Laser Peripheral Iridotomy
Also known as LPI
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.


Overview
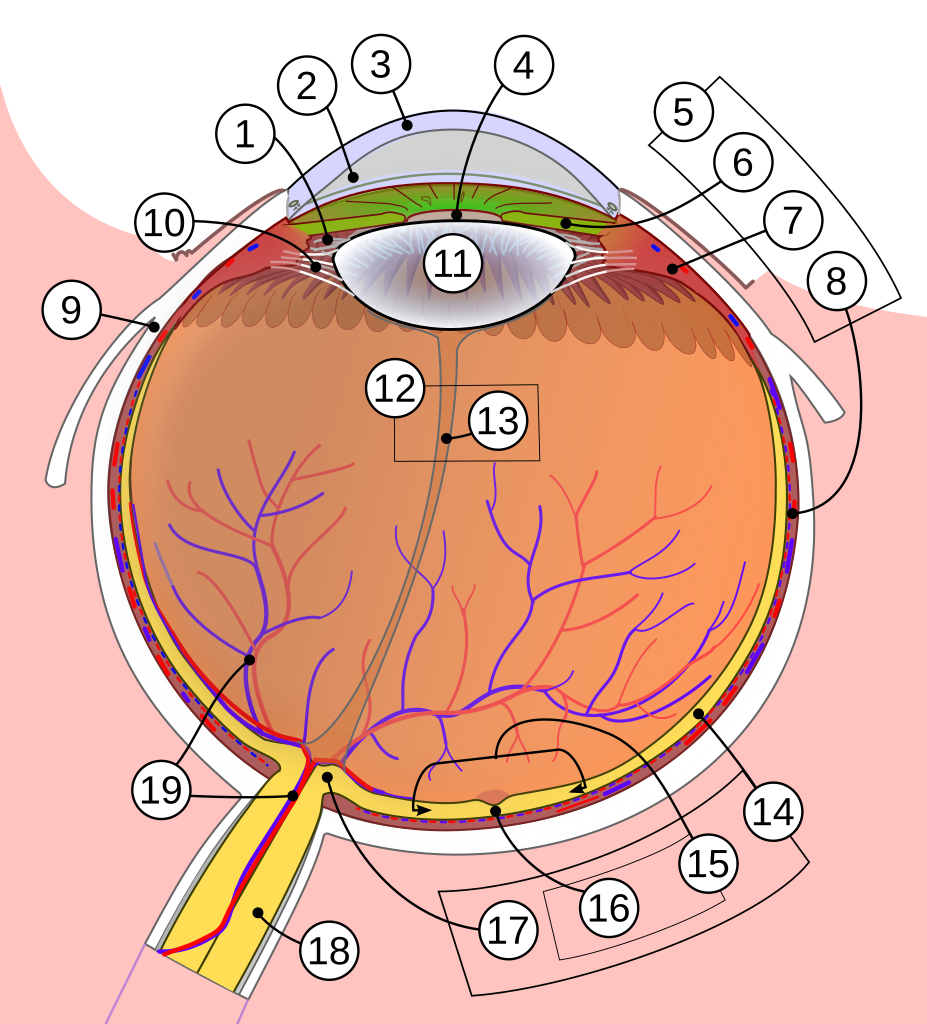
Laser peripheral iridotomy (LPI) is a quick outpatient laser procedure used to prevent or treat a type of angle-closure glaucoma caused by a pupillary block. The laser makes a tiny opening near the edge of the colored part of the eye (the iris) to create a new path for aqueous fluid to move from the back of the eye to the front so it can drain more normally, lowering eye pressure and protecting the optic nerve.1
Angle-closure can be sudden and severe, bringing symptoms like eye pain, headache, halos around lights, nausea, and blurry vision. It is a medical emergency—people with these symptoms should seek urgent eye care immediately.2
Why does this happen? In some eyes, the iris bows forward and crowds the drainage angle (where the cornea and iris meet). When the pupil is mid-dilated, the flow of fluid through the pupil can get blocked and pressure builds behind the iris, pushing it even more forward. LPI creates a small “pressure-release valve,” which helps the iris relax back and opens the angle. By addressing the main mechanism, LPI lowers the chance of damage to the optic nerve, which is the “cable” that carries vision from your eye to your brain. The procedure itself usually takes only minutes, but the benefits can be long-lasting when the anatomy is right.
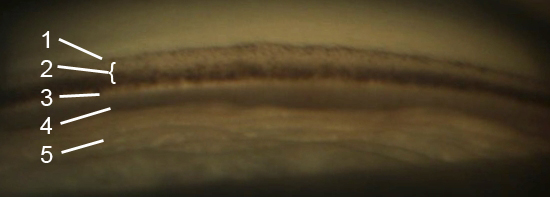
People at higher risk include those with narrow angles found on routine eye exams, individuals who are far-sighted (hyperopic), older adults, and in some populations, people of East or Southeast Asian descent. Certain medicines that dilate the pupil can also worsen a narrow angle, which is why knowing your angle status is important before some eye drops or procedures. Your eye doctor can diagnose narrow angles using a special mirrored lens in a test called gonioscopy and may also use imaging such as anterior segment OCT to measure crowding around the drainage area.
How the Procedure Works & Options
Step-by-step: Most LPIs are done with an Nd:YAG laser at a slit-lamp microscope. After numbing drops, the surgeon places a special contact lens on your eye to focus the laser. A few brief pulses create a pinhole opening in the peripheral iris—usually under the upper eyelid between 11 and 1 o’clock—so fluid has another route forward and the angle can open. In some eyes with thicker, darker irides, the surgeon may first use a different laser to thin the tissue, then complete the opening with the YAG laser. These choices depend on your iris color and thickness, the view, and the surgeon’s preference.3
During an acute attack: If you arrive with very high pressure and pain, medicines (pressure-lowering drops, pills, or sometimes IV medication) are given first to make the eye safer for laser. When the pressure is lower and the cornea is clearer, the LPI is performed to fix the block. Other options may be considered in selected cases, such as laser iridoplasty (to shrink the peripheral iris) or removing the natural lens when lens crowding is a major part of the problem. Your ophthalmologist will tailor the plan to your eye’s anatomy and the urgency of your situation.4
- Before: You may receive pressure-lowering drops and a pill to prevent a temporary pressure spike, and your eye will be numbed.
- During: You sit at the microscope, a lens rests gently on the eye, and you see bright lights. The laser pulses last fractions of a second.
- After: Your team checks the eye pressure, confirms the opening, and gives anti-inflammatory drops. Most people go home the same day and resume light activities soon after.
Who Is a Candidate?
LPI is commonly recommended for people across the primary angle-closure spectrum—especially those with primary angle closure (PAC) or primary angle-closure glaucoma (PACG)—and for the fellow eye after an acute attack. The procedure often widens the angle in these eyes and is considered relatively safe when performed by an experienced surgeon.5
For people who are only “angle-closure suspects” (narrow angles but normal pressure and no optic nerve damage), the decision is individualized. Large randomized studies suggest that while LPI modestly lowers the risk of progression, the overall absolute risk is low for many suspects—so careful observation may also be reasonable after a discussion of risks, benefits, and your preferences.6
Good candidates can attend follow-up visits, understand warning signs, and have angles where pupillary block is a key driver. Not ideal candidates include people with active eye inflammation, uncontrolled infection, or eyes in which a different mechanism (such as plateau iris or extensive scarring) is dominant—these cases may need added procedures or surgery. Your doctor will review your medications, general health, and any prior eye surgeries, then explain expected benefits for your eye.
Is Laser Peripheral Iridotomy (LPI) Right for Me?
Select your details to estimate suitability.
Cost and Price
LPI is a medically necessary outpatient procedure and is generally covered by Medicare Part B and many private insurers when indicated. Costs include professional fees (the physician’s service) and, in some settings, a facility fee (clinic, hospital outpatient department, or ambulatory surgery center). Your exact out-of-pocket cost depends on your plan, deductible, coinsurance, and whether the surgeon and facility are in-network.7
Under Original Medicare, covered outpatient services usually require you to meet the Part B deductible and then pay 20% coinsurance of the Medicare-approved amount. Drugs or supplies used during the visit may be billed under the same benefit. If you have a Medicare Supplement plan or secondary insurance, it may cover some or all of that coinsurance. Ask the clinic for an estimate in advance and whether prior authorization or a referral is needed based on your policy.8
Tips to prepare:
- Bring your insurance cards and list of medicines.
- Arrange for a driver if your vision might be blurry after the visit.
- Clarify any potential facility fees, co-pays, or separate charges for pressure checks the same day.
Benefits and Limitations
Benefits: LPI addresses the root cause of pupillary block by equalizing pressure on both sides of the iris. In appropriately selected eyes, it widens the drainage angle, reduces the chance of another acute attack, and can lower the need for emergency visits. Evidence from clinical studies and expert guidance shows LPI is effective in relieving pupillary block and stabilizing the angle in many patients.9
Limitations and risks: Some eyes remain narrow after LPI because a different mechanism, like plateau iris, is present. In those cases, additional laser (iridoplasty) or surgery may be discussed. Short-term effects can include light sensitivity, mild eye redness, a small amount of bleeding from the iris, and temporary pressure spikes that are treated with drops. A small number of people notice glare, lines, or “ghost images,” especially if the opening is not fully covered by the upper lid; your surgeon can adjust the opening’s location to reduce this. Rarely, changes in corneal endothelial cell counts or other complications have been reported; your eye team will monitor you at follow-up visits.10
It is important to remember that LPI is one tool among several for angle-closure disease. If there is established optic nerve damage or very high pressure, additional treatments—like pressure-lowering drops, laser to the ciliary body in special cases, or lens extraction—may still be needed to protect vision. Your doctor will explain how LPI fits into your overall plan.
Recovery and Long-Term Care
Most people go home right after LPI and can resume light activities the same day. Your team may check eye pressure within one to two hours after the laser and again at follow-up visits. Anti-inflammatory drops are usually used for a few days, and you should avoid rubbing the eye. It’s normal to have mild light sensitivity, tearing, or a scratchy feeling that fades over a day or two.11
Call your ophthalmologist right away for severe pain, a sudden drop in vision, many new floaters, flashes of light, or increasing redness—these can be warning signs that need urgent care. Even after a successful LPI, the drainage angle may remain narrow or can narrow again over time, so regular checkups are important. Your doctor may repeat gonioscopy, confirm that the iridotomy is open, and use imaging to track the angle, especially if you have plateau iris or a thick natural lens that continues to crowd the angle.12
Everyday tips: Keep all follow-up appointments, carry a list of your eye medicines, and tell other health professionals that you have narrow angles so they can avoid risky dilating drops without clearing it with your eye doctor.
Latest Research & Innovations
Modern research helps match treatment to the person. Studies using gonioscopy and imaging show that eyes with persistent angle narrowing after LPI have a higher chance of progressing, which alerts doctors to keep a closer watch on those patients and consider additional procedures when needed.13
Another important trend is earlier consideration of lens surgery in specific cases. In some patients with established primary angle closure or angle-closure glaucoma, removing the natural lens can deepen the front of the eye, open the angle, improve quality of life, and control pressure better than LPI plus drops alone. Your surgeon will discuss whether lens extraction, LPI, or a combination is best for your eye’s structure, pressure goals, and lifestyle.14
Innovation also includes small refinements: improved contact lenses for the laser, energy settings tailored to iris color, and better ways to image the angle during follow-up. These advances aim to make the procedure safer, the opening more stable, and the results easier to monitor over time.
Recent Peer-Reviewed Research
Reverse Pupillary Block after Implantation of a Sutureless Scleral Fixation Carlevale Intraocular Lens.
Sánchez-Vela L, García-Arumí Fusté C, Castany-Aregall M, et al.
COVID-19 Pandemic and Rates of Common Ophthalmic Procedures Among Medicare Beneficiaries.
Mahmoudzadeh R, Samuel M, Wheeler S, et al.
Changes in IOL power after laser peripheral iridotomy based on multivariate analysis.
Wang X, Xue S, Yu Z, et al.
Next Steps
If you’ve been told you have narrow angles, PAC, or PACG—or if you’ve had symptoms of an acute attack—don’t wait. Schedule a visit with an eye specialist. The most appropriate clinician is a board-certified ophthalmologist (ideally a glaucoma specialist). Kerbside can also connect you with the right specialist for a medical education consult (this is not a physician-patient relationship).15
Seek emergency care right away for sudden eye pain, headache, halos, nausea, vomiting, or sudden blurred vision, since these can be signs of acute angle-closure glaucoma. Early treatment protects vision and can prevent permanent damage to the optic nerve.16
Remember: education is powerful, but only an in-person exam can confirm your exact diagnosis and best treatment plan. Bring your glasses, a list of medicines, and any prior eye records to your appointment so the team can see the full picture.
Trusted Specialists
Board-certified providers specializing in Laser Peripheral Iridotomy.


