diagnosis starts with a comprehensive eye exam. The doctor will check visual acuity with age-appropriate charts or matching tests, measure refraction to find the glasses prescription, and perform a cover test to look for misalignment. The front and back of the eye are examined to rule out cataract or other causes that block vision. 2
For prevention, the U.S. Preventive Services Task Force recommends vision screening at least once for all children ages 3–5 years to detect amblyopia or its risk factors, with earlier referral if concerns arise. 4
Treatment and Management
Treatment aims to deliver a clear image from the weaker eye and encourage the brain to use it. Plans are tailored to age, cause, and severity, and evolve as vision improves.
- Correct the optics: Many children improve simply by wearing the right glasses full-time—especially when unequal prescriptions are the cause. 6
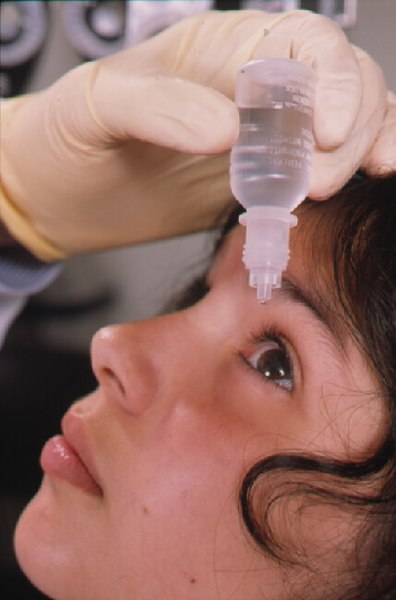
- Encourage use of the weaker eye: Two proven options are patching the stronger eye for set hours per day or using atropine drops in the stronger eye to blur it for near tasks. The Amblyopia Treatment Studies found that, in moderate amblyopia, daily atropine works about as well as patching, and weekend atropine can match daily in some cases.
- Treat the cause: If cataract, significant ptosis, or another blockage is present, surgery or procedures may be needed, often followed by glasses and patching or drops.
- Support & follow-up: Consistency matters. Set routines (patch during reading/crafts) and use reward charts. Regular visits allow adjusting hours, tapering safely to avoid relapse, and switching strategies if progress stalls. 5
Living with Amblyopia and Prevention
With a clear plan and family support, most children gain meaningful vision in the weaker eye. Practical tips:
- Make it a habit: Keep glasses on all waking hours; place patches or give drops at the same time daily and pair with fun near tasks.
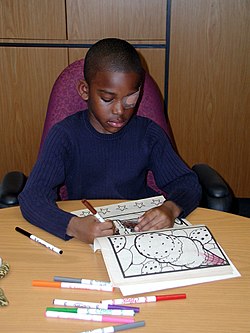
- Break it up: Split patching into shorter blocks while doing near work (reading, coloring, building).
- Protect both eyes: Use polycarbonate lenses for sports/outdoor play; hats and sunglasses outside.
- School partnership: Share the plan with teachers so patching can continue during quiet classroom activities.
- Stick with follow-ups: Vision can slip if treatment stops too early; your doctor will guide a safe taper and long-term monitoring.
Good adherence and steady follow-up are strong predictors of success; most kids treated early reach vision that supports school, sports, and later driving. 3 If new eye turning, headaches, or reading struggles appear, schedule a recheck to adjust the plan. 2
Latest Research & Developments
Research continues to refine amblyopia care and explore help for older patients. A Cochrane review pooling several trials found similar vision gains with patching and atropine in many children, giving families more than one effective option. 7
Newer binocular approaches (dichoptic training using games or specialized displays) aim to retrain both eyes to work together; early studies in adults show improvements in contrast sensitivity and other visual skills, though methods are still evolving. 8
Recently Published in Peer-Reviewed Journals
The British journal of ophthalmology
July 3, 2025
Current status of school vision screening-rationale, models, impact and challenges: a review.
Little JA, Chan VF, Saw SM, et al.
Investigative ophthalmology & visual science
July 1, 2025
Axial Length Dynamics and Safety of Occlusion Therapy in Pediatric Amblyopia: A Longitudinal Analysis.
Yu W, He Y, Qiu X, et al.
Investigative ophthalmology & visual science
July 1, 2025
Dichoptic Visual Search at Varied Fellow Eye Contrasts and Visual Function Deficits in Amblyopia.
Shi S, Quagraine IM, Cakir GB, et al.
Next Steps – See a Pediatric Ophthalmologist Early
If you suspect amblyopia, schedule an evaluation with a pediatric ophthalmologist or an optometrist experienced with children. Tell the scheduler you’re concerned about “possible amblyopia,” and ask about cancellation lists if the next routine slot is far out. Bring your child’s glasses and any school or screening results. 2
Early treatment offers the best chance to build strong, lasting vision, and you can also connect on Kerbside for a medical education consult with the right specialist (no patient–physician relationship is established). 1