Trabeculectomy
also known as Trab
Last updated August 30, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.
Overview
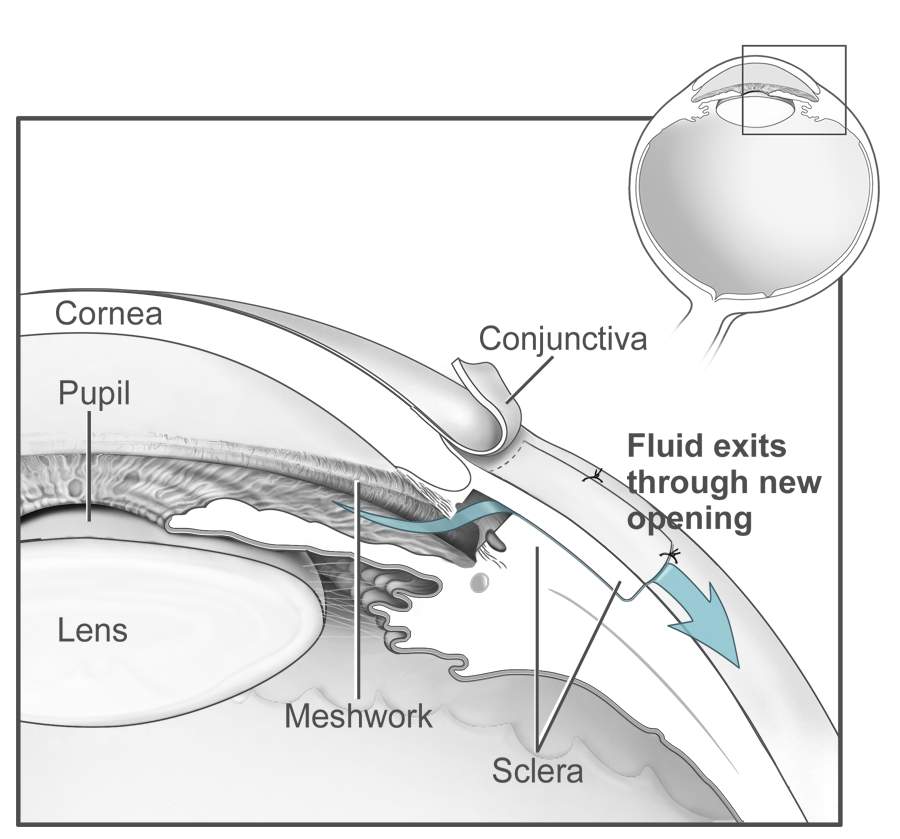
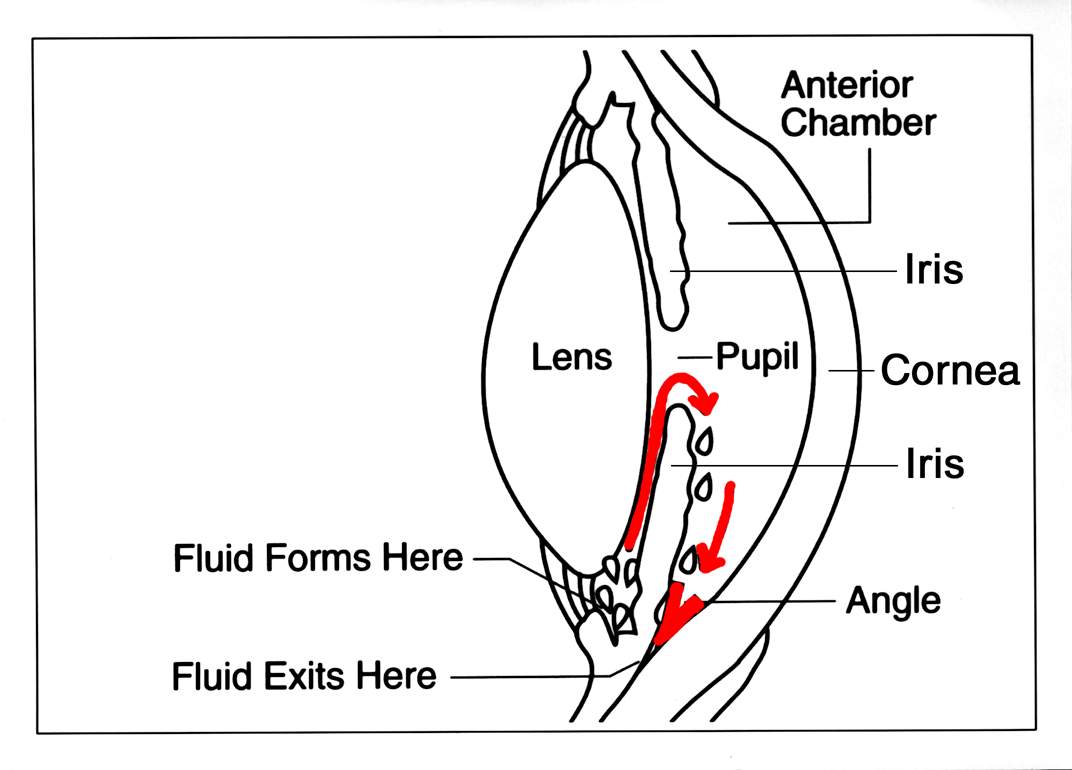
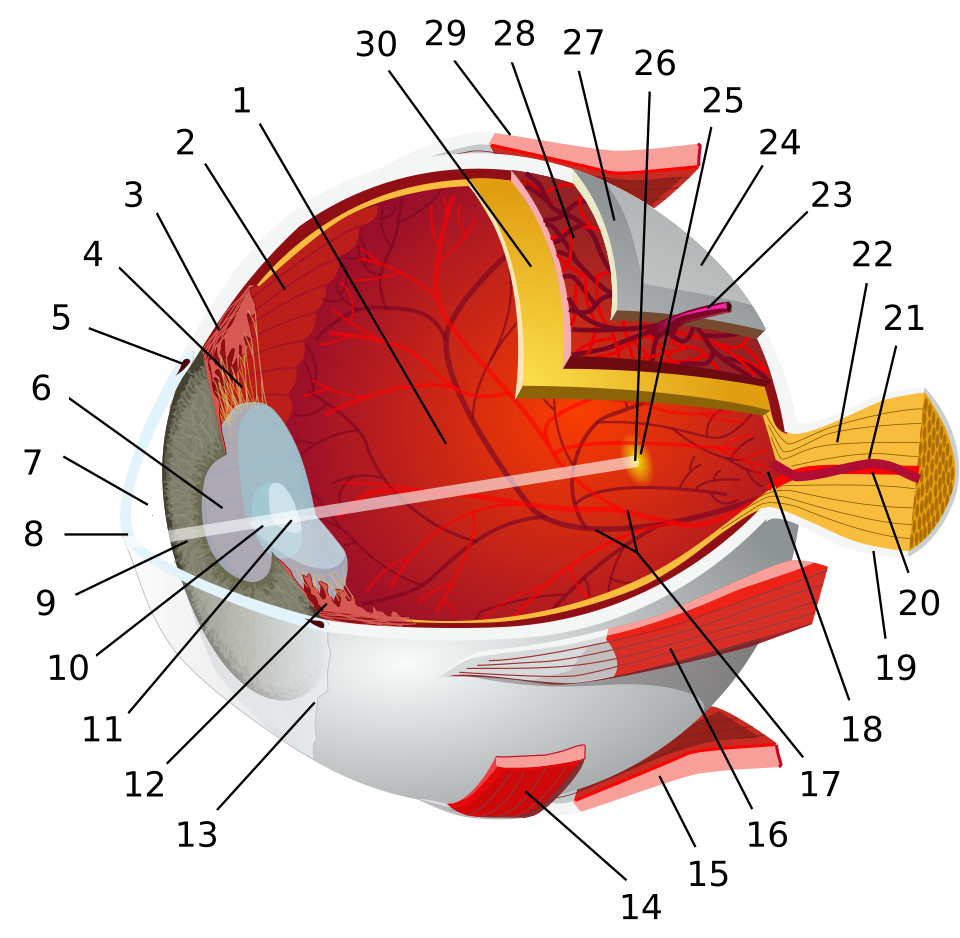
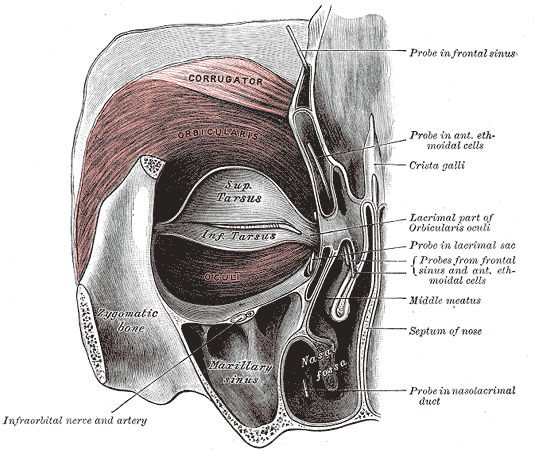
Trabeculectomy is a time-tested glaucoma surgery that creates a new drainage pathway so fluid can leave the eye more easily. By lowering eye pressure (intraocular pressure, or IOP), the surgery helps protect the optic nerve and slow vision loss. 1 In simple terms, the surgeon makes a tiny controlled flap and opening in the white part of the eye so fluid can filter into a small pocket (a "bleb") hidden under the upper eyelid, where it is absorbed by surrounding tissues. 2
Doctors consider trabeculectomy when eye drops and laser are no longer enough, or when very low target pressures are needed to protect vision. It can help many types of glaucoma, including primary open-angle glaucoma and some angle-closure eyes after the angle has been opened. The procedure has been refined over decades, with modern techniques focused on safety, customization, and careful follow-up to keep the bleb healthy and the pressure steady.
How the Procedure Works & Options
Step-by-step, in plain language: After numbing the eye, the surgeon creates a thin scleral flap (like a hinged door), then removes a tiny piece of tissue at the natural drain to let fluid exit. The flap is closed with small sutures so the outflow is slow and controlled, and a clear membrane (conjunctiva) is closed over it to form the hidden bleb. This controlled outflow lowers IOP without a permanent tube or valve. 3 Because healing can scar the new pathway, surgeons may apply anti-scarring medicines (like mitomycin-C or 5-fluorouracil) during or after surgery to keep the bleb working. 4
Customization options: Sutures can be tied to allow later adjustment (releasable stitches) or opened with a gentle in-office laser (laser suture lysis) if more flow is needed after surgery. Surgeons also tailor flap size, placement, and medicine strength to each eye’s risks. The goal is a steady pressure in the safe range with the fewest drops.
Who Is a Candidate?
Often a good fit:
- People with glaucoma whose IOP remains too high, who are losing vision despite medicines and/or laser, or who need very low target pressures that other options may not reach. 5
- Those able to return for early follow-ups and adjustments.
- Eyes where a realistic pressure goal has been set with the care team. 6
Who may need a different plan: Eyes with active infection or severe surface disease may need to heal first. People who cannot return for early visits may be steered to options that require less immediate adjustment. Surgeons will also consider other eye problems (e.g., cataract) and may time surgery to address both efficiently.
Trabeculectomy Suitability Score
Enter your details below to check your suitability for this treatment
Suitability Level
Recommendation
Cost and Price
In the U.S., trabeculectomy is typically covered by medical insurance when medically necessary. Your total cost depends on your plan, deductibles, and the setting (hospital or ambulatory surgery center). A practical way to budget is to ask your clinic for an itemized estimate separating: surgeon fee, facility and anesthesia fees, and postoperative visits. Coding resources list common procedure codes such as CPT 66172 (trabeculectomy with anti-scarring agent), which your insurer may use when reviewing authorization and benefits. 7 If a cataract operation is done in the same sitting (a phacotrabeculectomy), your estimate may include combined-surgery details; ask what’s bundled and what happens if additional procedures are needed later. 8
Other costs to plan for:
- Prescription eye drops and protective shields.
- Possible office procedures (e.g., laser suture lysis or small anti-scarring injections) within the global period.
- For high-deductible plans: ask about payment plans and use of HSA/FSA funds.
Bring your insurance card to the pre-op visit so benefits can be checked and any prior authorization submitted. A clear, written estimate helps avoid surprises and supports smoother recovery and follow-up.
Benefits and Limitations
Benefits:
- Can lower eye pressure substantially—often more than drops or some lasers—and may reduce or eliminate daily glaucoma medicines. 9
- Compared with tube shunts, both approaches can work; in some analyses, trabeculectomy reached similar pressures with fewer medications in selected patients.
Limitations & risks: Success depends on healing—too much scarring can block flow, while too much flow can cause low pressure (hypotony). Early bleb leaks, infection risk around the bleb, cataract progression, and temporary blurred vision are possible. Postoperative tools such as laser suture lysis and targeted anti-scarring injections help fine-tune pressure and keep the bleb healthy during healing. 12
Recovery and Long-Term Care
The first weeks: You’ll use prescribed drops to prevent infection and calm inflammation. Light activities usually resume within a week, but avoid heavy lifting, bending, straining, hot tubs, and eye rubbing while tissues heal. Your surgeon will check the bleb often and may adjust stitches or perform minor in-office treatments to guide pressure into the safe zone. Call right away for increasing pain, redness, discharge, or sudden vision changes. 11
Over time, visits space out, but lifelong glaucoma care continues to watch pressure, optic nerve health, and visual fields—pressure can drift upward again. 14
Daily success tips:
- Take drops exactly as directed.
- Use a protective shield during sleep as advised.
- Keep showers gentle (face turned away) at first.
- Bring all medicines to follow-ups so the team can simplify your routine when possible.
Latest Research & Innovations
Randomized trial reports continue to shape expectations for pressure lowering, medication use, and safety. Five-year results from the Primary Tube Versus Trabeculectomy (PTVT) Study showed both surgeries can achieve similar average pressures; in some analyses, trabeculectomy required fewer medications—reinforcing that procedure choice should be personalized. 10
Reviews explore strategies to prevent scarring (optimized MMC/5-FU dosing, collagen matrices, targeted anti-fibrotic delivery) and to standardize early postoperative adjustments for better long-term bleb health. Guidelines emphasize setting and maintaining a safe target pressure over a lifetime, using the full toolbox (drops, laser, trabeculectomy, tubes) as needed. 12 Clear communication about goals, side effects, and warning signs helps patients stay engaged and protects vision.
Recently Published in Peer-Reviewed Journals
JAMA ophthalmology
August 7, 2025
Omidenepag Isopropyl-Associated Cystoid Macular Edema After Trabeculectomy.
Zur D, Rachmiel R
JAMA ophthalmology
August 7, 2025
Prostaglandin EP2 Receptor and Cystoid Macular Edema in Phakic Posttrabeculectomy Eyes.
Cheng MH, Hwang DK, Liu CJ
Ophthalmology. Glaucoma
July 31, 2025
Glaucoma Surgery: From the Tried and True to the Novel and New.
Gedde SJ, Herndon LW Jr
Next Steps
If your pressure is still too high or vision is worsening, bring a simple packet to your visit: your drop list (with times), any side effects, recent IOPs, and your goals (night driving, reading, fewer drops). This helps your glaucoma specialist decide whether trabeculectomy is the right next step and how to plan your aftercare. 13 You can also review plain-language surgery information to know what to expect during healing and how follow-up adjustments work. 16
Reminder: This page is for education only. Decisions about surgery are personal and should be made with your doctor after a full exam. If trabeculectomy is chosen, staying on schedule with visits and medicines gives you the best chance of long-term success.