Pigmentary Glaucoma
also known as Pigment Dispersion Glaucoma
Last updated September 4, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.

Overview
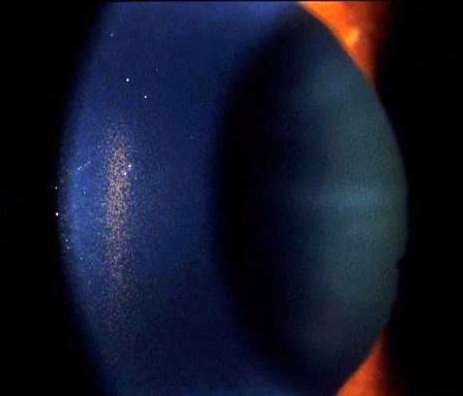
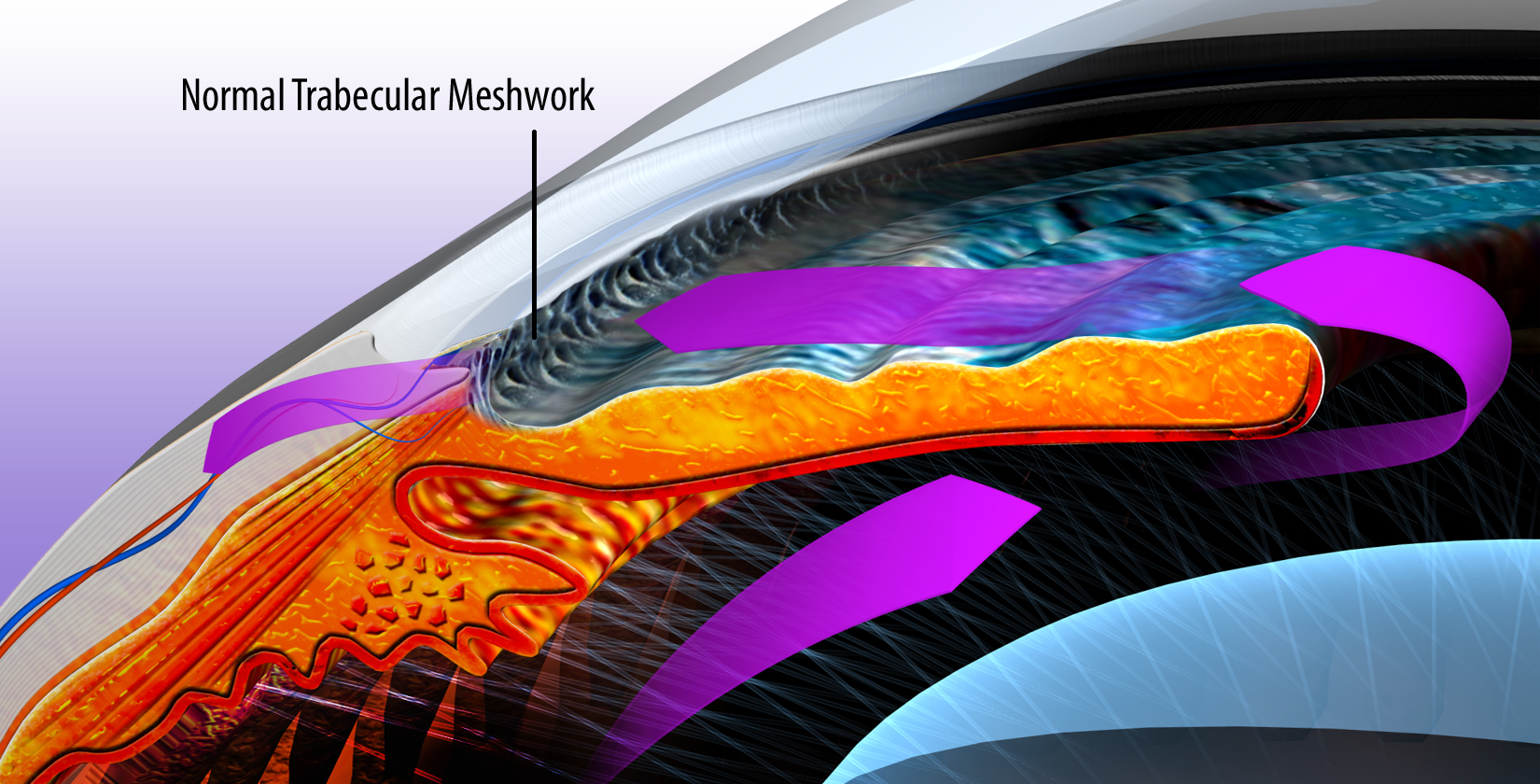
Pigmentary glaucoma (PG) is a form of open-angle glaucoma that occurs when tiny bits of iris pigment rub off and clog the eye’s drain (trabecular meshwork). This can raise eye pressure and damage the optic nerve over time. It often begins as pigment dispersion syndrome (PDS), where pigment floats and deposits inside the front of the eye. Over time, some people progress to glaucoma.
Doctors look for a classic triad:
- Pigment on the cornea (Krukenberg spindle)
- Heavy angle pigmentation
- Spoke-like iris transillumination defects 1
PG is considered a secondary open-angle glaucoma (the drainage angle is open but not functioning properly). Regular eye exams are crucial because early PG is painless and vision seems normal until side vision is affected. 3
Symptoms
Most people have no symptoms initially. As pigment releases (e.g., after exercise), some may notice brief blurry vision or halos. Over time, untreated glaucoma can cause gradual loss of peripheral (side) vision.
Important notes:
- Symptoms are often subtle, so many cases are only found during routine eye exams.
- Testing usually includes pressure checks, optic nerve evaluation, and visual field testing. 2
Causes and Risk Factors
In PDS/PG, the back surface of the iris may bow backward and rub against the lens’ tiny fibers (zonules). This friction sheds pigment, which can clog the drain and cause spikes in eye pressure.
Risk factors include:
- Age & sex: Typically diagnosed in younger adults; men are more often affected in later glaucoma stages.
- Myopia (nearsightedness): Very common in PDS/PG.
- Exercise triggers: Jarring or vigorous activity can release pigment and temporarily raise pressure.
- Family history: Having relatives with glaucoma or PDS/PG increases risk.
Certain treatments (e.g., pilocarpine or laser iridotomy) can sometimes flatten iris shape, reducing rubbing in some cases. 5 Key exam clues include the triad of findings described above. 1
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
Diagnosis is made by an eye doctor after a comprehensive eye exam.
Typical steps include:
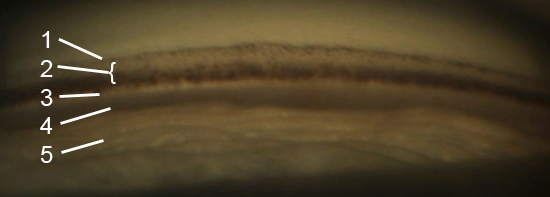
- Slit-lamp exam to check for corneal pigment (Krukenberg spindle) and iris transillumination defects.
- Gonioscopy to examine the drainage angle for heavy, even pigment.
- IOP checks, sometimes before and after exercise or dilation.
- OCT imaging of the optic nerve and retinal nerve fiber layer.
- Visual field testing to map changes in peripheral vision.
Other conditions like pseudoexfoliation and uveitis must be ruled out. 8 The AAO EyeWiki provides detailed descriptions of these findings. 1
Treatment and Management
The goal is to protect the optic nerve by lowering eye pressure to a safe target set by your doctor.
Options include:
- Prescription eye drops: Common types include prostaglandin analogs, beta-blockers, alpha-agonists, and carbonic anhydrase inhibitors. Pilocarpine may also be used to reduce iris–zonule rubbing in some cases.
- Selective Laser Trabeculoplasty (SLT): A clinic laser that improves drainage and may reduce or replace drops. Frequently considered for PG. 6
- Laser Peripheral Iridotomy (LPI): Creates a tiny opening in the iris to improve fluid flow and flatten a concave iris. A major trial found no long-term benefit for most PDS cases, so it's used selectively. 4
- Surgery: If glaucoma worsens, options include trabeculectomy or drainage implants.
Cost & practical tips:
- Ask about generic drops, 90-day supplies, and prior authorization to reduce costs.
- SLT is usually billed as an outpatient procedure—request a pre-estimate including facility and doctor fees.
- LPI is typically covered if medically necessary—confirm coverage with your plan.
- For surgery, request bundled estimates and check for in-network providers.
- Manufacturer copay cards and pharmacy discount programs may lower out-of-pocket expenses.
Daily habits: Use drops as prescribed, attend follow-ups, avoid smoking, and discuss how to manage workouts that may cause temporary IOP spikes.
Living with Pigmentary Glaucoma and Prevention
With steady care, most people with PG maintain good vision.
Helpful steps:
- Stick to treatment: Use reminders and bring your drop bottles to appointments.
- Plan workouts: If exercise triggers pressure spikes or blurry vision, discuss timing drops and choosing lower-impact activities. 2
- Protect eyes: Wear protective gear during sports and yardwork.
- Don’t skip checkups: Regular testing (pressure, visual fields, OCT) helps detect changes early. 3
There’s no guaranteed way to prevent PDS/PG, but early diagnosis and consistent pressure control greatly reduce vision loss risk.
Latest Research & Developments
Iris shape and mechanics: Imaging shows a concave iris in PDS that can flatten after treatment, reducing pigment release. 5
Mapping pigment release: Studies explore how pigment deposits form, such as Scheie stripes or Zentmayer rings, to improve diagnosis and monitoring. 9
Research continues on SLT vs. drops, selective LPI use, and how exercise or pupil changes affect short-term IOP spikes. 6
Recently Published in Peer-Reviewed Journals
Ophthalmology. Glaucoma
July 26, 2025
Selective Laser Trabeculoplasty and the Evolving Glaucoma Paradigm.
Realini T, Gazzard G
Ophthalmology
May 9, 2025
Randomized Noninferiority Trial of Direct Selective Laser Trabeculoplasty in Open-Angle Glaucoma and Ocular Hypertension: GLAUrious Study.
Gazzard G, Congdon N, Azuara-Blanco A, et al.
JAMA ophthalmology
April 1, 2025
Selective Laser Trabeculoplasty After Medical Treatment for Glaucoma or Ocular Hypertension.
Konstantakopoulou E, Gazzard G, Garway-Heath D, et al.
Next Steps
If you suspect or are diagnosed with PDS/PG, see a glaucoma specialist (ophthalmologist).
How to schedule:
- Ask for a "glaucoma evaluation."
- Bring your glasses/contact prescription, medication list, and prior records.
- If your insurance requires a referral, request it early from your primary care provider.
Timing tips: Ask to be added to the cancellation list. If you experience symptoms after exercise or dilation, let the clinic know for a quicker appointment.
Fast guidance: Kerbside offers educational consults to help you prepare for your visit (note: this is for education only and does not establish a physician–patient relationship).


