Minimally Invasive Glaucoma Surgery
also known as MIGS
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.


Overview
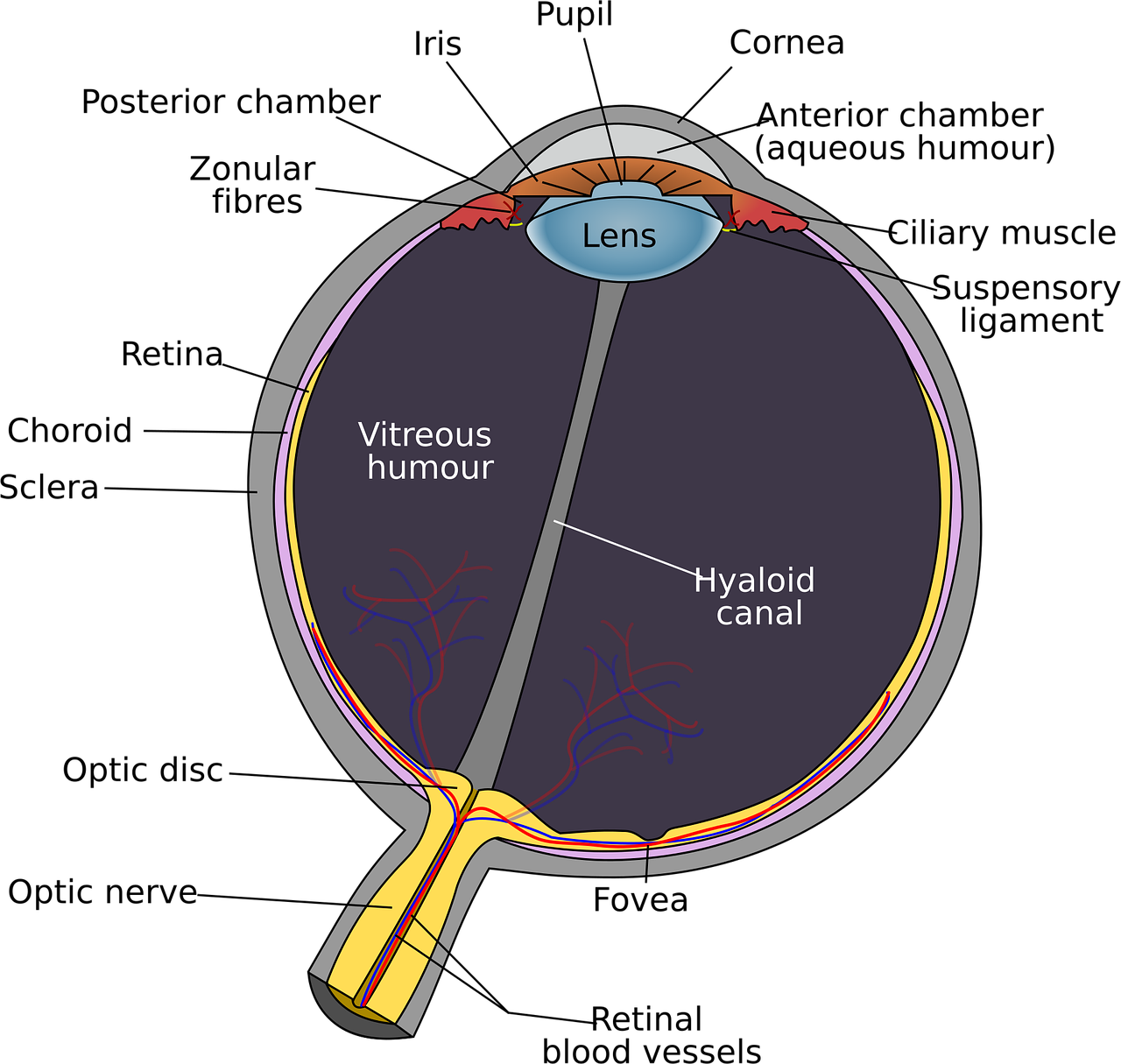
Minimally Invasive Glaucoma Surgery, or MIGS, is a group of small-incision procedures that lower eye pressure (intra-ocular pressure or IOP) with far less tissue disruption than traditional glaucoma operations. Because MIGS is gentler on the eye, healing is faster and the risks are lower, making it a helpful option for many people with mild-to-moderate glaucoma.
The goal is the same as with any glaucoma treatment — protect the optic nerve by improving the eye’s natural fluid drainage or by inserting a tiny stent that creates a new pathway. MIGS can be performed alone or at the same time as cataract surgery.
Doctors may recommend MIGS when eyedrops or laser treatment are not enough, or when medication side effects and costs become burdensome.12
How the Procedure Works & Options
MIGS procedures are done through a 1–2 mm clear-corneal entry using special microscopes and tiny instruments. Surgeons either:
- Bypass the trabecular meshwork with a micro-stent (e.g., iStent inject, Hydrus, XEN Gel Stent).
- Remove or excise a strip of trabecular tissue (e.g., Kahook Dual Blade, GATT).
- Dilate Schlemm’s canal with visco-surgical catheters.
- Shunt fluid to the subconjunctival or suprachoroidal space.
Most MIGS take 5-15 minutes and are often combined with phacoemulsification for cataract. A drop of local anesthetic and mild IV sedation keep you comfortable throughout.34
Who Is a Candidate?
You may benefit from MIGS if you have:
- Primary open-angle or certain secondary glaucomas in the mild-to-moderate stage.
- IOP that is not at target despite one or more medications.
- Difficulty affording, tolerating, or remembering drops.
- An open anterior chamber angle and no active inflammation.
- A need or desire to combine treatment with cataract surgery.
MIGS is usually not enough for eyes with very advanced optic-nerve damage that require very low IOP targets; in those cases traditional filtering surgery may still be necessary.56
MIGS Suitability Score
Enter your details below to check your suitability for this treatment
Suitability Level
Recommendation
Benefits and Limitations
Benefits
- Lower complication rate than trabeculectomy or tube shunts.
- Quicker vision recovery — many people resume normal activities within a week.
- May reduce or eliminate daily glaucoma drops.
- Can be performed through the same micro-incision as cataract surgery.
Limitations
- IOP reduction is modest (often 20–40 %).
- Results may wane over time, sometimes requiring repeat treatment.
- Not ideal for eyes needing very low single-digit pressures.
Understanding both the upside and the trade-offs helps patients choose wisely.78
Risks and Side Effects
Although safer than traditional surgery, MIGS still carries some risks:
- Temporary blurred vision, light sensitivity, or redness.
- Mild bleeding in the eye (hyphema) that usually clears on its own.
- Transient IOP spikes or, rarely, pressure that is too low.
- Device mal-position or blockage that may need revision.
- Infection and severe vision loss are very uncommon.
Your surgeon will review precautions to minimize these risks and will check the eye at 1 day, 1 week, and 1 month after surgery.910
Recovery and Long-Term Care
Most people return home the same day. Expect:
- Prescription anti-inflammatory and antibiotic drops for 2–4 weeks.
- Activity limits (no heavy lifting, swimming, or eye rubbing) for about a week.
- A mild scratchy sensation that fades as the eye heals.
Long term, you will still need routine glaucoma check-ups. Some patients stay off drops for years; others may need medication again if pressure creeps up. A healthy lifestyle, good medication adherence, and regular optic-nerve monitoring remain key.1112
Latest Research & Innovations
Newer devices such as the Hydrus Microstent and XEN Gel Stent are showing encouraging multi-year results in lowering IOP and medication burden. Researchers are also exploring drug-eluting stents and adjustable implants that can be fine-tuned after surgery.
A 2024 case series reported sustained pressure control with circumferential trabeculotomy using an illuminated micro-catheter, even after other angle surgeries had failed.1314
Recently Published in Peer-Reviewed Journals
Ophthalmology. Glaucoma
July 31, 2025
Glaucoma Surgery: From the Tried and True to the Novel and New.
Gedde SJ, Herndon LW Jr
Ophthalmology. Glaucoma
July 26, 2025
Selective Laser Trabeculoplasty and the Evolving Glaucoma Paradigm.
Realini T, Gazzard G
BMC ophthalmology
July 24, 2025
Serous retinal detachment with retinal pigment epithelium tear after PreserFlo MicroShunt surgery: a case report.
Sadahide A, Harada Y, Sakaguchi H, et al.
Next Steps – See a Glaucoma Specialist
If you think MIGS might be right for you, schedule a comprehensive evaluation with a glaucoma specialist. They will measure your eye pressure, examine the drainage angle, and discuss all treatment options. You can connect with the right specialist quickly on Kerbside.
Bring a current list of medications, past eye records, and any questions you have about recovery, cost, and long-term expectations.1516


