YAG Laser Capsulotomy
also known as YAG Capsulotomy
Last updated August 10, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.
Overview
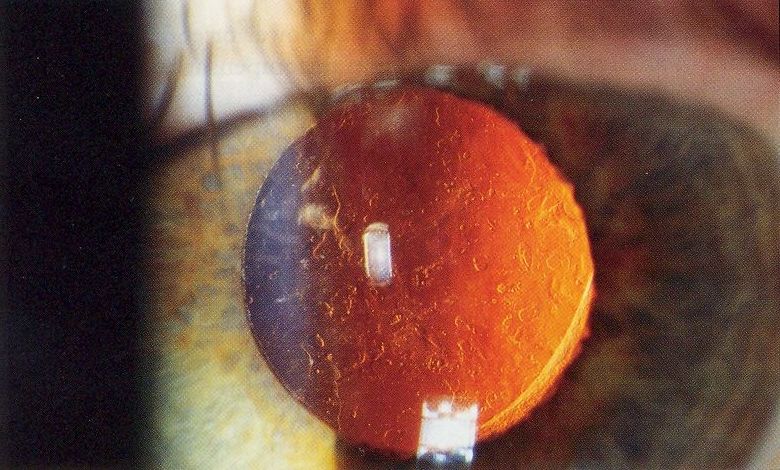
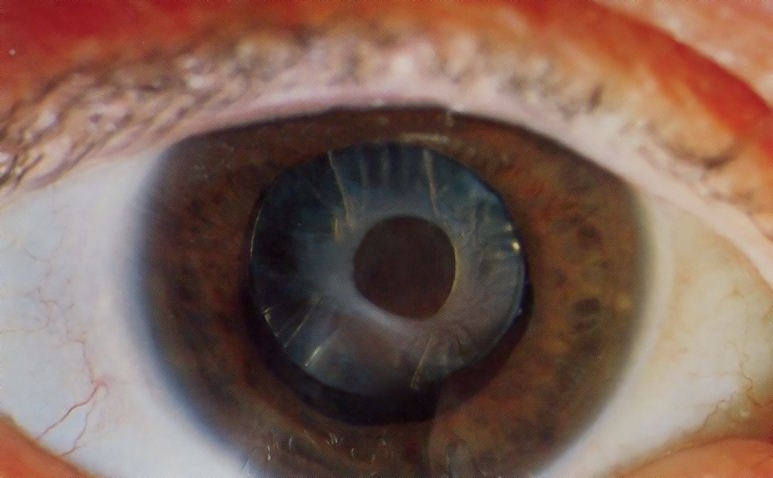
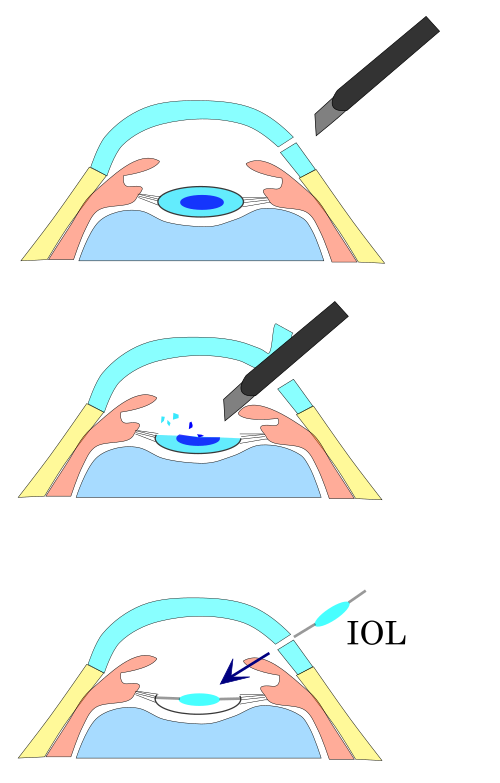
Months or years after cataract surgery, the thin membrane that holds your new lens can turn cloudy. Doctors call this posterior capsule opacification (PCO), and it can blur vision much like the original cataract. A YAG laser capsulotomy is a quick, outpatient treatment that clears a tiny window in that cloudy membrane so light can reach the retina again. Most people notice sharper vision within hours, and the risk of serious problems is low.1 The procedure has become the standard of care worldwide, with millions performed safely every year.2
How the Procedure Works & Options
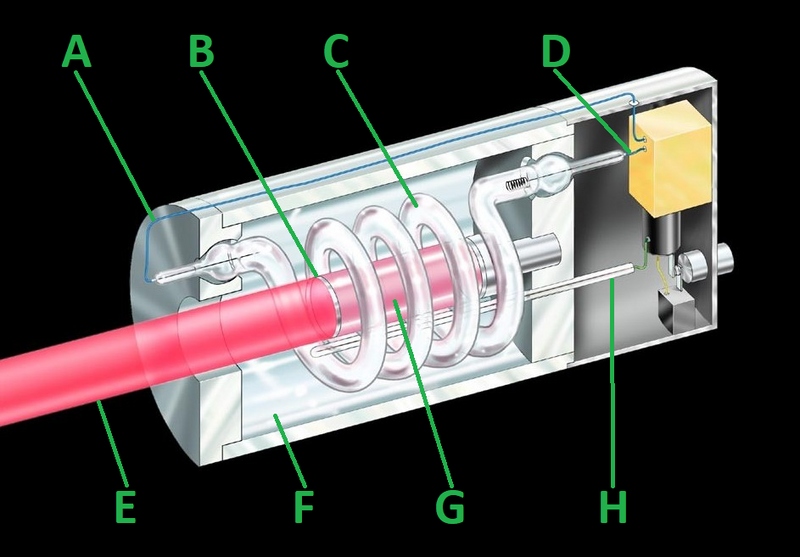
In the exam room, your eye is numbed with drops and a special contact lens is placed on the surface to help focus the Nd:YAG laser. The doctor aims short laser pulses to cut a dime-sized opening in the back of the capsule; no blades or stitches are needed. The treatment itself takes less than one minute, although plan on 10–15 minutes for setup. Variations include size-customized openings for multifocal or toric lenses and combined treatments with micropulse lasers for patients at risk of eye-pressure spikes.1 Clinical studies show modern laser settings keep energy levels low while maintaining success rates over 95 percent.2
Who Is a Candidate?
You may benefit if you had cataract surgery at least three months ago and now struggle with hazy or glare-filled vision, especially when reading or driving at night. Eye exams often reveal a frosted-glass appearance on the posterior capsule. Good candidates have a healthy cornea and retina, stable intraocular lens (IOL) position, and no active eye infection. People with very high myopia, uveitis, or a history of retinal detachment need extra discussion because their risk profile is a bit higher.1 Your ophthalmologist will weigh these factors along with your day-to-day visual goals.2
YAG Capsulotomy Suitability Score
Enter your details below to check your suitability for this treatment
Suitability Level
Recommendation
Cost and Price
In the United States, most private insurers and Medicare cover YAG capsulotomy because it is considered medically necessary once vision drops below 20/40 or daily tasks are affected. Typical out-of-pocket costs for insured patients range from USD 0–150 (copay or coinsurance). For self-pay, fees average USD 500–1 000 per eye, which usually includes the laser session, facility fee, and one follow-up visit. Exact pricing depends on geography, facility type, and whether additional tests (such as OCT) are required.1 Because recovery is almost immediate, there are no extra costs for time off work in most cases.2
Benefits and Limitations
The main benefit is rapid, lasting visual improvement; studies report 90–95 percent of patients regain pre-PCO clarity after one treatment. The procedure is painless, incision-free, and performed in minutes. Limitations include a small chance of increased eye pressure, floaters, pitting of the IOL surface, or, rarely, retinal detachment. Most complications are minor and treatable with drops or additional care.1 Long-term data show less than 2 percent of eyes need a repeat laser because the capsule cannot become cloudy again in the opened area.2
Recovery and Long-Term Care
You can return to normal activities almost right away, but mild floaters or light sensitivity may last a day or two. Your doctor will check eye pressure about an hour after the laser and again in one to two weeks. Prescription anti-inflammatory drops are often used for three to five days. Serious problems such as retinal detachment are very uncommon; however, call your doctor immediately if you see a curtain-like shadow, flashes of light, or a sudden shower of floaters.1 Most people do not need additional long-term medications, but regular yearly eye exams are still important.2
Latest Research & Innovations
Recent laboratory and clinical studies focus on laser energy delivery patterns that further reduce IOL pitting and postoperative pressure spikes. One study comparing newer low-energy burst modes to standard single-pulse modes found equal clearing of the capsule with 40 percent less total energy.1 Researchers are also exploring prophylactic IOL edge designs and drug-eluting lenses to minimize the need for future capsulotomy.2
Recently Published in Peer-Reviewed Journals
BMC ophthalmology
April 10, 2025
Posterior capsule opacification treatment using Nd: YAG laser capsulotomy: 36 months retrospective analysis.
Montrimas A, Rinkevičiūtė J, Žemaitienė R
BMC ophthalmology
November 5, 2024
Rapid posterior capsular opacification in two patients treated for negative dysphotopsias.
Navia JC, Huang JJ, Reategui JA, et al.
BMC ophthalmology
February 2, 2024
A potential role for inflammatory cytokines in a rare late-onset capsular block syndrome: a case report.
Du YH, Liang XF, Hirooka K, et al.
Next Steps
If cloudy vision is limiting your work, hobbies, or driving, schedule a complete dilated eye exam. An ophthalmologist can confirm posterior capsule opacification, review your medical history, and explain whether a YAG laser capsulotomy is right for you. You can connect with the right specialist on Kerbside for a medical-education consult—no physician-patient relationship will be created.12
Trusted Providers for YAG Laser Capsulotomy

Dr. Nicholas Carducci
Specialty
Ophthalmology
Education
UPenn

Dr. Karen Chen
Specialty
Ophthalmology
Education
Harvard Medical School

Dr. Levi Kanu
Specialty
Ophthalmology
Education
Harvard Medical School

Dr. Emily Eton
Specialty
Ophthalmology
Education
Harvard Medical School

Dr. Owen Qi
Specialty
Ophthalmology
Education
Washington University in St. Louis

Dr. Jose Davila
Specialty
Ophthalmology
Education
Harvard Medical School

Dr. Connie Wu
Specialty
Ophthalmology
Education
Brown University

Dr. Grayson Armstrong
Specialty
Ophthalmology
Education
Harvard Medical School

Dr. Emily Schehlein
Specialty
Ophthalmology
Education
Johns Hopkins University