Toric Intraocular Lens
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.

Overview
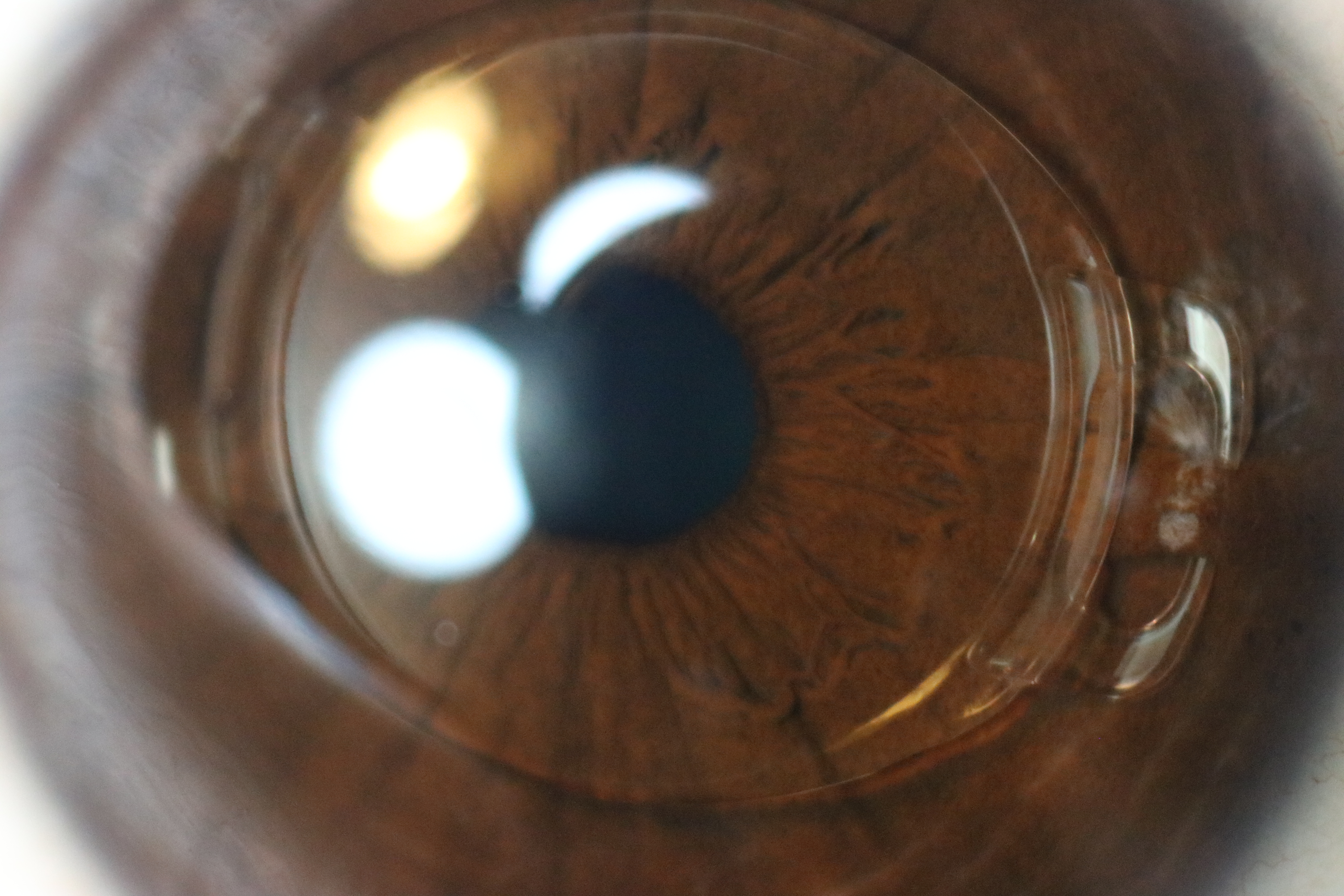
A toric intraocular lens (IOL) is a special lens implanted during cataract surgery to correct astigmatism at the same time the cloudy natural lens is removed. Cataract surgery is the only way to remove a cataract and is one of the most common outpatient surgeries, with a strong safety record. 1
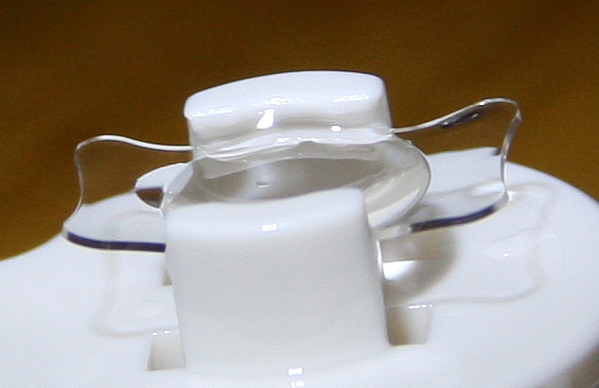
Toric IOLs have built-in astigmatism power (like the cylinder in eyeglasses). When aligned to the correct axis, they help create clearer, sharper distance vision and can lower the need for glasses after surgery. 2
How the Procedure Works & Options
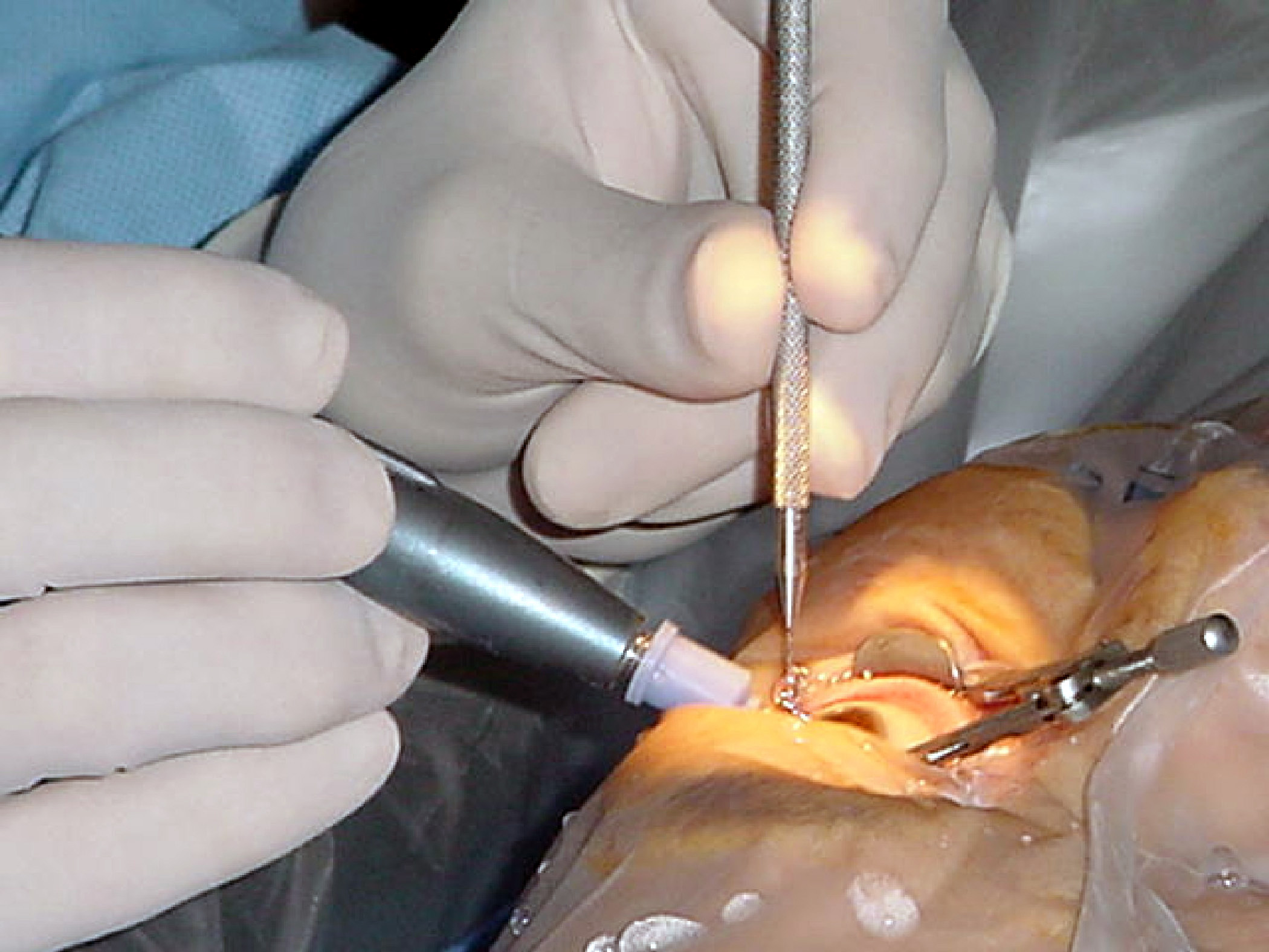
Step 1: Cataract removal and IOL placement. After numbing drops, the surgeon makes a tiny opening, breaks up and removes the cloudy lens, and places the new IOL into the natural lens capsule. Most people go home the same day, and the procedure often takes less than an hour per eye. 3
Step 2: Toric alignment. The toric IOL has marks that must line up with your eye’s astigmatism axis; careful measurements and planning before surgery guide the power and axis choice. Your surgeon may also offer a toric version with different strengths to match your corneal shape. 4
- Planning tools: keratometry/topography, toric calculators, and sometimes intraoperative aberrometry.
- Goal setting: discuss target focus for distance and glasses needs for near.
Who Is a Candidate?
You may be a good candidate if you have regular corneal astigmatism, a visually significant cataract, and healthy eye structures (cornea, macula, optic nerve). Toric IOLs are designed to reduce regular astigmatism; very irregular astigmatism (for example from keratoconus or scars) often needs a different plan. 5
Is a Toric IOL a Good Fit for Me?
Select your details to estimate suitability.
Cost and Price
Insurance basics: In the U.S., Medicare and many insurers cover medically necessary cataract surgery with a conventional (monofocal) IOL. When you choose a toric IOL to correct astigmatism, the extra cost for the astigmatism-correcting feature is typically an out-of-pocket upgrade, while the base cataract surgery remains covered. Always confirm with your plan and ask your clinic to explain what is and isn’t included. 7
Typical patient costs: Harvard Health notes that toric lenses commonly add about $1,500–$2,500 per eye (practice and region vary). Wider-range lenses may cost more. Request an itemized quote and ask about payment options (HSA/FSA, financing). 8
- Your quote may include: toric IOL upgrade, surgeon’s refractive planning fee, facility/technology fees, diagnostics, and non-routine follow-up.
- Smart questions: Will a toric lens fully treat my astigmatism? What if the lens rotates and needs repositioning—how is that billed? Are postoperative glasses, YAG laser (if needed), or enhancements included or discounted?
Benefits and Limitations
Benefits: Compared with non-toric monofocal lenses, toric IOLs more predictably reduce postoperative astigmatism and improve unaided distance vision when eyes are healthy and measurements are accurate. 9 Many patients enjoy clearer distance vision for driving and outdoor activities with less dependence on glasses.
Limitations & trade-offs: Toric IOLs must stay on the planned axis; rotation can reduce the effect (about 3.3% loss of astigmatism correction per degree off axis, ~33% at 10°). Precise planning and follow-up are important, and some patients still need glasses for fine-tuning or near tasks. 10
Recovery and Long-Term Care
Most people see improvement within days, with most healing over a few weeks. You’ll use prescribed eye drops, avoid rubbing, and limit heavy lifting and swimming briefly. Your surgeon will check that the toric IOL remains aligned; if a meaningful rotation occurs, a quick in-office or operating-room adjustment may be recommended. 11
Later, a common and treatable haze behind the lens called posterior capsule opacification (PCO) can blur vision; a short YAG laser visit can restore clarity if needed. 12
- Call promptly for: increasing pain, sudden blur, new floaters/flashes, or redness/light sensitivity.
Latest Research & Innovations
Current reviews in top journals support treating corneal astigmatism during cataract surgery and highlight toric IOLs as a predictable option when planned carefully (including accounting for posterior corneal astigmatism and surgically induced astigmatism). 13
Newer hydrophobic acrylic platforms and refined haptic designs continue to improve rotational stability in real-world studies.
Planning tools: modern toric calculators and intraoperative aberrometry help choose power and axis more accurately—tailored to corneal shape, prior surgeries, and lifestyle. 14
Recent Peer-Reviewed Research
One-year outcomes of a trifocal intraocular lens with glistening-free hydrophobic acrylic using the mix-and-match technique.
Choi S, Choi YS, Nam DJ, et al.
Changes of corneal biomechanical and biometrical properties after combined phacoemulsification with viscocanalostomy surgery in patients with open-angle glaucoma.
Azimi A, Sadeghi E, Hassanipour H, et al.
Comparison of Surgical Methods for the Correction of Low Amounts of Corneal Astigmatism during Cataract Surgery.
Schallhorn SC, Schallhorn JM
Next Steps
Who to see: A cataract and refractive ophthalmologist who routinely implants toric lenses. Ask about your astigmatism amount, target focus for each eye, and how the team manages lens alignment and any rare need for repositioning. For Medicare beneficiaries, a specific ruling allows patients to choose an astigmatism-correcting (toric) IOL and pay only for the refractive portion while the medically necessary cataract surgery remains covered. 15 After cataract surgery with an IOL, Medicare Part B also covers one pair of glasses or one set of contact lenses; ask your clinic how this is handled. 16
- Prep tips: bring your glasses prescription, medication list, and prior eye records to maximize the value of your visit.
Trusted Specialists
Board-certified providers specializing in Toric Intraocular Lens.








