Hydrus Microstent
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms for details.

Overview
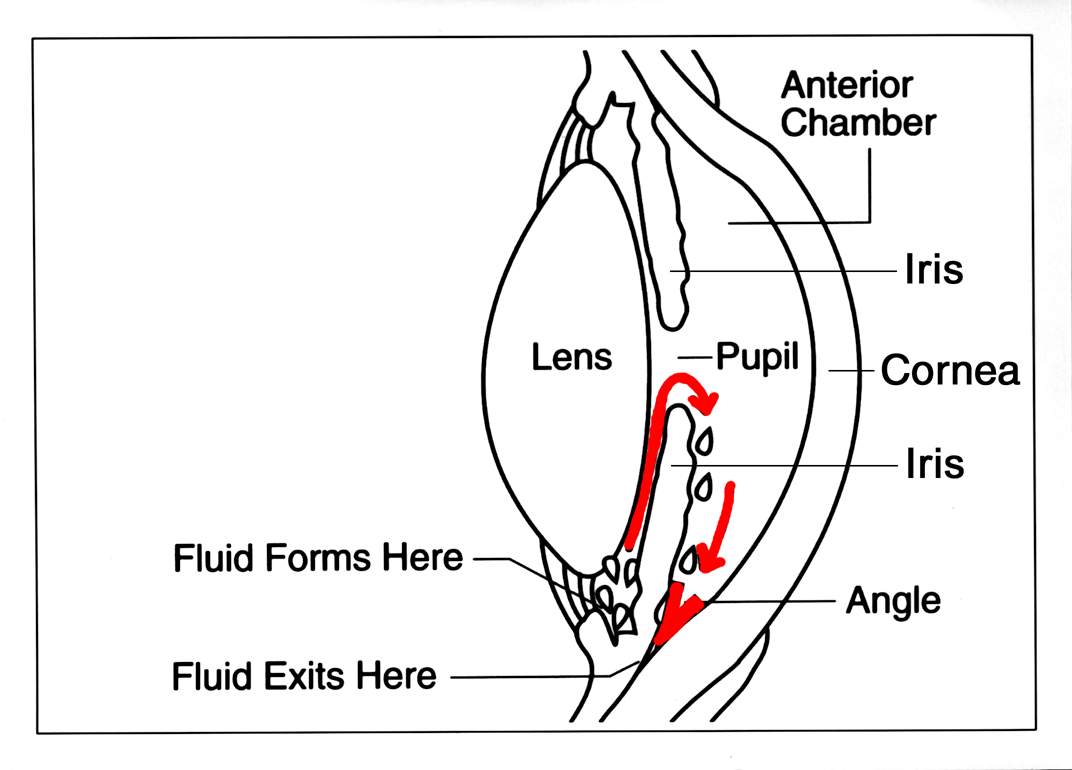
The Hydrus Microstent is a tiny curved implant used during cataract surgery to help lower eye pressure (intraocular pressure, or IOP) in adults with mild to moderate primary open-angle glaucoma (POAG). It belongs to a group of procedures called microinvasive glaucoma surgery (MIGS), which aim to control pressure with small openings and a quicker recovery than traditional glaucoma surgeries.1
The device sits inside Schlemm’s canal (the eye’s natural drain) to gently prop it open across about 90 degrees, creating a wider pathway for aqueous humor to exit and helping protect the optic nerve long term.2
Hydrus is placed at the same time as cataract surgery and is not a stand-alone procedure in the U.S. The goal is to reduce IOP and, when possible, decrease the number of daily glaucoma drops after surgery. Your surgeon will evaluate your glaucoma stage, target pressure, and angle anatomy before recommending it.
How the Procedure Works & Options
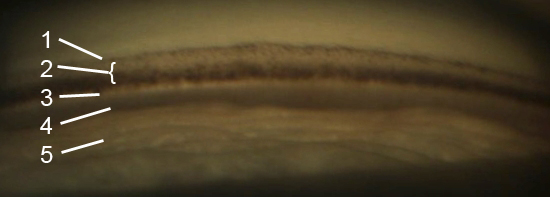
How it works: During cataract surgery, the cloudy lens is removed and a clear lens implant is placed. Using a special angle-viewing lens (gonioprism), the surgeon advances the Hydrus through the trabecular meshwork and into Schlemm’s canal, where it acts as a micro-scaffold to improve outflow through the eye’s natural drainage system.3
The implant’s design allows it to expand the canal over about one quarter of its circumference, improving access to multiple collector channels that drain fluid from the eye.4
Where it fits among options: POAG care is personalized. Options include:
- Drops
- Laser trabeculoplasty
- Canal-based MIGS (like Hydrus)
- Other MIGS under the conjunctiva
- More invasive surgeries such as trabeculectomy or tube shunts
Your ophthalmologist will match treatments to your disease stage, target IOP, and medication tolerance.
Who Is a Candidate?
Good candidates: Adults with mild to moderate POAG scheduled for cataract surgery and an open drainage angle on gonioscopy so the surgeon can safely access the trabecular meshwork.5 The decision also considers medication burden, pressure history, optic nerve health, and your agreed-upon target IOP.6
Not suited: Those with angle-closure glaucoma, active eye inflammation, secondary causes listed in labeling, or poor angle visibility (e.g., corneal opacity). Your surgeon will review your medical history and exam findings to confirm candidacy.
Is Hydrus Microstent a Good Fit for Me?
Select your details to estimate suitability.
Cost and Price
Because Hydrus is implanted during cataract surgery, costs include the cataract operation plus MIGS device placement. In the U.S., medically necessary outpatient eye surgery is usually covered under Medicare Part B and many commercial plans, but you may owe a deductible and coinsurance.7 Exact out-of-pocket costs depend on your plan and network status. If performed in a hospital outpatient department, outpatient hospital service rules apply; ask the facility to estimate copays and fees.8
Tip: Bring insurance cards and a medication list to your pre-op visit. The office can check benefits and prior authorization needs.
Benefits and Limitations
Benefits: In the randomized HORIZON trial, Hydrus plus cataract surgery produced sustained IOP lowering and reduced the need for glaucoma medications versus cataract surgery alone.9 By scaffolding Schlemm’s canal and bypassing the trabecular meshwork, the device enhances natural outflow, offering pressure control with a favorable safety profile compared with more invasive surgery in selected patients.10
Limitations & Risks: Results vary. Some still need drops or later procedures. Reported risks: bleeding, inflammation, device malposition or obstruction, peripheral anterior synechiae (PAS), and rare additional surgery. Your surgeon will explain risks for your eye.
Recovery and Long-Term Care
Recovery generally follows cataract-surgery steps: use prescribed drops, avoid eye rubbing, wear a shield as instructed, and attend follow-ups. Benchmarks suggest an exam on day 1, 1–2 weeks, and further visits to monitor vision, IOP, and anterior segment.11
After Hydrus, clinicians check the implant with gonioscopy for inlet patency and ensure no cornea or iris touch, while tracking pressure and drops.12
Urgent signs: severe pain, sudden vision drop, increasing redness, or many new floaters—seek care promptly.
Latest Research & Innovations
Long-term outcomes: The HORIZON trial’s multi-year data showed Hydrus with cataract surgery sustained pressure reduction and reduced later incisional surgery need versus cataract surgery alone.13 Additional analyses report slower visual-field loss over five years in Hydrus patients.14
Ongoing research explores surgeon techniques, patient selection, and Hydrus comparisons with other MIGS in real-world settings.
Recent Peer-Reviewed Research
Outcomes of Hydrus Microstent with Cataract Surgery in Asian and Non-Asian Eyes with Normal Tension Glaucoma.
Kuo DS, Lee SYH, Theophanous CN
Cost-Effectiveness Analysis of Hydrus Microstent for Patients with Mild to Moderate Primary Open-Angle Glaucoma in Canada.
Ahmed IIK, Hussein I, Saheb H, et al.
Phacoemulsification combined with trabecular meshwork-Schlemm canal-based minimally invasive glaucoma surgery in primary angle-closure glaucoma: a systematic review and meta-analysis.
Fang Z, Song Y, Jin L, et al.
Next Steps
If you have a visually significant cataract and mild to moderate POAG, talk with a board-certified ophthalmologist (ideally a glaucoma specialist) about Hydrus during cataract surgery to reach target IOP with fewer drops. Use the AAO directory to find an eye M.D.15
Seek urgent care for sudden eye pain, halos, headache, nausea, or big vision changes—possible signs of acute pressure rise.16 Kerbside can help you connect with the right specialist for education-focused consults (not a physician–patient relationship).