Kahook Dual Blade Goniotomy
Also known as KDB Goniotomy
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms for details.
Overview
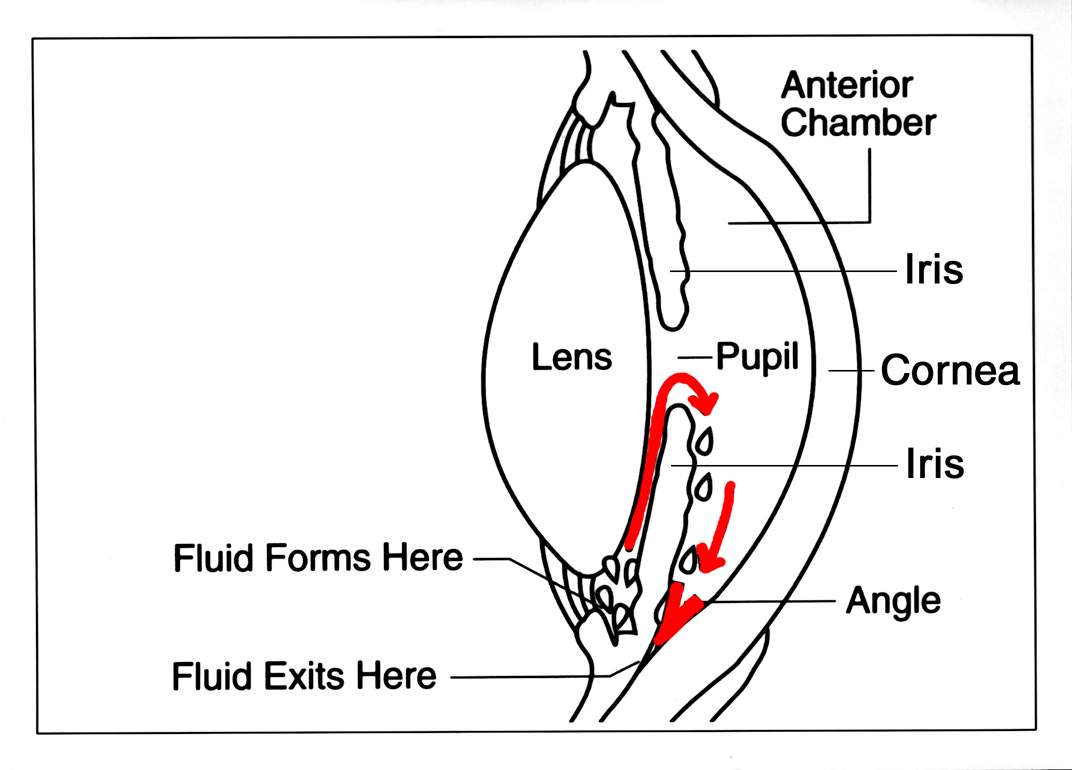
Kahook Dual Blade (KDB) goniotomy is a minimally invasive glaucoma surgery (MIGS) that helps lower eye pressure by removing a thin strip of the eye’s natural drain (the trabecular meshwork) from inside the eye. Lowering pressure protects the optic nerve and can slow or prevent vision loss from glaucoma.1
With special mirrors and a tiny, single-use blade, the surgeon gently opens the drainage system so fluid (aqueous humor) can leave the eye more easily through the normal pathway.2
KDB goniotomy is often paired with cataract surgery in adults with mild to moderate primary open-angle glaucoma (POAG), but it can also be performed on its own. The goal is to lower intraocular pressure (IOP) and reduce the number of daily glaucoma drops.
How the Procedure Works & Options
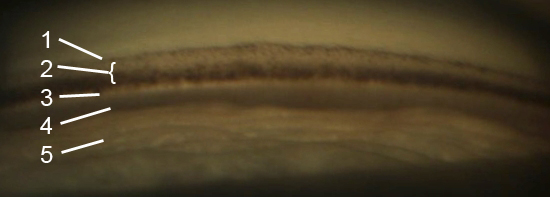
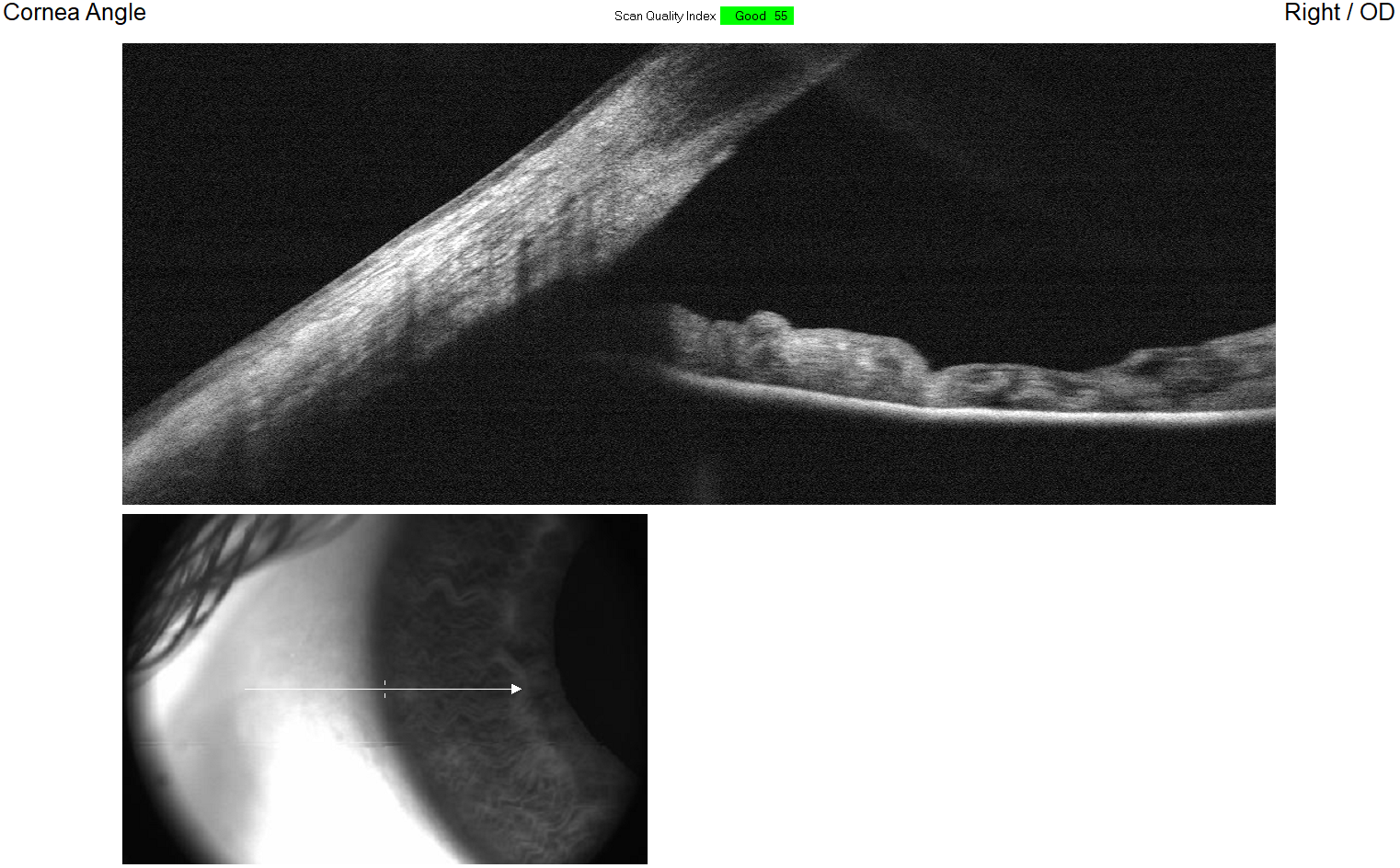
Step by step: Through a micro-incision, the surgeon uses a viewing lens (gonioprism) to see the drainage angle. The KDB’s dual blades excise a narrow strip of trabecular meshwork, opening Schlemm’s canal over a small arc. This improves access to the canal and its collector channels, helping fluid exit where it should.3
KDB goniotomy is usually done with numbing and mild sedation, and because no implant is left behind, implant-related risks are avoided.
Where it fits: Glaucoma care is personalized and may include:
- Drops
- Laser trabeculoplasty
- Canal-based MIGS (like KDB)
- Traditional surgeries (trabeculectomy or tube shunt)
Doctors choose based on glaucoma type, optic nerve health, and target IOP.4
Who Is a Candidate?
Often considered for: Adults with mild to moderate POAG (and some other open-angle glaucomas) who have an open angle on gonioscopy and need better pressure control or fewer daily drops. Your doctor will also consider optic nerve status and a reasonable target IOP.4
Because the procedure uses the eye’s natural drain, it is not for angle-closure glaucoma where the angle is blocked.2
What evidence suggests: Studies show meaningful IOP reduction and fewer medications after KDB goniotomy, both as stand-alone and with cataract surgery.
Is KDB Goniotomy a Good Fit for Me?
Select your details to estimate suitability.
Cost and Price
What affects cost: Setting (clinic, ASC, hospital), insurance plan, and whether KDB is combined with cataract surgery. In the U.S., many glaucoma procedures are outpatient under Medicare Part B or commercial insurance; you typically owe deductible and coinsurance.7
If done in a hospital outpatient department, Medicare outpatient rules apply; copayments and facility fees can differ.8
How to prepare: Ask your surgeon’s office to verify benefits and any prior authorization. Request a written estimate that includes surgeon fee, facility fee, and anesthesia. Medication costs may drop if you need fewer drops post-surgery.
Benefits and Limitations
Benefits you may notice: Many patients have lower IOP and need fewer drops after KDB goniotomy. Peer-reviewed series show meaningful reductions with a generally favorable safety profile.3
Limits & risks: Not everyone reaches target pressure. Some still need drops or later procedures. Common short-term effects include:
- Light sensitivity
- Mild inflammation
- Small layered hyphema (blood) that clears with time
Rare risks include pressure spikes, scarring that limits flow, or additional surgery.5
Recovery and Long-Term Care
Right after surgery: Most people go home the same day. You may have mild scratchiness, light sensitivity, or blurry vision. Surgeons often prescribe anti-inflammatory drops and check your pressure within the first day or week, then again later. Benchmarks recommend early postoperative checks and ongoing follow-up.11
When to call: Worsening pain, a big drop in vision, dense redness, or many new floaters are warning signs—contact your surgeon promptly.
Latest Research & Innovations
What studies show: Studies report significant IOP and medication reductions with KDB, both stand-alone and with cataract surgery.
Newer analyses examine success factors over 1–5 years.14
Emerging data: Technique (arc length, heme control) and patient selection are key.13
Recent Peer-Reviewed Research
Kahook dual blade goniotomy combined with phacoemulsification in eyes with primary open angle glaucoma and pseudoexfoliation glaucoma: comparative study.
Koylu MT, Yilmaz AC, Gurdal F, et al.
Trabecular Procedures Combined with Cataract Surgery for Open-Angle Glaucoma: A Report by the American Academy of Ophthalmology.
Richter GM, Takusagawa HL, Sit AJ, et al.
Outcomes of standalone ab interno trabeculotomy in the treatment of open-angle glaucoma in eyes with high myopia.
Yoshida T, Nomura T, Yoshimoto S, et al.
Next Steps
If you’re considering KDB goniotomy—especially if you also need cataract surgery—schedule a visit with a board-certified ophthalmologist (ideally a glaucoma specialist). You can search by location and subspecialty using the AAO directory.15
Urgent signs: Sudden severe eye pain, halos, headache, or rapid vision changes need immediate care.16