Retinal Artery Occlusion
Also known as RAO
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.
Overview
Retinal artery occlusion (RAO) happens when blood flow to the retina suddenly gets blocked. The retina is the light-sensing layer at the back of your eye. Without oxygen-rich blood, retinal cells can be injured within minutes. Doctors often call RAO an eye stroke, and it is an emergency. If you notice sudden vision loss in one eye—especially if it is painless—call emergency services or go to the nearest stroke-capable emergency department right away. Rapid treatment may protect vision and also check for problems that could lead to a brain stroke. 1
There are two main types: central retinal artery occlusion (CRAO), which affects the main artery, and branch retinal artery occlusion (BRAO), which affects a smaller branch. Both can cause significant vision problems and both need urgent care. 2
Symptoms
Most people with RAO describe sudden, painless vision loss in one eye. Vision may become blurry, dim, or blacked out. Some people notice a shadow or a curtain over part of their vision—this is more common with BRAO, which affects only a section of the retina. If the blockage briefly comes and goes, you may have short episodes of vision loss called amaurosis fugax. Any of these symptoms are emergencies. 2
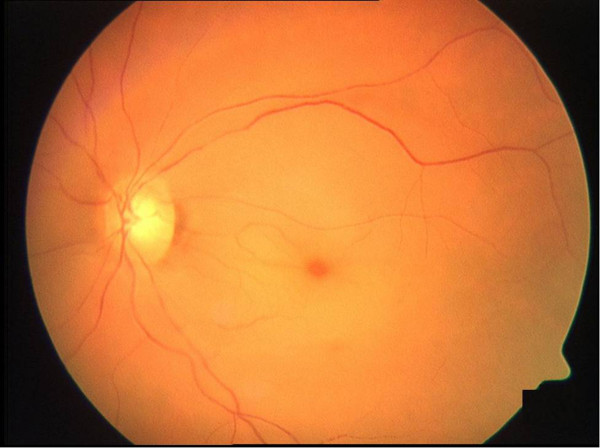
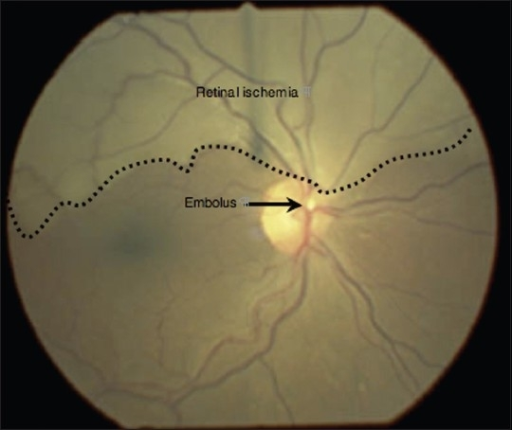
Other clues your eye doctor may see during an exam include a pale retina and a bright red spot in the center (a “cherry-red spot”). Because RAO is linked to conditions that can also cause brain stroke, sudden vision loss should trigger fast evaluation. 3
Causes and Risk Factors
RAO most often occurs when a tiny clot or cholesterol plaque breaks off from another part of the body—commonly the carotid arteries in the neck or the heart—and travels to the eye. Less commonly, inflammation of blood vessels (for example, giant cell arteritis in adults over 50) can narrow or block the artery. 3
Common risk factors include older age, high blood pressure, high cholesterol, diabetes, smoking, atrial fibrillation, carotid artery disease, and a prior stroke or transient ischemic attack. These risks overlap with those for brain stroke. In people over 50 with sudden vision loss and scalp tenderness, jaw pain with chewing, new headaches, or fatigue, doctors consider giant cell arteritis and start urgent testing and treatment. 5
RAO Immediate Concern Score (for triage and urgency guidance)
Select your details to estimate risk factors.
Diagnosis
Your eye care team will ask about symptoms and medical history, check vision and pupils, and examine your retina after dilating the pupil. Classic findings may include retinal whitening and a central “cherry-red spot.” Imaging tests can help confirm the diagnosis and rule out other vision emergencies:
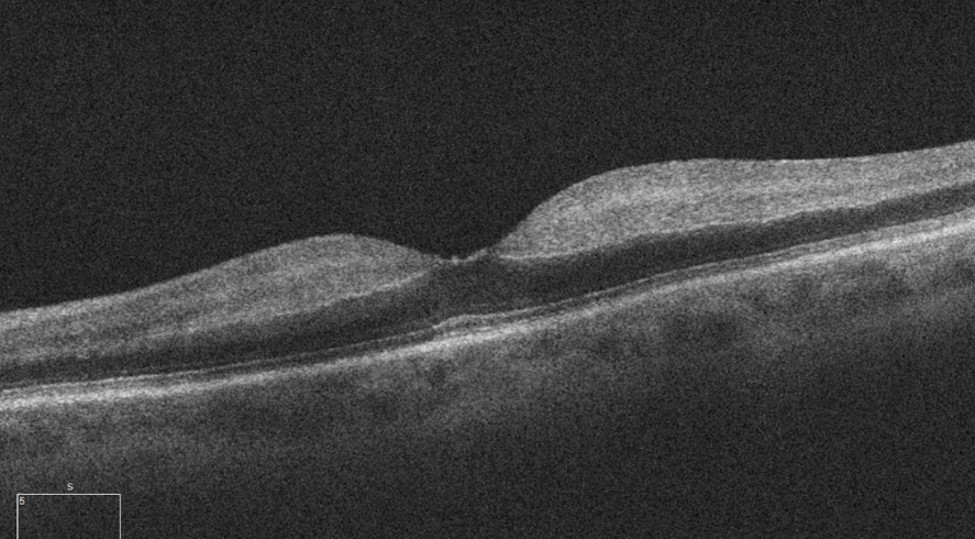
- Optical coherence tomography (OCT): shows swelling (hyperreflectivity) in the inner retina in acute RAO.
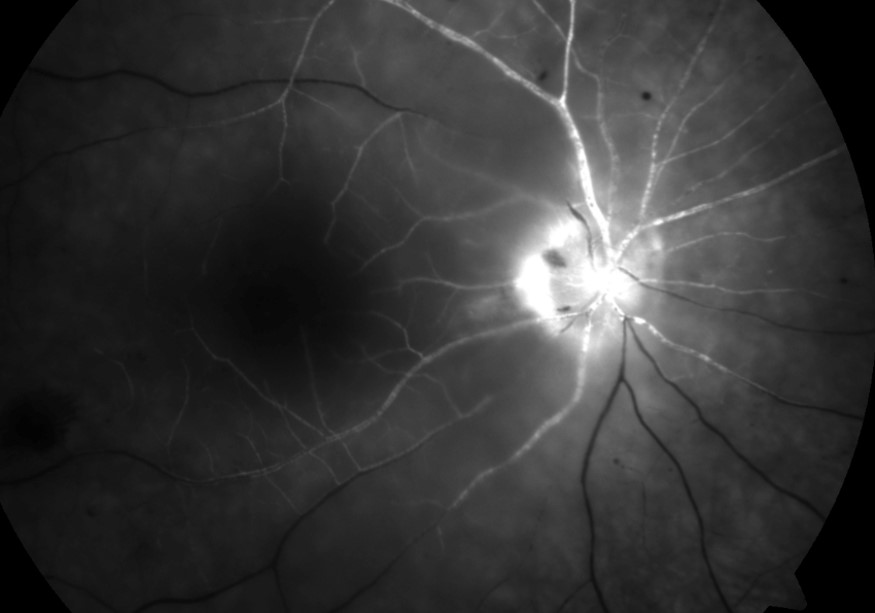
- Fluorescein angiography (FA): shows delayed or blocked filling of retinal arteries.
- Stroke workup: urgent tests may include brain MRI, carotid imaging, heart rhythm monitoring, and blood tests. In patients over 50, blood tests for inflammation (ESR and CRP) help screen for giant cell arteritis.
These steps guide both eye treatment and prevention of future strokes. 5 3
Treatment and Management
RAO is managed like a stroke. The first goal is to quickly restore or support blood flow to the retina, when possible, and to evaluate for conditions that could cause another stroke. Current expert guidance emphasizes:
- Immediate stroke-center referral: Patients with acute, symptomatic CRAO or BRAO should be evaluated at the nearest stroke-capable center. Some centers consider thrombolysis (clot-busting medicine), especially if symptoms started within about 4.5 hours, following stroke protocols. Evidence is evolving and shared decision-making is important.
- Adjuncts: Hyperbaric oxygen therapy (HBOT) may be considered at experienced centers as a temporizing measure when available, although proof of benefit is limited. Maneuvers like ocular massage or lowering eye pressure have not shown reliable vision gains in studies. 1
- Rule out giant cell arteritis: In patients over 50 with suggestive symptoms or signs, doctors start steroids quickly to protect the other eye while confirmatory testing proceeds.
- Secondary prevention: After the acute phase, a team (often ophthalmology, neurology, cardiology, and primary care) addresses carotid or cardiac sources, blood-thinner needs, blood pressure, cholesterol, diabetes, and smoking cessation to reduce risk of another event. 6
Living with Retinal Artery Occlusion and Prevention
Some people recover part of their sight, but many have lasting vision loss after RAO. Your care plan will focus on protecting your overall health and helping you function well day to day. Practical steps include:
- Stroke risk reduction: keep blood pressure, cholesterol, and blood sugar controlled; take prescribed antiplatelet or anticoagulant medicines if recommended; and stop smoking.
- Heart and vessel checks: evaluation for carotid narrowing, atrial fibrillation, and other sources of clots helps prevent future events.
- Vision rehabilitation: low-vision tools and training can improve reading, mobility, and independence if vision remains limited.
Population-based research suggests there is a small but real increase in symptomatic stroke around the time of a CRAO, underscoring the need for urgent evaluation and prevention steps. 4 For everyday prevention and symptom recognition tips, see this patient-friendly overview. 2
Latest Research & Developments
RAO is increasingly treated as a vascular emergency similar to brain stroke. Recent expert statements highlight three themes: (1) rapid recognition and referral to stroke-capable centers, (2) ongoing clinical trials of thrombolysis for carefully selected patients within a short time window, and (3) system-wide efforts to improve public and clinician awareness so patients arrive earlier. 1
Ophthalmology resources have also consolidated best practices for diagnosis—including OCT patterns and fluorescein angiography findings—and stress evaluation for embolic and inflammatory causes, reflecting updated guidance through professional organizations. 5
Recent Peer-Reviewed Research
Successful intra-arterial thrombolysis for central retinal artery occlusion secondary to chronic internal carotid artery occlusion: a case report.
Pang F, Yin C, Zhan J, et al.
Intraretinal arterial cannulation for central retinal artery occlusion caused by cosmetic facial injection.
Li H, Cai S, Lin R
Sequential bilateral retinal artery occlusions with promising visual prognosis in a diabetic patient: a case report and literature review.
Li Z, Li Y, Chen T, et al.
Next Steps
If you are having sudden vision loss now, call emergency services or go to the nearest emergency department that can manage strokes.
If your symptoms have improved or you were already diagnosed, the best specialist to see for eye care is a retina specialist (ophthalmologist). Many people also benefit from coordinated care with a neurologist or stroke clinic to address the underlying cause and reduce future risk. Depending on your location, you may need a referral from your primary care provider, and there could be waitlists. Ask to be placed on a cancellation list for the earliest available appointment, and tell schedulers that you recently had an eye stroke.
For education and care coordination, you can also connect on Kerbside to get matched to the right specialist for a medical education consult. This is not a patient–physician relationship, but it can help you prepare for visits, understand tests, and know which questions to ask.
Trusted Specialists
Board-certified providers specializing in Retinal Artery Occlusion.



