Normal-Tension Glaucoma
also known as Low-Tension Glaucoma
Last updated September 3, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.


Overview
Normal-tension glaucoma (NTG) is a form of open-angle glaucoma where the optic nerve is damaged and side vision is lost even though measured eye pressure stays in the typical range. This happens because some optic nerves are more sensitive to pressure or have reduced blood flow.
NTG usually progresses slowly and is painless, so many people do not notice changes early on. Treatment focuses on lowering your eye pressure from your personal baseline to protect the nerve, even if your starting pressure is "normal." 2
A landmark research program found that lowering eye pressure by about 30% can reduce the risk of NTG worsening for many patients. Your specialist will personalize the target based on your exam and test results. 1
Symptoms
Most people with NTG feel fine at first. Over time, it can cause:
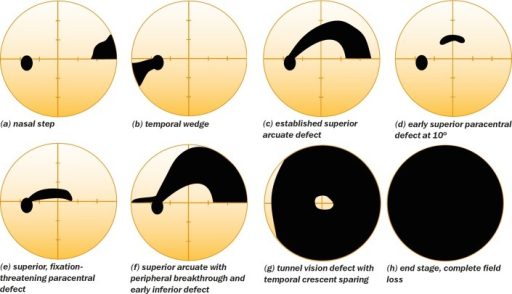
- Slow loss of side (peripheral) vision that is easy to miss in daily life.
- Blank or dim spots on visual field tests, sometimes near the center early on.
- Small bleeding spots on the optic nerve (disc hemorrhages) seen during an exam.
Because early NTG is subtle and painless, regular eye exams and specialized testing are important for finding it early. 3
Causes and Risk Factors
NTG likely reflects a mix of pressure sensitivity in the optic nerve and reduced blood flow. Risk factors include:
- Family history of glaucoma.
- Thin corneas, which can make measured pressure seem lower than it really is.
- Migraine or Raynaud’s (blood-vessel spasm tendencies).
- Very low blood pressure at night (nocturnal hypotension).
- Sleep apnea.
- Older age and, in some studies, Japanese/Asian ancestry.
Eye doctors also watch for optic disc hemorrhages, which can signal change. Managing sleep apnea and reviewing blood pressure timing with your primary care team may be part of care. 2 1
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
An eye specialist diagnoses NTG after a full work-up, which may include:
- Eye pressure (IOP) checks at different times of day.
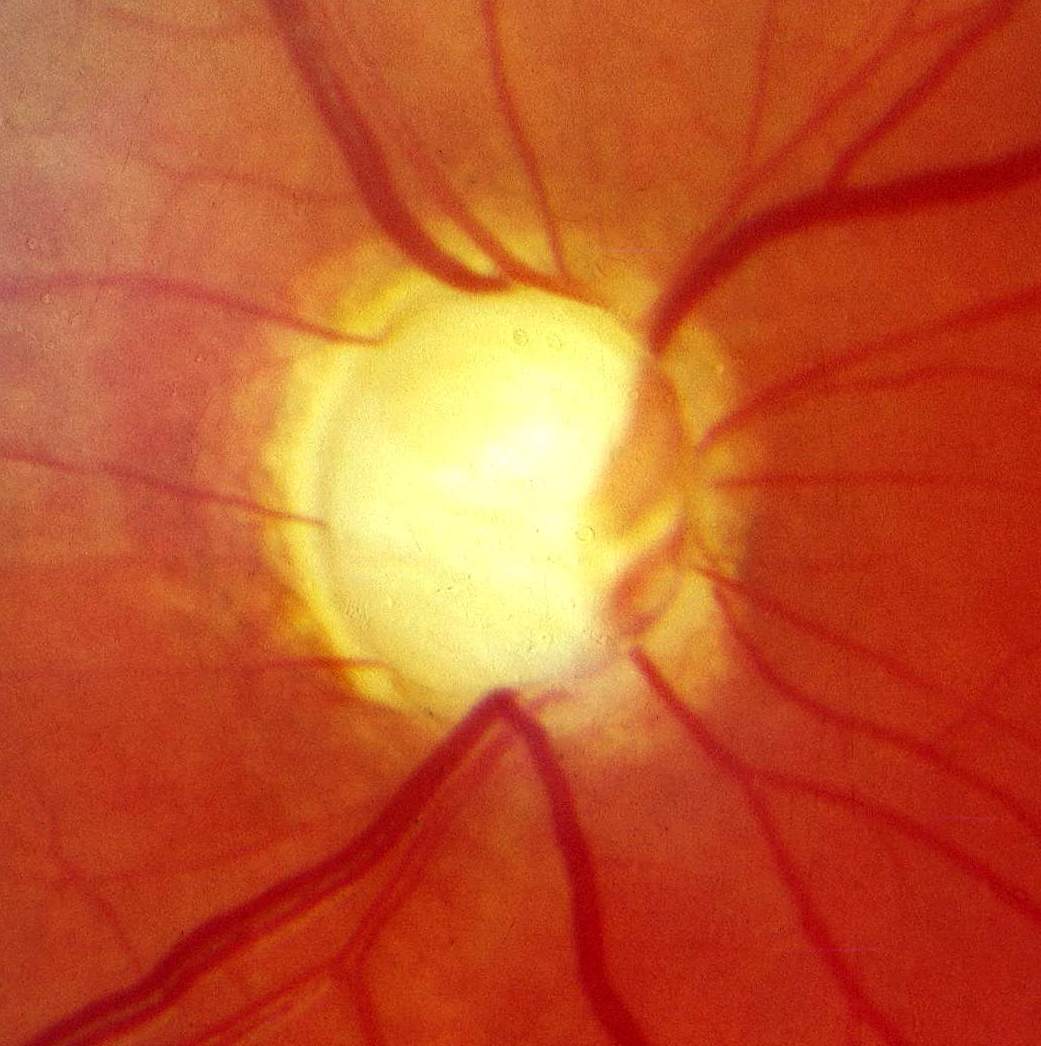
- Dilated optic nerve exam to look for thinning or disc hemorrhage.
- Optical Coherence Tomography (OCT) to measure nerve fiber and ganglion cell layers.
- Visual field testing to map blind spots and follow changes.
- Corneal thickness (CCT) measurement to detect masked higher pressure.
Other causes of optic nerve damage are ruled out. Results help guide monitoring frequency and treatment decisions. 4 2
Treatment and Management
The goal is to protect the optic nerve by lowering IOP from your baseline, usually by about 30%. 1
- Prescription eye drops: Prostaglandin analogs are common first-line treatments, with other options like beta-blockers, alpha-agonists, carbonic anhydrase inhibitors, and Rho-kinase inhibitors. 3
- Laser (SLT): A clinic laser helps fluid drain and can reduce or replace the need for daily drops.
- Surgery: Options like trabeculectomy, tube shunts, or MIGS may be used if progression continues.
Costs & Price Tips:
- Drops: Request generics, 90-day supplies, and once-daily dosing to reduce costs.
- SLT: Often billed as a minor procedure. Check deductibles and copays.
- Surgery: Typically covered if medically necessary. Request an itemized estimate and ask about combining with cataract surgery. 5
Daily habits: Take drops on schedule, treat sleep apnea, avoid smoking, stay active, and limit head-down yoga poses. 8
Living with Normal-Tension Glaucoma and Prevention
Living well with NTG is possible with consistent care:
- Stick to treatment: Use reminders and bring your bottles to visits.
- Keep follow-ups: Regular OCT scans and visual field tests track disease progression.
- Protect overall health: Treat sleep apnea and manage nighttime blood pressure.
- Eye safety: Wear protective glasses for sports and projects.
Early detection and treatment greatly reduce vision loss risk. 8
Latest Research & Developments
Beyond pressure lowering: Studies suggest brimonidine may slow vision loss compared to timolol, hinting at neuroprotective effects, though more research is needed.
Imaging blood flow: OCT angiography shows reduced vessel density around the optic nerve in NTG, potentially useful for monitoring. 6
New studies focus on nighttime blood pressure, sleep apnea, and ways to protect retinal ganglion cells. 7
Recently Published in Peer-Reviewed Journals
BMC ophthalmology
August 12, 2025
Correction: Efficacy analysis of microinvasive glaucoma surgery alone or in combination with phacoemulsification in patients with normal tension glaucoma: a systematic review and meta-analysis.
Yu Z, Wu M, Tao Y, et al.
Ophthalmology. Glaucoma
July 21, 2025
A Prospective Study of a New 24-2C Algorithm Using the Swedish Interactive Thresholding Algorithm Standard.
Nishijima E, Noro T, Sano K, et al.
Investigative ophthalmology & visual science
July 1, 2025
Natural Course and Risk Factors of Glaucoma Development in the Untreated Fellow Eye in Unilateral Normal-Tension Glaucoma.
Lee EJ, Park DY, Kee C, et al.
Next Steps
If you suspect NTG or were recently diagnosed:
- See a glaucoma specialist for confirmation and treatment planning.
- Bring your glasses prescription, medication list, and prior eye records.
- Ask about target pressure, test frequency, and scheduling tips.
- If wait times are long, request to be added to a cancellation list.
For fast guidance, you can connect on Kerbside for an educational consult (no physician–patient relationship formed). 8


