Micropulse Transscleral Cyclophotocoagulation
Also known as MP-TSCPC
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.


Overview
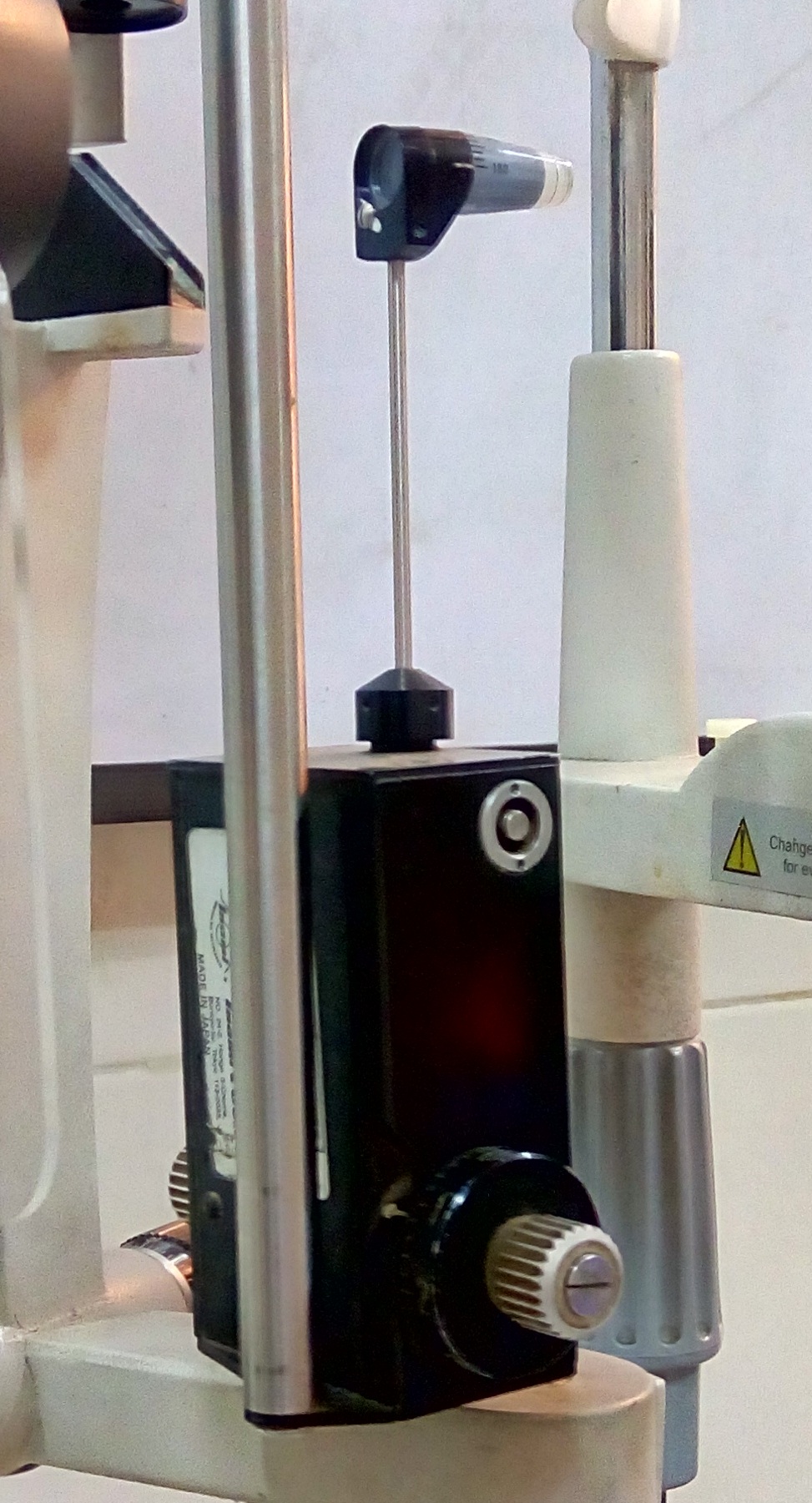
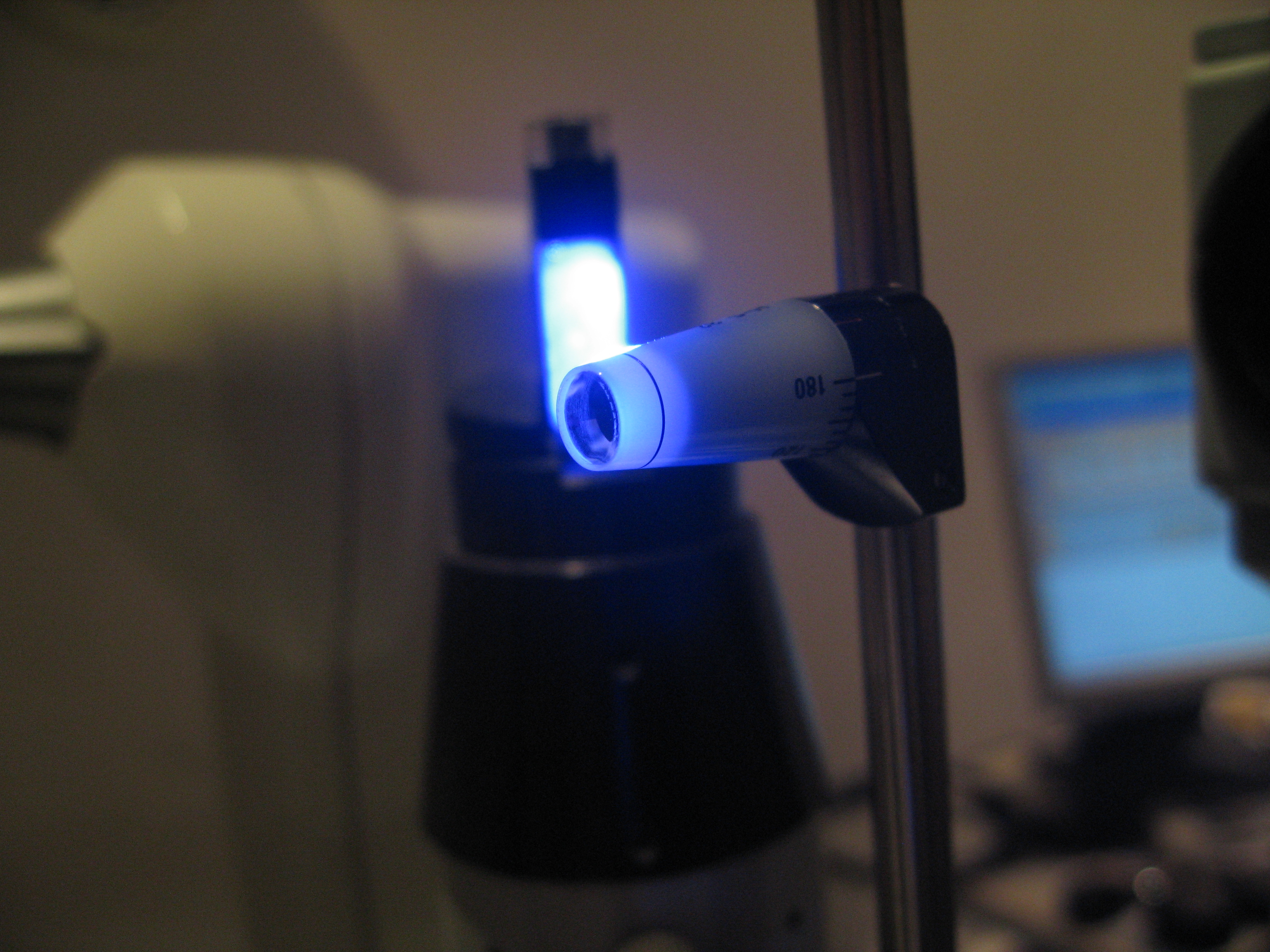
Micropulse transscleral cyclophotocoagulation (MP-TSCPC) is a non-incisional laser procedure for lowering eye pressure (intraocular pressure, or IOP) in glaucoma. A special probe delivers very short bursts of 810-nm diode laser energy through the white of the eye (sclera) to the ciliary body, the tissue that makes aqueous fluid. The laser turns on and off rapidly (micropulses), allowing heat to dissipate between pulses and aiming to reduce fluid production with less tissue damage than older continuous-wave treatments.1
In studies across many glaucoma types, MP-TSCPC has been shown to lower IOP and reduce the number of pressure-lowering drops for many patients, with a safety profile that is generally more favorable than continuous-wave (traditional) transscleral cyclophotocoagulation (CW-TSCPC).2
Glaucoma is a group of diseases that damage the optic nerve, often related to high IOP. Lowering IOP is the only proven treatment to slow or prevent vision loss. MP-TSCPC offers an option when drops and prior lasers or surgeries are not enough—or when patients and doctors wish to consider a less invasive step before incisional surgery.
How the Procedure Works & Options
Step by step: MP-TSCPC is usually done in an outpatient setting with numbing and a nerve block around the eye to keep it comfortable. The probe is placed on the sclera, typically sweeping around 180°–360° of the limbus while avoiding the 3 and 9 o’clock positions to protect nerves and vessels. Common settings include a 31.3% duty cycle (0.5 ms “on,” 1.1 ms “off”) and power near 2000 mW, though parameters vary by surgeon and case. Total treatment time often ranges from about 100 to 360 seconds per session.3
Because energy is delivered in pulses, the approach aims to minimize collateral damage compared to continuous energy delivery.
Where it fits among options: Glaucoma care is customized. Depending on the type and severity of disease, choices may include:
- Medicines
- Laser trabeculoplasty
- Minimally invasive glaucoma surgery (MIGS)
- Trabeculectomy or tube shunt surgery
- Lens/cataract surgery in select angle-closure mechanisms
MP-TSCPC can be considered before or after incisional surgery, and the treatment may be repeated if needed after follow-up evaluation.4
Who Is a Candidate?
MP-TSCPC has most often been used in eyes with refractory glaucoma—cases that remain above target IOP despite drops, prior laser, and sometimes even surgery. Unlike older continuous-wave cyclophotocoagulation that was commonly reserved for eyes with very poor vision, MP-TSCPC may be considered in seeing eyes and across many glaucoma subtypes (primary open-angle, pseudoexfoliation, normal-tension, uveitic, neovascular, chronic angle-closure, and more).5
It has also been used in eyes that already have filtering blebs or tubes, and in patients who want to avoid or delay incisional surgery.
Consensus guidance suggests matching energy and sweep technique to disease severity, and underscores careful selection in eyes with active inflammation or very thin conjunctiva at the probe path. Many centers consider MP-TSCPC in mild to advanced glaucoma when medical therapy is insufficient or poorly tolerated, with discussion of benefits, risks, and the possibility of retreatment.6
MP-TSCPC Educational Suitability Estimator
Select your details to estimate suitability.
Cost and Price
Costs vary by location and setting (clinic, ambulatory surgery center, or hospital outpatient department). Typical components include:
- Physician service
- Facility fee (if applicable)
- Anesthesia
- Follow-up visits
In the U.S., medically necessary outpatient procedures are generally covered under Medicare Part B and many commercial plans, but deductibles, co-insurance, and copays may apply. Always confirm coverage and any prior authorization needs with your insurer before treatment.7
When performed in a hospital outpatient department, the visit is typically billed under the Part B outpatient hospital benefit. Your out-of-pocket responsibility depends on your specific plan, whether the providers and facility are in-network, and if you carry Medigap or secondary coverage to offset co-insurance.8
Benefits and Limitations
Benefits you can expect: Most studies show meaningful IOP reduction and, in many patients, fewer glaucoma drops after MP-TSCPC. A 2023 systematic review and meta-analysis found that micropulse treatment lowered IOP up to 12 months and was associated with fewer adverse events (such as hypotony and prolonged inflammation) than continuous-wave cyclophotocoagulation.9 Because the laser energy is delivered in pulses with rest periods, the goal is to achieve pressure control while limiting collateral tissue damage, making it a potential option earlier in the care pathway for the right eyes.
Limitations & risks: Results vary. Some eyes need retreatment or still require drops. Short-term effects can include soreness, light sensitivity, transient IOP spikes, and mild inflammation; rare complications include persistent inflammation, hypotony, choroidal detachment, or vision loss. Technique and energy settings are not yet fully standardized, and surgeons adapt parameters to each patient’s disease and anatomy.10
Recovery and Long-Term Care
Right after the procedure: You can usually go home the same day. Your eye may feel tender or gritty for a day or two. A short course of steroid drops (often prednisolone acetate 1%) with or without a nonsteroidal anti-inflammatory drop is commonly prescribed; some surgeons also add a cycloplegic drop for comfort. Your team will decide when to taper medicines and whether to adjust your glaucoma drops based on your IOP at follow-ups.11
Follow-up: Expect pressure checks within the first weeks and repeat visits over the next few months. Because protocols differ, your surgeon will set visit timing and decide if a touch-up treatment is appropriate. Reviews emphasize that dosing (power, duty cycle, sweep speed, and arc treated) and postoperative care are individualized, and that careful monitoring helps balance efficacy and safety over time.12
Latest Research & Innovations
Durability: Five-year follow-up data from a large European center suggest that standardized MP-TSCPC can provide sustained IOP reduction for many eyes with primary or secondary glaucoma, including those with prior surgeries, with an acceptable long-term safety profile.13 Investigators also report that outcomes relate to energy delivery and patient factors, motivating ongoing work on optimized settings and patient selection.
Refined dosimetry & technique: Recent studies in Ophthalmology Glaucoma explore revised probe designs and dosing algorithms to improve consistency, comparing higher vs. lower energy regimens and mapping sweep speeds to target energy per arc. These efforts aim to maintain efficacy while minimizing inflammation and other adverse events, supporting broader use across disease stages.14
Recent Peer-Reviewed Research
Inflammation and patient satisfaction in micropulse versus continuous wave transscleral cyclophotocoagulation.
Keidel LF, Eckardt F, Nobl M, et al.
Micropulse Transscleral Cyclophotocoagulation in Non-Incisional Eyes with Ocular Hypertension and Primary Open-Angle Glaucoma.
Murtaza F, Kaba Q, Somani S, et al.
Micropulse transscleral cyclophotocoagulation (MP-CPC): efficacy endpoints for the treatment of refractory paediatric glaucoma - a retrospective case-series.
Balbaid N, AlJodai M, Fairaq G, et al.
Next Steps
If your pressures are not at goal—or if drops cause side effects—ask for a comprehensive review of options with a glaucoma specialist (ophthalmologist). You can use the American Academy of Ophthalmology’s directory to find an eye M.D. by location and subspecialty.15 Bring a list of your medications, allergies, prior laser or surgery dates, and your target IOP so your care team can tailor a plan that fits your life and vision goals.
Urgent warning signs: sudden severe eye pain, halos, headache, nausea, or a fast drop in vision can be emergencies—seek immediate care or head to an emergency department.16 Kerbside can also connect you with the right specialist for a medical education consult (this is not a physician–patient relationship or medical care).